CHAPTER 17
Raynaud Phenomenon
Patricia A. Lewis
First Edition Authors: Patricia A. Lewis and Sue Monaro
OBJECTIVES
1. Distinguish between primary and secondary Raynaud phenomenon.
2. Identify physical examination findings consistent with Raynaud phenomenon.
3. List medical treatment options for Raynaud phenomenon.
4. Discuss key elements in nursing management of patients with Raynaud phenomenon.
Introduction
In 1862, Maurice Raynaud noticed that some people developed transient digital ischemia when exposed to cold. He attributed this response to an overreaction of the central nervous system (Bakst, Merola, Franks, & Sanchez, 2008; Wigley, 2002). Raynaud phenomenon is now defined as a vasospastic disorder resulting in intermittent digital or body part ischemia. The other vasospastic disorders include acrocyanosis (continuous cyanosis of hands or feet aggravated by cold), pernio or chilblains (pruritic burning lesions affecting skin exposed to cold), and livedo reticularis (semipermanent bluish discoloration of hands and legs that worsens with cold exposure). Attacks of Raynaud’s are characterized by well-demarcated, sudden pale or cyanotic changes of digits, ears, nose, or, rarely, other body parts such as the nipple (Barclay, 2004) or penis (Kropman, 2004) in response to cold or emotional stress. The affected body part often becomes bright red as rewarming and reactive hyperemia occur, resulting in the classic sequential white, blue, then red color changes. However, not all affected individuals will demonstrate this triphasic color sequence; many will have only pallor or cyanosis (Creager & Dzau, 2005).
Primary Raynaud’s occurs without other associated diseases or causes and is also known as Raynaud disease or syndrome. Secondary Raynaud phenomenon has similar symptoms with an associated vasospastic or immunologic disease process (e.g., scleroderma) as the cause of the disorder. The distinction between primary and secondary Raynaud phenomenon is not always clear (Anders, Sigi, & Schattenkirchner, 2001), but generally the vasospasm of primary Raynaud’s is less severe, totally reversible, and does not result in permanent ischemic changes, such as ulceration. However, a small quality of life study on the psychosocial effects of primary Raynaud disease showed a reduction is quality of life and increased anxiety compared to age-matched controls (DeAngelis, Slaffi, & Grassi, 2008). Because secondary Raynaud’s is associated with underlying connective tissue disease, particularly scleroderma, permanent skin changes with ulceration may occur. Studies suggest that between 10% and 30% of patients who have primary disease will eventually be diagnosed with a systemic connective tissue disorder over a period of as long as 20 years (Hodges, 1995), thus making the transition to secondary Raynaud phenomenon (Kahaleh, 2004; Wigley, 2002). Although approximately 15% of patients who have primary disease will improve spontaneously (Craeger & Dzau, 2005), health care providers should be cautious about assuming that primary Raynaud’s remains a relatively benign problem over the course of an individual’s lifetime.
Although true incidence of Raynaud’s is unknown because a standardized definition and testing are lacking and mild cases are underreported, surveys estimate that between 4% and 30% of the general population have symptoms of the phenomenon (Coffman, 1996; Klippel, Crofford, Stone, & Weyand, 2001). More than 50% of patients with symptoms have primary Raynaud’s (Creager & Dzau, 2005). A familial tendency toward the disease has been identified, and females are affected in a ratio of 4:1 over males, with the usual age of onset between the second and fourth decades (Coffman, 1996). One study documented 15% prevalence in children aged 12 to 15 years; prevalence was higher in girls (18%), increased with age, and had no association with psychosocial factors (Jones et al., 2003). Prevalence, as well as frequency and severity of attacks, varies depending on natural environment (increased in a cold, damp climate or in winter) and occupation (especially use of vibrating heavy equipment, such as a jackhammer). “Evidently, any disease, persistent vasoconstrictor stimulus, or constant trauma that causes damage to blood vessels or tissue may lead to one of the vasospastic syndromes, perhaps by the common mechanism of ischemia” (Coffman, 1996).
 I. Anatomy (Refer to Chapter 3, Anatomy and Physiology of the Vascular System, for a complete anatomic description.)
I. Anatomy (Refer to Chapter 3, Anatomy and Physiology of the Vascular System, for a complete anatomic description.)
A. Upper Extremity Digits are More Often Affected (Wigley, 2002).
1. Radial and ulnar arteries are the major suppliers of hand circulation.
a. Multiple intercommunications occur at palmar level.
b. One dorsal and two palmar arches (superficial and deep) provide a variety of inflow pathways to digits (see Fig. 17-1).
c. Superficial palmar arch is usually the dominant arterial circulation to fingers, supplying common digital arteries that branch into proper digital arteries on either side of fingers.
d. Distal circulation of the hand is much more variable than proximal, larger vessels of upper extremities.
2. In addition to capillary circulation, human digits contain multiple arteriovenous anastomoses, connecting arterial and venous circulation directly (Coffman, 1996).
a. These bypass the capillary bed.
b. Shunts allow a large blood flow to pass through digits in a warm environment and close when exposed to cold, thus allowing the body to regulate core temperature.
c. They are under control of the sympathetic nervous system by means of alpha receptors.
d. During body cooling, arteriovenous shunts constrict and close, but capillary and nutritional blood flow is normally maintained unless vasospastic disease is present.
