Melissa LaCour By the end of this chapter, the student should be able to: 1. Discuss the various ways health information is used by a health care facility. 2. Discuss the various ways health information is used by those outside of the health care facility. 3. Understand the intent of various health care regulations and standards. 4. Review health records for documentation of compliance with accreditation standards. 5. Explain how health information is monitored to ensure quality. 6. Explain performance improvement. 7. Identify performance improvement tools. 8. Explain the purpose of various data-gathering tools. 9. Explain how health information is used by specific committees in the health care organization. American College of Surgeons (ACS) benchmarking brainstorming case management certification clinical pathway concurrent review decision matrix granularity graph Healthcare Effectiveness Data and Information Set (HEDIS) Health Care Quality Improvement Program (HCQIP) incidence intensity of service (IS) interdepartmental intradepartmental litigation marketing Medicaid Integrity Contractor (MIC) morbidity rate mortality rate National Integrated Accreditation for Healthcare Organizations (NIAHO) National Patient Safety Goals performance improvement (PI) potentially compensable event (PCE) prevalence qualitative analysis quality assurance (QA) Quality Improvement Organization (QIO) quantitative analysis research retrospective review risk management (RM) severity of illness (SI) survey table tracer methodology utilization review (UR) This text so far has discussed the obvious reason(s) to document health information: patient care. And yet, timely, accurate, and complete health information is essential for many other reasons. This chapter explores the methods used to evaluate and ensure data quality as well as how quality health information is used for reimbursement, litigation, accreditation, marketing, research, education, and performance improvement. Many of the uses of health information have already been discussed in this text. The information that follows may seem repetitious, but an understanding of the many different ways health information is used is essential to HIM professionals. Although each and every use of health data is important, the measurement of quality, discussed in the second part of this chapter, cannot be understated. The uses of health information can be classified as internal to the health care facility or external. Here is a list of some internal health care facility uses: • To support and collect reimbursement • To support and prove compliance for licensing, accreditation, and certification • To support the administration of the facility • To provide evidence in litigation Agencies outside the health care facility (external) use health information for the following reasons: • To study the mortality rates and the prevalence and incidence of morbidity • To develop community awareness of health care issues • To influence national policy on health care issues through legislation • To educate patients and health care professionals The aforementioned uses are the most obvious, but they may not include every possible use of health information. Health information is used to improve the quality of care provided to patients. Many people have been in a health care facility and thought that a few things could have been improved. For instance, did the patient have to wait too long to see the physician? Was communication among the health care professionals inadequate? There may have even been an impression that no one knew exactly what was going on. Historically, health information management (HIM) professionals have reviewed the documentation of patient health care after the patient is discharged to determine whether patients received appropriate care. Review of the patient’s record after discharge is called retrospective review; this method of review analyzes how, when, and where the patient received care. Retrospective reviews provide statistical information to support decisions that will improve care for future patients. Although retrospective reviews can be effective in improving future care, they cannot change or improve the outcome for patients who have already been discharged. The alternative to retrospective review is concurrent review. Concurrent review of patient health information provides timely information that is used to support decisions made while the patient is still in the hospital. Concurrent information provides an opportunity to change or improve the patient’s outcome. This process is discussed in greater detail later in this chapter, in the section about health information in quality activities. Reimbursement refers to the amount of money that the health care facility receives from the party responsible for paying the bill. Health care, although personal in service, has evolved into a large and sometimes very impersonal industry. All health care providers have a vested interest in their financial operations. As with any other business, a health care provider offers a service or product and then charges a fee for that service or product. The provider may obtain reimbursement from for example—the patient, an insurance company, a managed care organization, or the state or federal government. The patient’s health record, which contains documentation of all of the patient’s care, supports the charges for services and supplies. The health record contains documentation of the type of product or service, the date and time at which the service was provided, and the individual who provided the service to the patient. HIM coding personnel review the patient’s health record to identify the correct diagnoses and procedures and then assign the appropriate ICD-10-CM/PCS