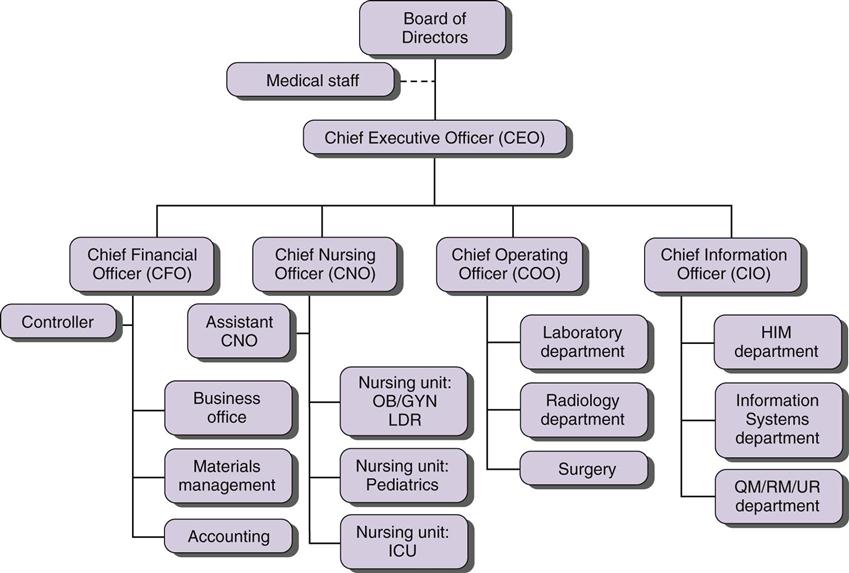
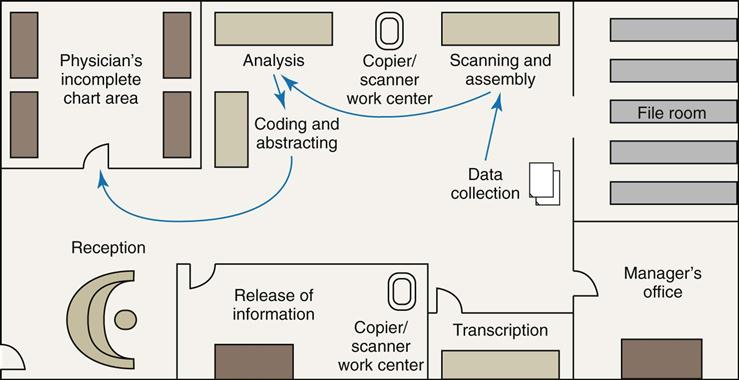
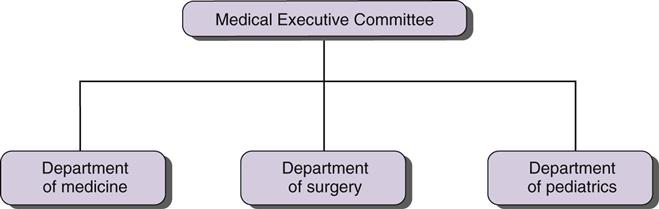
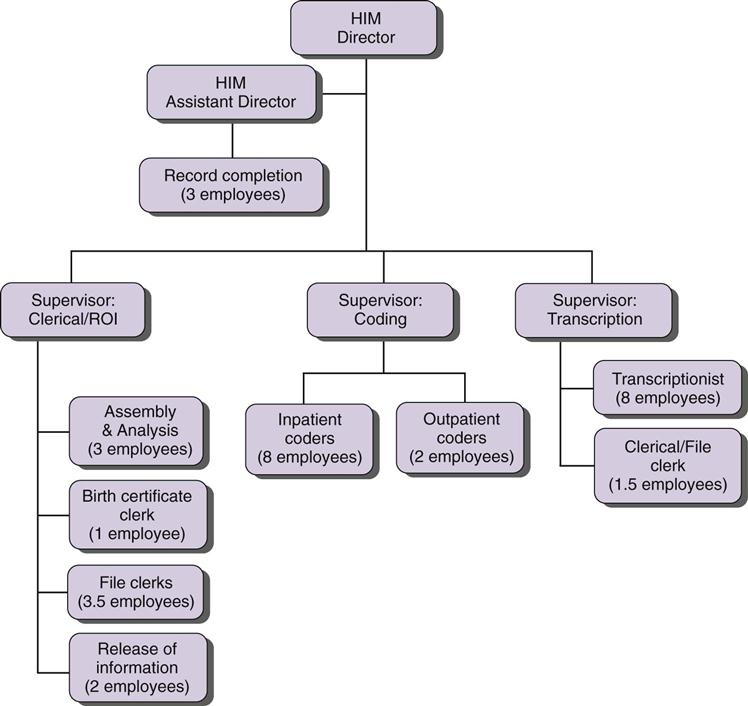
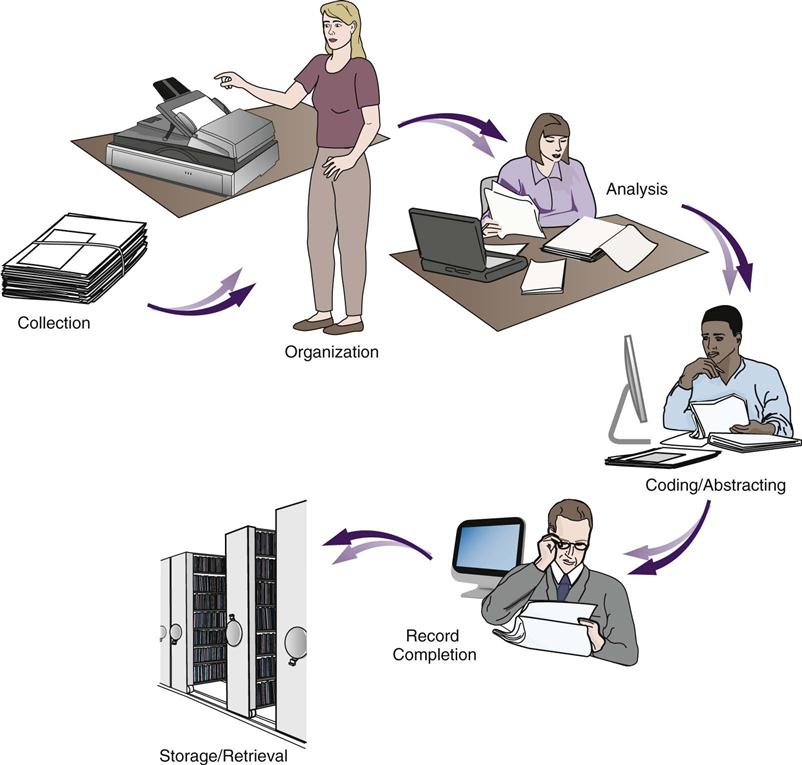
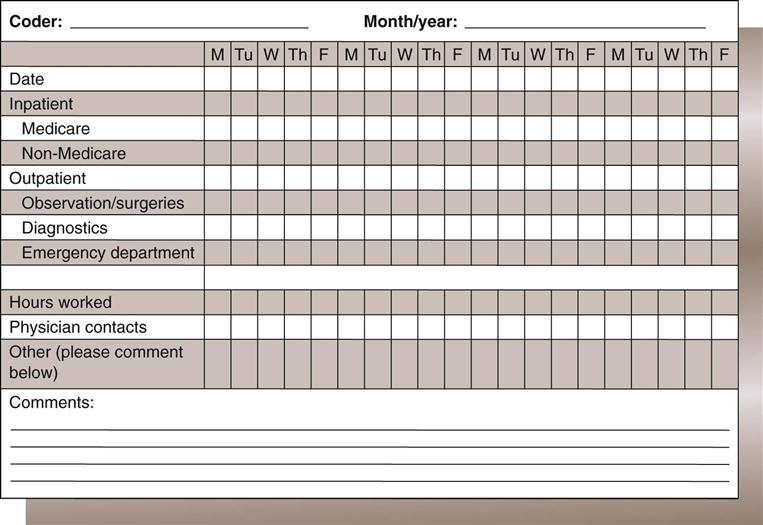
Melissa LaCour By the end of this chapter, the student should be able to: 1. Explain the purpose of the organization chart. 2. Organize the appropriate workflow of health information management functions and services. 3. Develop plans, goals, and objectives for health information management employees. 5. Develop department policy and procedures for health information management functions and services. 7. Write job descriptions using the Americans with Disabilities Act requirements. 8. Develop health information management department policies for employee operations and conduct. 11. Evaluate the effectiveness of operations and services in a health information management department. 12. Explain the steps associated with hiring health information management department employees. 13. Identify health information management functions that can be outsourced. 14. Monitor the use of department resources, including inventory, budget, and planning. capital budget chain of command delegation ergonomics full-time equivalent (FTE) goals job analysis job description matrix reporting mission statement objectives operational budget organization chart outsourcing performance improvement plan (PIP) performance standards policy procedure productivity request for proposal (RFP) span of control stakeholder system development life cycle (SDLC) unity of command vision workflow analysis This chapter focuses on issues, tools, and techniques used to manage health information management (HIM) employees who perform HIM department functions. Previous chapters explained how to process, maintain, and secure health information. In these final two chapters, human resources, organization, planning, policy, procedures, equipment, and