3. Attack usually begins in a single digit.
4. Attack spreads to other digits symmetrically in both hands.
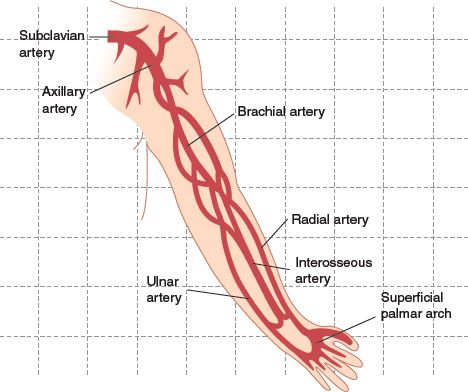
FIGURE 17.1 Anatomy of the major arteries of the upper extremity.
5. Index, middle, and ring fingers are most frequently affected; thumb is usually not involved.
B. Toes are Commonly Involved, but Patients are Less Likely to Complain of Symptoms.
C. Other Affected Sites
1. Ears, nose, face, knees
2. Nipples of breastfeeding mothers (Barclay, 2004)
a. Involves painful breastfeeding with symptoms brought on by cold exposure.
b. Nipple blanching is followed by cyanosis and/or erythema.
c. Symptoms may also be present during pregnancy.
d. Attack is treatable (refer to Medical Management); does not result in permanent damage.
3. Penis (Kropman, 2004)
 II. Pathology and Pathophysiology
II. Pathology and Pathophysiology
A. Primary Raynaud Disease
1. Pathology
a. Mild (early) diseased limited data; no tissue abnormalities noted (Coffman, 1996).
b. Severe diseased intimal hyperplasia, narrowing or total occlusion of digital arteries, thrombi, possible cellular or basement membrane changes; conflicting reports of abnormalities in digital arteries seen on arteriograms: some show stenoses/occlusions; others are normal (Coffman, 1996).
2. Pathophysiology
a. Normal physiology: digital flow depends on pressure gradient across vessel, and resistance is determined by blood viscosity and vessel radius.
1) Blood flow in vascular bed is regulated by central nervous system via sympathetic system; hypothalamus controls arteriovenous anastomoses to regulate body temperature; emotional response is also related to hypothalamus activity.
2) Messages from cerebral cortex are passed to vasomotor centers in medulla to stimulate either pressor or depressor activity.
3) Baroreceptors, chemoreceptors, and somatic afferent nerves also affect activity of vasomotor center. Messages are sent from medulla to sympathetic ganglia and then to sympathetic nerves.
4) Sympathetic activity regulates vessel smooth muscle tone and vessel wall thickness, changing the radius.
5) Increased sympathetic stimulation (stress) or cold causes secretion of norepinephrine, which stimulates alpha-adrenoreceptors and leads to vasoconstriction, with closure of arteriovenous shunts as already described.
6) Serotonin receptors are also present in hand, which have similar activity but are independent of alpha receptors. Stimulation of serotonin receptors causes vasoconstriction.
b. Abnormal/pathophysiology: primary Raynaud’s is associated with an extreme alpha-2 response to cold exposure, but cause is unknown.
1) Three physiology alterations are identified
a) Sympathetic nervous system
b) Adrenoreceptor number and function
c) Naturally occurring vasoactive peptides
2) Triggers (cold and stress) induce an abnormally forceful contraction of arterial wall smooth muscle.
3) Total finger and capillary flow is decreased in patients with primary Raynaud’s in both warm and cool environments (Coffman, 1996).
4) Patients who have primary Raynaud’s have lower brachial and finger systolic blood pressure and fingertip perfusion pressure than normal subjects, but not all individuals who have low systolic pressure have vasospastic attacks.
5) Increased number of peripheral alpha-receptors augments vasoconstriction; at the same time, decrease in beta and calcitonin receptors limits normal vasodilatation capacity (Hodges, 1995).
6) Hard red blood cells, increased plasma viscosity, and decreased fibrinolysis contribute to increased vascular resistance and sluggish microcirculatory blood flow (Hodges, 1995).
7) Endothelin, a potent vasoconstrictor, is elevated, whereas endothelium-derived relaxation factor (EDRF), a vasodilator, is decreased (Hodges, 1995).
8) Central nervous system pathology is suggested by decreased baseline microvascular flow and increased systemic levels of norepinephrine (Hodges, 1995).
9) The “local fault” theory was proposed by Sir Thomas Lewis, 1930: abnormality exists at digital artery level; local cooling produces ischemic attacks in a single finger, even with a sympathetic block (Wigley, 2002).
10) Raynaud’s “sympathetic overactivity” theory posits an exaggerated response of digital blood flow to body position and stress as well as to cold, implicating more of a sympathetic reaction than a local reaction. This theory is supported by positive response of some patients to the use of alpha-adrenergic blockers or sympathectomy. However, sympathectomy does not consistently provide relief, and sympathetic overactivity should alter blood and urine catecholamines, but these changes have not been demonstrated (Coffman, 1996).
11) Theory of generalized functional abnormality of vascular smooth muscle rests on close correlation of primary Raynaud symptoms to other vasospastic disorders, especially migraine headache, as well as to pulmonary, renal, and macular capillary vasospasm (Coffman, 1996).
B. Secondary Raynaud Phenomenon
1. Decreased blood flow and blood pressure in digits are due to atherosclerotic, vinyl chloride, or connective tissue diseases.
a. Underlying disease disrupts normal mechanisms of vessel reactivity.
b. Example: scleroderma involves intimal fibrosis and endothelial dysfunction; endothelial cell damage is associated with increased platelet adhesion, decreased storage of von Willebrand factor, and decreased adenosine uptake. Cold- or stress-induced vasospasm similar to Raynaud response is also documented in other circulatory beds (gastrointestinal, coronary, placental, and genitourinary) in these patients.
c. Reperfusion injury follows ischemia, leading to altered smooth muscle receptor expression and vascular function (Wigley, 2002).