and HCPCS/CPT codes. These codes are documented on the UB-04 or the CMS-1500 form; they tell the payer why the patient received health care (the diagnosis) and whether any procedures were performed that affect reimbursement. Accurate coding requires a thorough analysis of the complete health record. Inaccurate coding causes the facility to submit false claims for reimbursement. From a compliance perspective, submission of false claims is a crime punishable by law; therefore HIM coders are educated in the review of records and the appropriate assignment of codes for reimbursement. Revenue cycle management (RCM) ensures timely, accurate submission of patient bills for payment. Health care facilities must have a license to operate. Licensure of a health care facility is performed by the state in which the facility is located. Among the many requirements necessary to receive a license, the facility must maintain documentation (a health record) on all patients. As discussed in Chapter 1, health care facilities that provide care to Medicare and Medicaid patients receive reimbursement from the federal government. The Centers for Medicare and Medicaid Services (CMS) oversees the federal responsibilities of the Medicare and Medicaid programs. For a facility to receive reimbursement from the federal government, it must be certified under Medicare’s Conditions of Participation (COP). The COP are the CMS rules and regulations (standards) that govern the Medicare program. Certification under the COP, performed by the state, attests that a health care facility has met the CMS standards. Accreditation is another means by which some health care facilities may be approved to serve state-funded and federally funded patients. Accreditation, like certification, recognizes that a facility has met a predetermined set of standards. However, accreditation is voluntary. Facilities are not mandated to attain accreditation, but they may be motivated by third party payer requirements for reimbursement and the perception that accreditation indicates a certain quality of care necessary to compete in the marketplace. Accreditation is performed by organizations such as TJC, CARF, NIAHO, and the AOA. In some health care settings, a successful survey by TJC and some other accreditation agencies results in assignment of deemed status by the CMS, by which TJC accreditation is accepted in lieu of the Medicare COP certification. What does any of this have to do with health information? Licensure, certification, and accreditation require that a facility prove compliance with regulations or standards. Much of the proof necessary to validate certification and accreditation standards is found in a review of the patient records. The certification or accreditation survey of the records reveals the quality of care delivered to patients within a facility. The survey record review is coordinated to determine whether the facility is providing care within the established guidelines. For example, TJC requires that an operative report be completed immediately after surgery. In cases in which the physician chooses to dictate the operative report, an operative note should be made part of the patient’s chart and should include information pertinent to the operation that a health care professional might need to know in the absence of the detailed operative report. In a check for compliance with this standard, a sample of surgery records would be pulled for review. The surveyor, HIM personnel, or others would review the record to determine the date and time of surgery. The date and time of the surgery are used for comparison with the dates on which the operative report was dictated and transcribed, both of which are indicated on the operative report in Figure 11-1. At the end of the report, the transcriptionist’s initials, the date dictated (DD), and date transcribed (DT) are indicated in the mm/dd/yyyy format shown. This information identifies who the transcriptionist was, when the report was dictated, and when it was transcribed. In an electronic health record (EHR), time stamps are inherent in the process of record entries, including the signature on the dictation. If speech recognition technology is used, the timing of the interaction is also automatically recorded. Administration is the common term used to describe the management of the health care facility. In management of health care, the services that are provided must be evaluated. Managers want to be certain that they are providing health care services in an efficient and effective manner. The administrators responsible for a facility are concerned with personnel and financial and clinical operations of the health care facility. Health information is used in administrative aspects to support reimbursement, make decisions regarding services, and analyze the quality of patient care. The administrators of the facility rely on the review of health information to make decisions regarding the management of the facility. For example, review of health information may indicate that improper coding, which affects reimbursement, caused a significant decrease in revenue or that patients who receive physical therapy soon after heart surgery recover in a shorter time. Health information is also used to make decisions about the health care services offered, to formulate policies, and to design an organizational structure. Administrators also use health information to negotiate and evaluate contracts with managed care companies or other vendors, such as surgical supply companies and laundry services. For surgical supply companies and laundry services, the facility uses statistics from its database to negotiate terms of a contract. The statistics help the facility determine the proper