2. Hyperviscosity related to blood abnormalities (e.g., cryoglobulinemia) also leads to reduced flow state.
3. Persistent vasoconstriction is secondary to drug therapy or sympathetic nerve damage related to thoracic outlet syndrome (refer to Chapter 18, Thoracic Outlet Syndrome).
4. Vibration injury: degeneration of sensory vibration receptors produces reflex vasoconstriction by means of alpha-receptor activity; centrally mediated sympathetic hyperactivity is also increased with vibration (Hodges, 1995).
5. End-stage renal disease: Raynaud phenomenon related to endothelial dysfunction, rather than AV shunt steal syndrome, is responsible for symptoms in hemodialysis patients (Czupryniak et al., 2005).
C. Triphasic Color Change (white to blue to red) Episode.
Cold exposure/emotional stress
↓
Vasospasm of palmar and digital arteries/arterioles
↓
Cessation of capillary perfusion
↓
Pallor
↓
Reflexive dilatation of capillaries and venules from regional hypoxia and byproducts of anaerobic metabolism
↓
Slight relaxation of arterial spasm
↓
Blood flow into dilated capillary bed
↓
Desaturation
↓
Cyanosis
↓
Increased amounts of blood entering dilated capillaries
↓
Rubor
↓
Relaxation of arterial spasm
↓
Return of normal blood flow
↓
Capillary perfusion
 III. Causation and Precipitating Factors
III. Causation and Precipitating Factors
A. Primary Raynaud Disease
1. Causation is idiopathic and possibly genetic. Genome-wide screen among families with disease has tentatively identified five genetic loci on X chromosome and chromosomes 6, 7, 9, and 17 (Wigley, 2002).
2. Precipitating factors include cold exposure and increased stress.
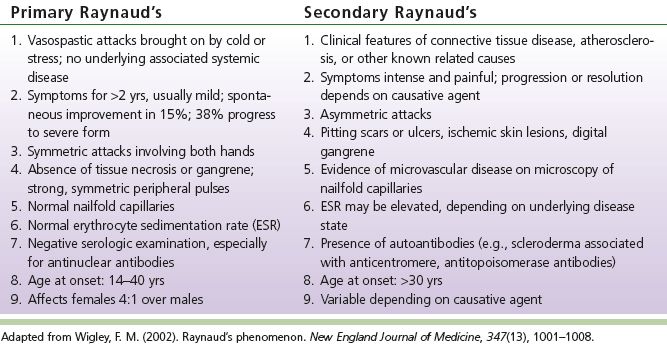
B. Secondary Raynaud Phenomenon (see Table 17-1)
1. Most common causes are drugs and connective tissue disorders.
2. Other causes include atherosclerosis, trauma, increased blood viscosity, compression of nerves/blood vessels, vasculitis.
3. Strong association with autoimmune disorders: most of these conditions have element of distal upper-extremity small artery obstruction.
4. Drugs
a. Beta-adrenergic antagonists, both nonselective and cardioselective
1) Affect males and females; all ages affected equally
2) No relationship to dose
3) Incidence: 4% to 40% of patients using these drugs (Coffman, 1996)
4) Substitution with alpha-adrenergic blockers does not always alleviate symptoms.
5) Exact mechanism of effect unknown; may be due to unopposed alpha-adrenergic vasoconstriction, reduced blood pressure and cardiac output with reflexive vasoconstriction, or central cardiovascular vasoconstriction effect.
b. Ergot derivatives
1) Produce intense vasospasm by stimulation of alpha-adrenoceptors.
2) Ergot intoxication leads to proliferation of endothelium, thrombosis, hyaline degeneration, and fibrosis of the vascular wall.
3) Vasospasm occurs with ingestion of more than 10 mg/week.
4) Females are affected more than males.
5) Incidence of toxicity is 0.01%.
6) Large and small vessels are involved: digital, carotid, axillary, renal, coronary, ophthalmic, and splanchnic circulation.
7) Symptoms include painful, cold, discolored extremities or intermittent claudication; occasional intense burning pain in extremities (known as St. Anthony’s fire). Large vessel pulses may be palpable; gangrene may occur.
8) Arteriographic findings: uniform smooth tapering of large- and medium-sized vessels that disappears at forearm or calf level.
9) Treatment: if patient does not have a limb-threatening condition, bed rest with heparinization for 3 days to allow for resolution of spasm. For severe cases: intra-arterial or intravenous nitroprusside with or without oral nifedipine.
c. Chemotherapeutics: vinblastine and bleomycin
1) 2.6% to 37% of patients may develop Raynaud’s (Coffman, 1996) with this combination.
2) Symptoms usually appear after 10 months of therapy.
3) It is unknown which drug is the causative agent.
4) Vinblastine causes nephrotoxicity; bleomycin causes skin toxicity.
5) Arteriographic findings: diffuse narrowing of digital arteries or multiple small vessel occlusions
6) Attacks may continue even after drugs are discontinued.
d. ADHD medications: methylphenidate and dextroamphetamine—case studies have suggested an association with Raynaud symptoms (Syed & Moore, 2008).
e. Other drugs associated with Raynaud’s include bromocriptine, clonidine, imipramine, amphetamine, cyclosporine; withdrawal from nitroglycerine products. Inconclusive data regarding oral contraceptives (Coffman, 1996).