quantities of supplies to purchase. Health care facilities are required to report statistics on communicable and infectious diseases to agencies of the federal government, as discussed in Chapter 10. The agencies use this information to aid in the prevention and treatment of these diseases. As you read about this use of health information, it is important to understand some statistical terms. Prevalence is the extent to which something occurs—that is, the number of existing cases. Incidence is the rate of occurrence—that is, the number of new cases. Prevalence and incidence are very similar terms, but they differ in that incidence captures only new cases of a disease, and prevalence captures all existing cases of the disease. By studying the number of cases and the speed at which a disease is spreading in a given population, the government can target areas for prevention and treatment. The other statistics that are reported as a result of the review of health information are mortality rates and morbidity rates. Mortality rates indicate the frequency of death. Morbidity rates convey the prevalence and incidence of disease or sickness. Federal agencies monitor, study, and determine the impact of diseases on American public health. Morbidity rates may also refer to statistics used within the hospital to study the frequency of certain complications, such as infection rates. Within the U.S. government, the Department of Health and Human Services (DHHS) is responsible for overseeing many agencies that have an impact on health care. The mission of the Centers for Disease Control and Prevention (CDC) is “to promote health and quality of life by preventing and controlling disease, injury, and disability” (Centers for Disease Control and Prevention, 2010). The agencies of the CDC use health information to study diseases and support their mission. The centers, institutes, and offices in the CDC are responsible for a wide variety of health issues, including minority health, human immunodeficiency virus, sexually transmitted diseases, tuberculosis prevention, occupational safety and health, chronic disease prevention and health promotion, infectious diseases, and genetics. Federal and state governments use health information when making decisions related to health care. Sometimes their decisions have an impact only on Medicare and Medicaid beneficiaries; at other times, their decisions influence the legislation that governs other areas of health care. For example, the Health Insurance Portability and Accountability Act (HIPAA) of 1996 affects health plans, health care clearinghouses, and providers. This legislation affects many aspects of health care, including the portability of health insurance, privacy and security of health information, and the standardization of electronic transfer of health information. Among many things HIPAA made universal are the following: In February 2009, President Barack Obama signed Public Law 111-5, known publically as the American Recovery and Reinvestment Act (ARRA). Although the law was intended to do as the title suggests—provide funding to an ailing economy—it also provided stimulus money for various projects, including health information technology (HIT). The section of this law that dealt specifically with HIT is known as the Health Information Technology for Economic and Clinical Health (HITECH) Act. This act promoted many things related to health information but was specifically intended to promote implementation of the electronic health record (EHR). To ensure implementation of the EHR, the government provided incentives for providers who not only implemented an EHR but also provided proof of “meaningful use” of the product in the health care delivered to its patients. For the benefit of Americans the HITECH act defined “meaningful use” and required that certified EHR technology be used in meaningful, connected, and measurable ways. In other aspects of federal regulation, health information is used to determine the type of coverage that Medicare or Medicaid patients receive. Specifically, the CMS (and other agencies) reviews the history of care provided to its beneficiaries and determines the cost and quality of that care to make decisions and enact legislation. These decisions and the legislation affect future coverage, reimbursement, and availability of services for Medicare and Medicaid beneficiaries. Health care policy is another method the federal government uses to influence health care. The U. S. Surgeon General is an advisor, spokesperson, and leader for many health issues that affect the United States public. For example, a familiar influence of the U.S. Surgeon General is the warnings on tobacco and alcohol products manufactured in the United States (Figure 11-2). How did the Surgeon General’s office decide that this warning was necessary? The incidence and prevalence of certain diseases, combined with research requiring review of health information, indicate that tobacco and alcohol products can cause harm to society. The warning statements are one way the government has tried to affect how and when people use these products. The Surgeon General also works to educate the public and advise the President about disease prevention and health promotion in the United States. In order to facilitate the aggregate data collection necessary to make such public health decisions, HITECH legislation requires that providers use EHR technology to collect and report data on certain diseases and treatments. Box 11-1 lists core set and additional clinical quality measures (CQMs) that are monitored in order to improve public health decision making. For many diseases in our society, people have organized into groups to promote awareness, raise money for research, and