5. Connective tissue disease
a. Scleroderma/systemic sclerosis: Raynaud’s is the earliest and most common symptom (Kahaleh, 2004).
1) Initial complaint of 50% of patients with scleroderma (Coffman, 1996)
2) 90% of scleroderma patients have Raynaud’s (Klippel et al., 2001)
3) CREST syndrome (limited systemic sclerosis): Calcifications in subcutaneous tissue, Raynaud’s, Esophageal motility abnormalities, Skin thickening or tightness, Telangiectasias
4) Other associated symptoms: sclerodactyly (loss of digital pads on fingertips), digital ulcerations, ischemic demarcation leading to amputation
5) Scleroderma is associated with vascular occlusion caused by fibrosis of intima, platelet activation, stimulation of clotting cascade, and fibrin deposition (see section on Pathophysiology). Walls of small arteries are thickened and trapped in fibrous tissue.
6) “(There is) strong evidence for “systemic” Raynaud phenomenon, a generalized vasospastic disorder involving vasculopathy of the terminal arterial circulation of the lungs, kidneys, and heart” (Klippel et al., 2001).
7) Cause of scleroderma and associated Raynaud’s is unknown.
b. Systemic lupus erythematosus (SLE)
1) 10% to 44% of patients have Raynaud’s symptoms.
2) Affects women in third to fourth decade; Blacks more than Whites.
3) Other signs and symptoms: photosensitive rash in butterfly distribution on face, arthralgias or arthritis, seizures, alopecia, pericarditis, nephritis, anemia, leukopenia, thrombocytopenia
4) Pathology: generalized vasculitis affecting both arterioles and venules; fibrinoid necrosis of blood vessels
5) Cause unknown: believed to be autoimmune, but some drugs can induce similar clinical presentation, such as procainamide, isoniazid, hydralazine.
c. Rheumatoid arthritis
1) Focal ischemic lesion and microinfarction
2) Arteriographic findings: occlusion of one or more digital arteries
d. Sjögren syndrome
1) Raynaud’s associated with symptoms of dry eyes and mouth with enlargement of salivary or lacrimal glands
2) Usually associated with rheumatoid arthritis or SLE
6. Trauma and occupational vasospasm
a. Also known as “vibration-induced white fingers”
b. Equipment: pneumatic hammers, chain saws, riveting machines, pounding machines, brush saws
c. Occupations: construction and demolition workers, typists, telephone operators, pianists, meat cutters, sewing machine operators
d. Incidence: 30% to 84% of workers using vibratory tools develop symptoms after 6,000 to 7,000 hours of work (Coffman, 1996).
e. Symptoms: blanching and numbness of fingers; pain and cyanosis rare; feet usually spared; attacks may also be brought on by cold exposure. Attacks lessen with avoidance of equipment use, but sensitivity to cold persists.
f. Pathology: usually normal but may show medial muscular hypertrophy or subintimal fibrosis of digital arteries (Coffman, 1996)
TABLE 17-1 Conditions Associated with Secondary Raynaud Phenomenon
7. Hypothenar hammer syndrome
a. Use of palm of hand as a hammer or during karate exercise, bowling, or pushing a walker may cause ulnar artery occlusion.
b. Patient develops Raynaud symptoms in only one hand.
1) Pallor or cyanosis with numbness on exposure to cold
2) No reactive hyperemia
c. 1.7% of patients with Raynaud’s symptoms; usually affects men in third to fourth decade; calluses over palm suggest diagnosis (Coffman, 1996)
d. Radial and ulnar pulses are usually palpable, normal
e. Allen test: color restored with release of radial artery (refer to Chapter 10, Upper Extremity Arterial Occlusive Disease for complete description)
f. Arteriographic findings: ulnar artery thrombosed, irregular, or aneurismal at level of hamate bone; possible multiple digital artery occlusions caused by emboli
8. Carpal tunnel syndrome
a. Numbness, burning, tingling of first three fingers of hand; worse at night; pain may radiate to elbow or shoulder; symptoms usually bilateral
b. Raynaud’s symptoms may precede other symptoms by 6 to 12 months.
c. Weakness and atrophy of muscles on thenar eminence with sensory complaints below the wrist
d. Symptoms related to compression of median nerve by swelling, inflammation, or infiltration of tissue of the transverse ligament that crosses the ventral surface of wrist
e. Common occupational disease: affects keyboard operators or others who overuse wrist, hand.
9. Thoracic outlet syndrome (refer to Chapter 18, Thoracic Outlet Syndrome)
a. 38.6% of patients who have hyperabduction and 5.3% of those who have other causes of thoracic outlet syndrome have Raynaud’s symptoms (Coffman, 1996).
b. Attacks may affect one or both hands.
c. Attacks are caused by either compression of nerves in thoracic outlet or by distal emboli from thrombi in subclavian artery.
10. Blood dyscrasias (See Table 17-1)
a. Raynaud’s symptoms develop as a result of clumping of red blood cells in small arteries and arterioles.
b. Cryoglobulinemia: patients develop purpura of legs, joint pain, leg ulcers, renal failure; twice as common in females, with symptoms starting in third to fourth decade; may be secondary to infections, autoimmune or connective tissue disease, lymphoproliferative disease, or liver disease.
c. Cold agglutinins: antibodies of -IgM type; Raynaud’s symptoms with or without pallor or cyanosis of entire hand. Affects men aged 30 to 90 years; need not be accompanied by underlying disease but may be associated with viral infection or lymphoma (Coffman, 1996).