increase prevention. Special lapel ribbons are worn to promote awareness of a particular disease. Breast cancer and acquired immunodeficiency syndrome (AIDS) awareness groups are quite common. These groups use widely known symbols (i.e., the pink and red ribbons, respectively) to promote public education. Since such groups have become involved in health care, more people are educated about the prevention, detection, and treatment of various diseases. These groups use health information, research, and statistics to inform the public. Health information in this case may relate to different populations’ exposure to a disease. Health information about the prevention, cause, and treatment of a particular disease can improve the recognition of the disease in a population. For many diseases, a diagnosis at an early stage is easier to treat, and the patient’s prognosis is better. Litigation is the process by which a disputed matter is settled in court. During litigation, health information is used to support a plaintiff’s or a defendant’s case. Health records can support or validate a claim of physician malpractice. However, the opposite can be proved if there is complete and accurate documentation showing that the physician was not at fault. The health record, when admissible in court, provides evidence of the events that are alleged in a lawsuit. Standards of care, expert testimony, and research are other sources of health information that may be used as evidence in a trial. Standards of care provide information about the typical method of providing services to a patient with a particular diagnosis. Expert testimony in health care gives the jury information or an explanation that helps them understand the highly technical language used in the health care profession. Research information furnishes information that the judge or jury can use to make decisions as well. Health information, whether specific to a patient or a disease, is helpful in litigation that involves a person’s health or injury. Health information is used in the education of health care professionals and patients. For example, physicians, nurses, physical therapists, and pharmacists need health information for instruction and examples as they learn how to perform their duties. The documentation of past occurrences provides an excellent opportunity to show others how to handle patient care in the future. Medical institutions use case studies of patients to teach new students about a disease process. Health care professionals are required to earn continuing education credits in their fields to keep their credentials current and to comply with professional standards. These professionals perform case studies on new and intriguing cases or present new technology for the education of their peers. Likewise, health information is presented to patients and the community to inform them of the prevention, causes, incidence, and treatment for many diseases. This use of health information involves research, statistics, and information on new technology for treatment or prevention of disease. Research is the systematic investigation into a matter to obtain or increase knowledge. Health-related research requires a tremendous amount of investigation of health information. In the health care profession, documentation from previous patient care, combined with the scientific process, allows physicians and other researchers to improve, develop, or change patient care and technology. The intention, of course, is to affect health care by giving patients the treatment they need to live longer, healthier, happier lives. Researchers review the health information from past or present patient health care. They retrieve data specific to their topic and analyze them to look for trends or suggested ways to enhance a treatment, disease, or diagnosis. They can analyze a patient’s response to medication or treatment, a prognosis, and the stages of a disease process—that is, the way in which the disease develops. Health information is documented during the course of the research. Although the health information may not be reported in the traditional form of a health record, it must be organized and stored in a manner that facilitates its retrieval and reference at a later date. Managed care is the coordination of health care benefits by an insurance company to control access and emphasize preventive care. Managed care organizations use health information internally and in their relationship with health care providers. A managed care organization chooses to use a health care provider’s services on the basis of an analysis of the provider’s performance. The managed care organization requires the health care facility to provide information about its services, performance, patient length of stay (LOS), outcomes, and so on. The managed care organization uses this information to determine whether to include the facility as a provider for the organization’s beneficiaries. This data gathering is part of the contract negotiation and evaluation. Before entering into a managed care contract, the managed care organization and the health care provider exchange a great deal of health information. While the facility is providing this information to the managed care organization, it also begins evaluating its own data to determine its ability to provide health care to this group of beneficiaries. With this information, the facility can determine whether the contract is viable. Managed care organizations can also be accredited by the National Committee for Quality Assurance (NCQA). The NCQA requires that managed care organizations comply with clinical and administrative performance standards, including a requirement for health records. Therefore the use of health information