11. Atherosclerosis of upper extremities
a. Atherosclerosis of extremities: frequent cause of Raynaud symptoms in men older than 50 years (refer to Chapter 10, Upper Extremity Arterial Occlusive Disease).
b. Arteriosclerosis obliterans: attacks of pallor and cyanosis occur in one or two toes with no reactive hyperemia; only one leg involved; pulses absent and patient has history of intermittent claudication.
c. Thromboangiitis obliterans (Buerger disease): Raynaud’s symptoms in as many as 57%; lower extremities usually affected but upper extremities affected in as many as 70% (Coffman, 1996) (refer to Chapter 16, Buerger Disease).
d. Acute arterial occlusion: Raynaud’s symptoms may follow acute occlusion of proximal large- or medium-sized vessels but should not be confused with embolization to smaller digital vessels, which involves only one or two digits and may lead to ischemic changes.
e. Inflammatory arterial disease/vasculitis: any of the many vasculitides may be associated with Raynaud’s symptoms owing to immune complexes that can induce inflammatory reactions in small arteries.
f. Arteriovenous fistula: more than 50% of patients with fistulas have Raynaud’s symptoms; peripheral coolness and trophic skin changes may develop; in addition to reduced blood flow to digits, other factors are probably involved, because the unaffected hand also develops symptoms with exposure to cold (Coffman, 1996).
12. Other conditions associated with secondary Raynaud’s
a. Polyvinyl chloride disease
1) Occurs in workers who clean autoclaves
2) Results in multisystem disease resembling scleroderma: thickening of skin on hands and arms, nodule formation, thinning of bones, thrombocytopenia, hepatic and pulmonary dysfunction, angiosarcoma of liver
3) Arteriographic findings: stenoses or occlusions of digital arteries
b. Hypothyroidism
1) Incidence may be as high as 24% (Coffman, 1996)
2) Vasoconstriction may be due to decreased production of body heat
c. Primary pulmonary hypertension
1) Incidence of Raynaud’s is 10% to 30% (Coffman, 1996)
2) Marked intimal thickening of pulmonary arterioles while skin and muscle biopsies are normal; no evidence of systemic disease
3) It is theorized that neurohumoral changes affecting both pulmonary and digital circulations cause vasospasm that could lead to permanent damage to small vessels (Creager & Dzau, 2005)
d. Heavy metal: Raynaud’s symptoms have been associated with toxicity from lead, arsenic, thallium, and mercury.
e. Neoplasms
1) Raynaud phenomenon or digital ischemia has been associated with stomach, kidney, colon, ovarian, breast, cervical, and lung cancers and leukemia.
2) No extrinsic compression from tumor needed for symptoms; no consistent identifiable causative relationship.
3) Raynaud’s symptoms preceded diagnosis of tumor in 63 of 180 patients by an average of 9 years (Coffman, 1996).
f. Drug-induced: ADHD medications and renal clearance.
 IV. Assessment
IV. Assessment
A. Assess for Risk Factors
1. Primary Raynaud disease: family history. As mentioned earlier, this idiopathic condition may have a genetic link; despite longstanding evidence for familial patterns, further longitudinal studies are needed (Kahaleh, 2004; Wigley, 2002).
2. Secondary Raynaud phenomenon
a. Risk associated with cause
b. Drugs: use of ergot derivatives, methysergide, excessive caffeine, beta blockers, ADHD medications, hemotherapeutics as listed
c. Connective tissue disorders
1) “One of the most difficult clinical challenges faced when evaluating patients with Raynaud phenomenon is the assessment of risk for transition to connective tissue disease” (Kahaleh, 2004).
2) 10% to 30% conversion from primary Raynaud disease to secondary Raynaud phenomenon occurs over 20 years (Hodges, 1995).
d. Trauma (see causes listed earlier)
1) Occupational hazards: use of vibratory tools, jackhammers, or chain saws; use of electrical wires; chronic exposure to cold; professional sports injuries; injuries from strenuous use of upper extremities in certain professions (e.g., commercial fishermen, lumberjacks, masons, farmers, meat cutters)
2) Frostbite
3) Recreational injuries from sports such as bowling, baseball, karate
4) Any limb trauma resulting in reflex sympathetic dystrophy, thoracic outlet syndrome, or carpal tunnel syndrome; use of hand as a hammer
e. Risk factors associated with atherosclerosis
1) Smoking
2) Hypertension
3) Hyperlipidemia
4) Advancing age
5) Male gender
6) Family history, including aneurysmal disease
7) Medical history of coronary artery disease, stroke, renal failure, diabetes mellitus
f. Medical conditions as listed earlier
g. Risks associated with other occupations: typists, pianists, sewing machine operators, workers who clean autoclaves (vinyl chloride exposure), workers who are exposed to heavy metal
B. Patient History
1. Subjective
a. Triphasic color changes of digits with exposure to cold or stressful situations.
1) Classic symptoms may or may not be present.
2) Onset is sudden with sharp demarcation of color changes; pallor/ischemic changes last 15 to 20 minutes.
3) Patient reports sensitivity to cold: avoids shopping in frozen food section of store or air conditioning; winter activities worsen complaints.
4) Involvement is usually bilateral and symmetric but may be unilateral, depending on cause.
5) General body chill may provoke attack.