within a managed care organization has an impact not only on the benefits of the group members but also on the accreditation of the organization. The National Committee for Quality Assurance (NCQA) was founded in 1990. It is a nonprofit entity focusing on quality in health care delivery by accrediting managed care organizations. Partnering with employers, third-party payers, providers, and consumers (patients), the NCQA has issued a special data set called HEDIS, the Healthcare Effectiveness Data and Information Set. With standard measures of coverages, health insurance companies and employers can use HEDIS to negotiate group plans for employees. Marketing is the promotion of products and services in the hope that the consumer chooses them over the products and services of a competitor. Health information can be used for marketing. Many health care facilities are in business to make a profit. Regardless of their status, for-profit or not-for-profit, they must raise enough funds to sustain their business. Facilities routinely involve themselves in situations that allow them to compare their business with that of the competition. They analyze market share and compare usage and cost of particular services and information about patient LOS. In other words, they analyze statistical information obtained from health care information databases to determine whether there is a need for new treatment or technology in the community. Perhaps a study reveals that the facility has a significant share of the maternity market. There are methods that the facility can use to promote other services to patients who have used its maternity services. Facilities also analyze trends that show a need for a specific type of health care, such as dialysis care, midwifery, sports medicine, or laser surgery. The marketing department also uses a successful survey by an accreditation agency as a way to promote the facility in the community. Because the accreditation recognizes compliance with set standards, an accredited facility is perceived as better than one that is not accredited. Table 11-1 reviews all of the uses of health information mentioned in the previous sections. TABLE 11-1 The quality of health care data has been a running theme throughout this text. It is essential to note that high-quality data are used to monitor, verify, and improve patient care, reduce inefficiencies, and lower costs. Some people define quality as “something that is excellent,” on the basis of a personal definition, whereas others may judge quality by the outcome of the service (success, dead, alive). The level of quality is determined by the expectations of the customer evaluating the product or service. Thus the most important concept of quality is measurement. Customers of any product or service judge its quality. In health care, there are many customers—patients, physicians, insurance companies, attorneys, accreditation agencies, and employees, to name a few. Therefore a discussion of quality management in health care can focus on many different areas of service. Patients determine quality according to their perception of the services and care they receive. Physicians perceive the facility through the eyes of their patients, their office staff, and their professional and personal interactions with employees in the facility. Insurance companies perceive the quality of a facility through the cost and outcome of the services provided to their beneficiaries. Employees may perceive the facility’s quality through the competence of the staff and support from the administration. Accreditation agencies perceive quality in terms of the facility’s compliance with set standards. The facility itself measures quality on the basis of its priorities, market share, and customer feedback. These are only a few examples of how a facility’s quality is assessed, but it is certain that a health care facility is judged or assessed from many different perspectives. However it assesses quality, the facility must use a formal method for measuring, documenting, and improving quality. Health care facilities have a quality management department, usually staffed by HIM and nursing professionals, to monitor and assess quality. It is the primary responsibility of this department to educate those in the health care facility about the quality management and performance improvement process and to monitor the assessment of quality for the facility. This department monitors the facility’s compliance with accreditation standards by performing a significant number of record reviews, participating in and often coordinating medical staff and facility committees, and oversees performance (quality) improvement. This department also works closely with the HIM, risk management, and case management functions to coordinate efforts to improve quality. The department is also ultimately responsible for coordinating the duties associated with on-site accreditation surveys, such as those conducted by TJC. A discussion of quality should always begin with a review of the founding quality theories. The next section provides a simple explanation of three quality theories (though there are many others) and the use of health information in quality activities. Customer expectation and accreditation standards prompted the development of methods to prevent, detect, or correct flaws in a product or service to improve the quality. These methods are referred to as preventive controls, detective controls, or corrective controls, respectively. To understand why these quality management methods are important, you will find it helpful to know something about those who are credited with the founding theories: Deming, Juran, and Crosby. Their theories contain very similar and yet sometimes contradictory