6) Upper extremity complaints include tips of fingers distal to metacarpophalangeal joint and thumb.
7) Initially, only one or two digits are involved; condition progresses to other digits over time. Index, middle, and ring finger are most frequently involved (Wigley, 2002).
8) Fewer than 50% also have attacks in toes (Coffman, 1996).
9) Other areas of involvement include nose, ears, lips, face, chest, and nipples during breastfeeding.
b. Symptoms of low blood flow: sensation of pins and needles, numbness, clumsiness of hands, finger aching
c. Age at onset: primary disease symptoms reported in younger years; secondary phenomenon usually reported in third decade and later.
d. Trophic skin changes: thickening of skin, pitting scars, chronic paronychia, fissuring of fingers, ulcerations, digital gangrene
e. Symptoms of associated disorders as listed earlier: thorough review of systems required.
1) Constitutional: fatigue, fevers, night sweats, weight changes
2) Skin: changes as listed earlier; rashes, telangiectasias, jaundice, hyper- or hypopigmentation
3) HEENT (Head, Ears, Eyes, Nose Throat): headache, vision change, dry eyes or mouth, oral ulcers
4) Respiratory: cough, exertional dyspnea, wheezing, frequent infections
5) Cardiovascular: chest pain/pressure, palpitations, limb swelling, claudication, rest pain
6) Gastrointestinal: appetite, dysphagia, abdominal pain, change in color or caliber of stools
7) Genitourinary: painful breastfeeding, vaginal dryness, erectile dysfunction, frequency, miscarriage
8) Musculoskeletal: painful, swollen joints; limitation of range of motion; muscular atrophy, especially of thenar eminence
9) Endocrine: intolerance to heat/cold, excessive thirst, urinary frequency
10) Hematologic: easy bruisability, petechiae, history of blood clots
11) Neurologic: numbness, tremor, seizure activity, symptoms of stroke, bilateral or unilateral weakness, changes in sensation
12) Psychiatric: anxiety, depression, panic attack, psychosis
2. Objective
a. Primary disease: physical examination is normal except for cool digits.
1) Triphasic color changes may be observed with cold exposure, nervousness, or startle reaction; completely reversed with rewarming.
2) Radial, ulnar, dorsalis pedis, posterior tibial pulses are palpable.
3) Livedo reticularis: mottling of skin of arms and legs during cold response; reversible with rewarming
b. Secondary phenomenon: wide variety of findings depend on causative agent.
1) Temperature and color changes as previously described
2) Trophic skin changes: skin thickening, fissuring, digital ulcerations or gangrene
3) Other signs of connective tissue disease: digital skin binding, dry eyes and mouth with or without oral ulcers, inflammatory joint changes, skin rash, alopecia, sclerodactyly, telangiectasia, xerostomia
4) Signs of atherosclerosis: hairlessness, decreased pulses
5) Evidence or history of trauma
6) Presence of dialysis fistula
7) Positive Allen test (assessment of palmar arch patency) or Adson maneuver (assessment of thoracic outlet)
3. Medical history, including medical or surgical conditions and medication use to identify secondary causes as listed
4. Social history, including occupation, tobacco and drug use, diet and caffeine consumption, recreational activities
5. Family history
a. Raynaud disease
b. Connective tissue disease
c. Atherosclerosis
d. Blood dyscrasias
e. Endocrine disorders: thyroid disease, diabetes mellitus
C. Physical Examination
1. Inspection
a. Primary disease: normal skin condition with visible color changes (as described) with exposure to cold or stressful situation.
b. Secondary phenomenon: trophic skin changes with fissures, ulcerations, gangrene; evidence of trauma; presence of fistula; swelling; muscle atrophy of thenar eminence; arthritic or inflammatory joint changes; punctate lesions on fingertips associated with cyanosis indicating microemboli; other signs of systemic disease as previously listed.
2. Palpation
a. Primary disease: normal skin turgor and texture; bilateral cool hands/feet; normal palpable proximal and distal pulses of upper and lower extremities
b. Secondary phenomenon: variable depending on cause; pulses may be diminished or absent; aneurysmal changes of native vessels or hemodialysis fistula (palpable thrill should be present); skin or joint nodules or calcifications may be present
c. Perform Allen test to assess patency of palmar arch: Radial and ulnar arteries are compressed while patient clenches fist to evacuate blood from hand. When hand is opened, the palm appears pale and mottled. In a patient with normally patent palmar arch, release of either the radial or ulnar artery results in prompt reactive hyperemia of the entire palm, with disappearance of pallor and mottling. In the presence of radial artery occlusion, releasing radial artery compression while maintaining occlusion of the ulnar artery results in continued pallor and mottling. Release of the ulnar artery compression restores hand perfusion. With ulnar artery occlusion, color returns to the hand only after release of the radial artery (Bruni, 2004)
d. Perform Adson maneuver to assess for subclavian artery compression at thoracic outlet: With patient sitting erect, palpate radial pulse as patient deeply inhales and turns head strongly to the affected side. If subclavian artery is compressed by this maneuver, radial pulse will weaken or disappear and return as patient resumes original position facing forward (Bruni, 2004)
e. All pulses, including abdominal aorta, should be palpated to assess for presence of other vascular conditions
3. Percussion of chest and abdomen assesses for pulmonary consolidation or hepatic/splenic enlargement
4. Auscultation
a. Primary disease: no bruits will be heard at any level.
b. Secondary phenomenon: assess for presence of bruits at carotid, subclavian, axillary, brachial, renal, iliofemoral.
1) Perform hyperabduction arm maneuver while auscultating subclavian, axillary, and brachial arteries.
2) If dialysis fistula is present, assess for normal hyperdynamic bruit versus blunted flow signal (stenosis) or flow changes associated with aneurysm.
D. Considerations Across the Life Span
1. Children and young adults
a. 15% of children aged 12 to 15 report symptoms of Raynaud disease; percentage is higher in females (18% vs. 12% males) and increases in later teens; no association with psychosocial factors such as economic level and school performance (Jones et al., 2003).
b. Social factors: occupation, recreational activities, and tobacco and drug use are implicated in secondary phenomenon.
c. Raynaud symptoms may be present for as long as 20 years prior to diagnosis of secondary causes, with conversion from primary disease to secondary phenomenon occurring in as many as 10% to 30% of cases (Hodges,1995).
d. Systemic sclerosis (scleroderma) is rare in children; usually diagnosed between ages 35 and 65; frequently accompanied by family history of connective tissue disease (Klippel et al., 2001).
2. Women of childbearing age
a. Increased prevalence in females (4:1 over males); usually diagnosed between ages 20 and 40 years (Coffman, 1996); affects as many as 20% of women of childbearing age (Barclay, 2004).
b. For systemic sclerosis, female predominance most pronounced during mid to late childbearing years, with ratio of females to males 7 to 12:1 (Klippel et al., 2001).
c. Raynaud’s symptoms of skin blanching followed by cyanosis and/or erythema may affect nipples of breastfeeding mothers, causing painful breastfeeding.
1) Associated with exposure to cold
2) Treatment options: prevention or reduction of cold exposure, avoidance of vasoconstrictive medications, use of calcium channel blockers (nifedipine), aerobic exercise, biofeedback, calcium and magnesium supplements, evening primrose oil and fish oil (Barclay, 2004)
3. Elderly
a. Primary disease is unusual in advanced years
b. Assess for multiple secondary causes, especially atherosclerosis or prolonged use of walker
c. Increased risk for injury results from cold exposure, falls
 V. Pertinent Diagnostic Testing
V. Pertinent Diagnostic Testing
A. Laboratory Tests
1. Once Raynaud phenomenon has been diagnosed based on presentation, laboratory evaluation is required to assess for possible secondary cause, especially in
a. Men
b. Women older than 40 years
c. Patients who have associated signs of sclerodactyly, ulcers, gangrene
2. Basic laboratory tests
a. Complete blood count
b. Erythrocyte sedimentation rate (ESR)
c. Antinuclear antibody (ANA)
d. Urinalysis assesses for crystals, sediment, protein
e. Chest radiographs assess for increased pulmonary markings, cardiac enlargement
f. If any of these are abnormal, proceed with more extensive evaluation
3. ESR
a. Measures speed with which red cells settle out of unclotted blood; during acute inflammation, asymmetric plasma proteins (e.g., fibrinogen, immunoglobulins) interact with red cells to cause stacking of cells; stacked cells fall to bottom of tube more quickly than normal cells.
b. Normal value for most laboratory tests is greater than 20 mm/hr. Normally increases with age, pregnancy, anemia, and renal failure; normally decreases in heart failure.
c. Elevation is seen in patients who have inflammatory process, infection, or neoplasia, but nonspecific.
d. Important to obtain baseline at time of diagnosis because disease process may progress over time.
4. ANA
a. Autoantibodies that react with a variety of nuclear antigens, including nucleic acids, histones, and parts of centromeres (Klippel et al., 2001)
b. Normal value reported as titer of dilution of patient’s serum that showed staining with fluorescein on a slide of human tumor cell, as well as pattern of staining.
1) Normal titer greater than 1:40
2) Patterns reported as homogeneous (SLE), speckled (scleroderma), nucleolar, peripheral, or centromere (CREST syndrome)
c. Positive ANA titer usually indicates autoimmune disease but may be present in as many as 5% of healthy people, especially women (Klippel et al., 2001).
1) 95% of patients who have SLE have positive titer.
2) 25% of patients who have primary Raynaud’s have positive ANA, but positive titer also associated with 63-fold increase in incidence of connective tissue disease (Hodges, 1995).
5. Other serum laboratory tests as indicated based on clinical suspicion: rheumatoid factor, lupus anticoagulant, complement levels, specific autoantibodies, hypercoagulopathy evaluation, lipid profile (when atherosclerosis is suspected), total protein (if elevated, obtain serum protein electrophoresis to assess for myeloma)
6. Electrocardiogram
a. Assesses for arrhythmia
b. If arrhythmia new, will need to be evaluated for possible myocardial infarction
7. Echocardiogram assesses for valve disease, cardiac enlargement and chamber function, and presence of thrombus as source of emboli.
8. Hand radiographs assess for subcutaneous calcium deposits (CREST syndrome) and/or prolonged narrowing of bone in distal fingertips.
B. Noninvasive Vascular Tests
1. Digital blood pressure with cold challenge
a. May use blood pressure cuff or strain gauge.
b. Double inlet cuff for local cooling is placed over the proximal phalanx of the test finger.
c. Measure baseline digital artery pressure at rest in reference and test finger at normal ambient temperature and with digital cooling by circulation of water through cuff at 20°C, 15°C, 10°C, and 5°C for 5-minute intervals.
d. Cuff is inflated above systolic level during cooling; pressure is measured after cuff is released following cooling.
e. Results are expressed as the percentage of decrease in the cooled finger’s systolic pressure on reperfusion as compared with pressure in the reference finger.
f. Positive test: decrease in digital blood pressure of more than 20% considered positive for Raynaud’s.