rules for managing quality. Although these writers did not become famous working with the health care industry, each has influenced the way the health care industry monitors quality. Therefore it would be correct to say they have inadvertently influenced the necessity to use health information to monitor quality and, in doing so, have promoted the improvement of the quality of health information. Of the three quality management pioneers, W. Edwards Deming was the first and is perhaps the most widely known. Deming established his reputation when the Japanese used his philosophy to rebuild their industry after World War II. As consumers increasingly chose products that were made in Japan, American industry realized the value of adopting a quality management philosophy. Deming’s philosophy is process oriented, with an emphasis on how a task is performed or a product is produced. A product that does not meet company standards must be identified before it is completed. If the problem is noted after the production is completed, the company may not be able to correct it. However, if a company inspects the process as the product is being developed, problems are more likely to be addressed and corrected before it is too late. Deming developed 14 principles to implement a successful quality management program and identified seven “deadly diseases” that would harm a quality management program. Deming’s quality principles (consolidated by Rudman, 1997) are as follows: • Change plus innovation equals stability and organizational survival. • Organizations have a responsibility to provide employees with appropriate education and resources. • Organizations must foster employee empowerment and pride in work. • Organizations should emphasize process and eliminate benchmark standards and performance evaluation. Another pivotal approach to quality management is Joseph M. Juran’s “quality trilogy.” According to Juran, every quality management program should have a strong yet balanced infrastructure of quality planning, control, and improvement. He also defined a successful program as one that is acceptable to the entire organization; the program should be as important to the employees as it is to the administrators. Finally, Juran emphasized the value of documentation and data in the quality management program. Philip Crosby is best known for the term zero defects. The Crosby quality management philosophy requires education of the entire organization. Education of the entire organization requires that everyone—staff employees, supervisors, managers, and administrators—learn about the program and be motivated to participate. For a health care facility to effectively improve the quality of its care and services, it needs to adopt some method or philosophy similar to the three mentioned here. The idea of checking the quality of health care provided in the United States is not new. Quality, however, is a major focus for the health care industry. In the eighteenth century, hospitals had a high incidence of deadly epidemics—owing to the lack of knowledge of disease etiology and infection control—and relatively high death rates. The poor received health care in hospitals, which were often administered by charitable organizations, mostly churches. The wealthy were usually visited in their homes. The concept of quality in health care can be traced to the late nineteenth century, when hospitals finally became known as places where people could go to get well, because of advances in the knowledge of disease and infection control. During this time, two important associations were founded: the American Medical Association (AMA) and the American Hospital Association (AHA). These two associations worked diligently to promote high-quality health care through standardized medical education and hospital functions. Figure 11-3 presents a time line of the evolution of quality in health care. Before the existence of formal medical education, physicians were trained through an apprenticeship. By the early twentieth century, many medical institutions existed to educate physicians. But the education of these physicians was not standardized. Each institution could decide which courses were required to obtain a medical degree. For this reason, the health care profession increased in size and number of physicians, but the quality of patient care was not improving. Although having more physicians seemed like a good solution to an ailing population, the facts suggested that more needed to be done to improve the quality of health care. Medical institutions needed a standardized mechanism to guide the training of physicians. Abraham Flexner studied the quality of medical education in the United States. His report in 1910 documented critical issues and discrepancies in medical education. The findings in the Flexner Report prompted the closing of many training institutions, revisions of the required curriculum in those that remained, and implementation by the AMA of a mechanism for accreditation of medical education institutions. It also led to a validation of competency for medical professionals.
Quality and Uses of Health Information
Chapter Objectives
Vocabulary
Uses of Health Information
Improving Patient Care
Support and Collection of Reimbursement
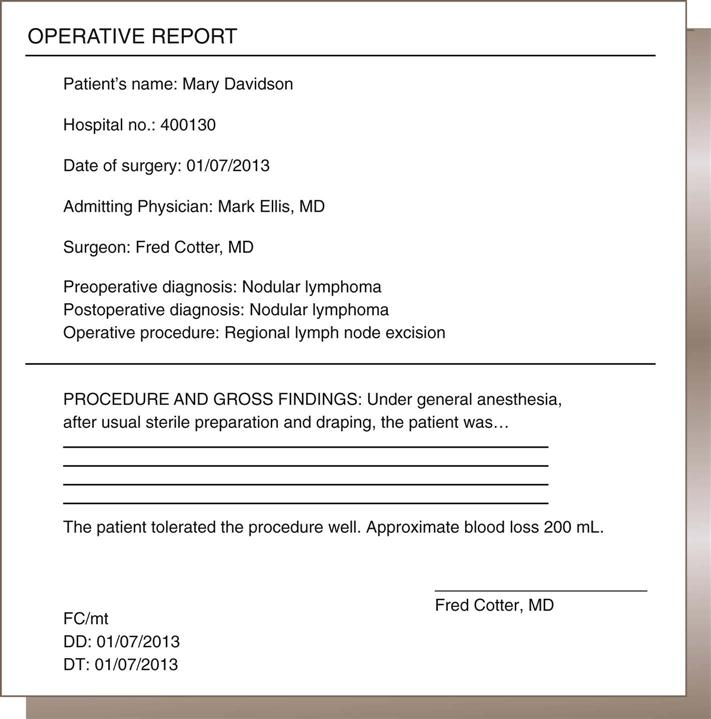
Licensure, Accreditation, and Certification
Administration
Prevalence and Incidence of Mortality and Morbidity
National Policy and Legislation
Development of Community Awareness of Health Care Issues
Litigation
Education
Research
Managed Care
The National Committee for Quality Assurance
Marketing
USE
EXAMPLE/EXPLANATION
Improvement in patient care
The health care facility uses the documentation in the health record to determine patient care.