1) Normal small digital pressure drop with decreasing temperature
2) Vasospastic similar to normal until critical temperature is reached; then abrupt arterial closure occurs
3) Obstructive similar to normal except much lower pressure seen at baseline and with cooling
g. If baseline digital pressures are more than 30 mm Hg lower than brachial pressures at baseline, suspect atherosclerotic/stenotic process.
2. Pulse volume recording (PVR)
a. Amplitude of PVR waveform normally decreases in cool environment; increases in warm environment.
b. Primary Raynaud’s: PVR flattens as patient is exposed to cold; restored to normal volume as patient rewarmed.
c. PVRs will be flattened during cooling and rewarming in patients who have atherosclerotic occlusive disease.
3. Duplex ultrasound evaluation of extremity may be indicated for evaluation of secondary causes, especially atherosclerosis, aneurysm, arteriovenous fistula (refer to Chapter 10, Upper Extremity Arterial Occlusive Disease) (Schmidt, Drause, Schicke, & Wernicke, 2008).
C. Invasive Tests—Arteriography
1. Primary Raynaud disease: limited role, as diagnosis is usually established without invasive procedure (Gerhard-Herman & Creager, 2003).
2. Secondary phenomenon
a. Gold standard for evaluation of upper extremity ischemia, trauma, arteritis, or occlusive disease
1) Plaque, occlusions, emboli, aneurysms, traumatic injuries, arteriovenous malformations, and vasospasm are visualized.
2) Arteritis of aortic arch and major vessels shows individual or multiple areas of stenosis with no plaque or ulcerations.
b. Additional techniques used to improve visualization of small digital arteries.
1) Hand warming
2) Intra-arterial injection of vasodilators used to prevent vasospasm, which may occur at time of contrast injection
3) Primary Raynaud disease may be distinguished from secondary Raynaud phenomenon with identification of cause
c. Collagen vascular disease: bilateral distal lesions with no findings of atherosclerotic changes; smooth, string-like arteries with or without segmental lesions; collateral circulation has “corkscrew” appearance (Bruni, 2004).
d. Provides surgeon/interventionist with a map with which to plan intervention, as well as identification of collaterals and distal vessel status.
e. Visualization of aortic arch and branches is important to identification of proximal lesions, aneurysms, and plaque.
f. One may perform maneuvers to evaluate thoracic outlet compression during examination.
g. Transfemoral route is preferred with use of the Seldinger technique.
D. Special Procedures
1. Nailfold capillary microscopy
a. Microscopic visualization of cutaneous capillaries
b. May assist in distinguishing primary Raynaud’s from secondary Raynaud’s associated with connective tissue disorders; primary disease will be normal.
c. Place drop of grade B immersion oil on skin at base of fingernail; view area with stereoscopic microscope or hand-held ophthalmoscope set at 10 to 40 diopters, or with magnifying glass.
d. Normal: capillaries are regularly spaced, hairpin loops.
e. Abnormal: avascular areas with enlarged, deformed capillary loops are associated with scleroderma; disorganized capillaries with avascular areas and hemorrhage present in dermatomyositis and polymyositis.
2. Electromyogram (EMG) assesses for presence of nerve conduction delay in median and ulnar nerves caused by carpal tunnel syndrome or proximal cervical compression.
3. CT scan or MRI/MRA provides imaging of proximal upper extremity arterial circulation for diagnosis of secondary causes of Raynaud’s symptoms.
a. CT scanning: advances in technology (spiral CT, electron beam CT, spin echo) are expanding usage; increasing usefulness in imaging the thoracic outlet and aneurysms.
b. MRA: gives full longitudinal and cross-sectional view of the vasculature; many advances are increasing its use; much less invasive than angiography (Bruni, 2004).
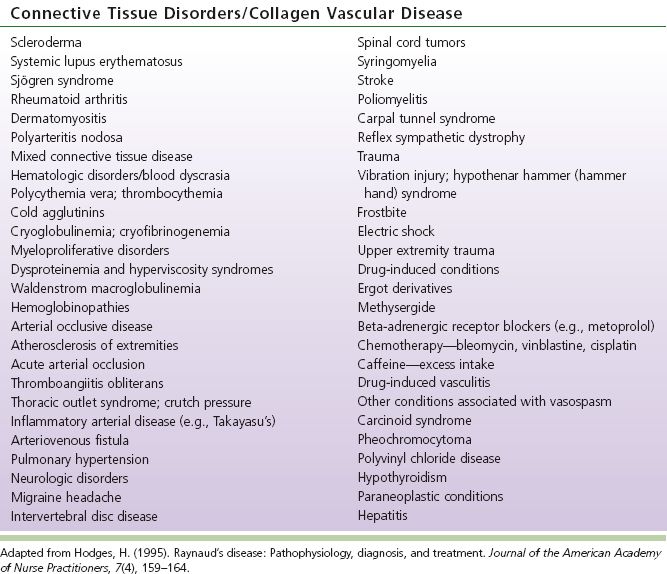
E. Diagnostic Criteria to Distinguish Primary from Secondary Raynaud Phenomenon. Allen/Brown criteria proposed in 1932 for primary Raynaud disease:
1. Vasospastic attacks brought on by cold or emotional stimuli
2. Bilateral extremity involvement
TABLE 17-2 Clinical Features of Raynaud Disease