Support and collection of reimbursement
Documentation of health care is used to support and collect reimbursement for services rendered to patients.
Licensing, accreditation, and certifications
Health information must be maintained as a requirement of licensure. Likewise, it supports compliance with certification requirements and accreditation standards.
Administration
Health information is used to make decisions regarding the delivery of health care services.
Prevalence and incidence of morbidity and mortality
Statistics are reports to aid in the prevention and treatment of certain diseases.
National policy and legislation
Research and statistics are references to establish policy and legislation related to health care (i.e., Medicare and Medicaid).
Development of community awareness of health care issues
Research and literature are used to educate the public regarding health care issues (e.g., cancer awareness programs).
Litigation
Health information is used to support or prove a fact in a lawsuit.
Education
Health information is used to educate patients, clinicians, allied health professionals, and the public.
Research
Health information is used to support and document health care research.
Managed care
A managed care organization evaluates health information (statistics) to determine whether to include a facility in its plan. Also, managed care organizations use health information to analyze services provided to their beneficiaries.
Marketing
Analysis of health information provides statistical information that the marketing department can use to promote the facility within a community.
The Quality of Health Care
Quality Management Theories
Deming
Juran
Crosby
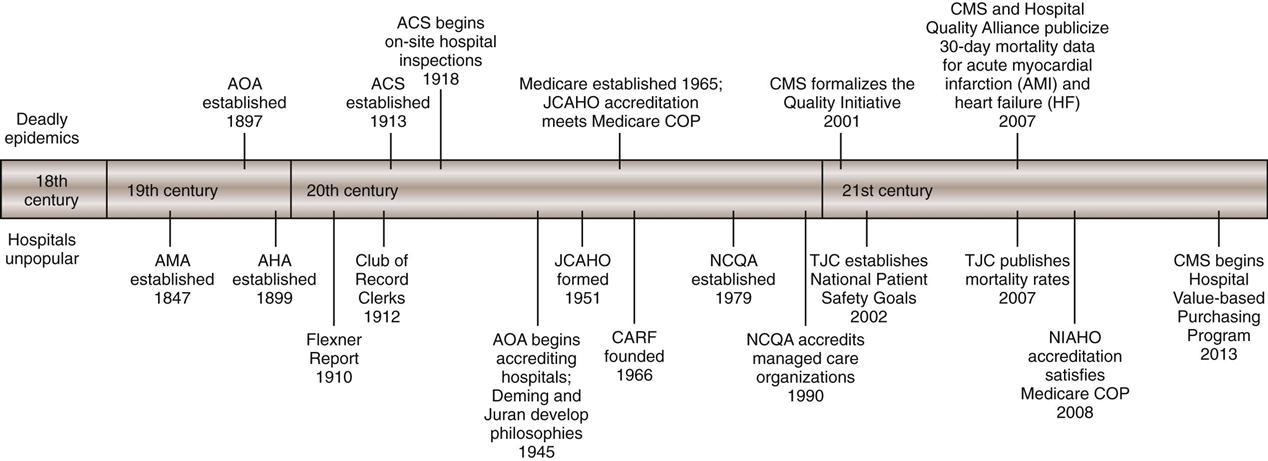
History and Evolution of Quality in Health Care
Medical Education
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Quality and Uses of Health Information
Get Clinical Tree app for offline access