supplies are discussed in the context of their importance, relevance, or function in the HIM department. Within an organization, the human resources (HR) department maintains personnel records; handles employee benefit issues; and advertises for, interviews, hires, disciplines, and terminates facility employees. HR works with the managers and supervisors in the health care facility when developing job descriptions and performance standards, conducting employee performance evaluations, handling employee conduct problems, and managing other technical aspects of employment. Supervisors, managers, and directors of an HIM department should consult the human resources department for advice and guidance as necessary on these matters when managing employees. The phrase “human resources within the HIM department” refers to the employees, who are the source of effort and productivity required to accomplish health information functions. Along with physical resources such as buildings and technology, and capital resources that allow the operation to run, employees are resources that are essential to performing the work/job duties/tasks. Although many functions in a health care facility are electronic, humans are still needed to facilitate HIM functions to ensure timely, complete, and accurate health information. Furthermore, the appropriate management of HIM employees has an impact on the entire organization. Managers are responsible for efficient and effective use of all the resources in an organization, including the people. They organize workflow, establish policy and procedures, hire, and monitor employee productivity and performance. In this chapter we discuss many of the tools HIM managers employ to coordinate these functions. Please note that HIM departments differ among health care facilities. The methods that work in one department may not work the same in another department. Employees may be classified according to hours worked (full-time or part-time) or by position—such as management or staff. Those in management or supervisory positions have responsibility for other employees. Staff employees are responsible for daily tasks and functions, and they report to a supervisor or manager. As shown in Table 13-1, employee classifications by hours worked are full-time, part-time, and temporary (also known as PRN [as needed], extra help, pool, or per diem). A full-time employee typically works 32 to 40 hours each week—up to 2080 hours per year—excluding overtime (or in some cases, 64 to 80 hours every 2 weeks), thereby earning full benefits as offered by the health care facility. Full-time status affects employees’ benefits in terms of hours earned in paid time off (PTO), vacation, holiday benefits, and retirement options. For example, an employee who works 40 hours each week is considered a full-time employee, and he or she may earn 4 hours of vacation each week. Additionally, the organization might match retirement benefits for the full-time employee at a rate higher than for other classes of employees. TABLE 13-1 A part-time (PT) employee is one who typically works less than the standard, full-time hours (frequently less than 20 hours) per week, thereby earning benefits at half the weekly rate of a full-time employee, if at all. For example, a PT employee may earn 2 hours of vacation, sick leave, or paid time off for every 20 hours of work. Temporary or per diem employees rarely earn any type of employee benefit. Per diem employees are scheduled to work as needed in the facility when the amount of work exceeds what the regular employees can accomplish. These employees are valuable to the organization when there is an unexpected excess of work. Staffing complements are often described by the number of full-time equivalent (FTE) employees. If the normal work week is 40 hours, an employee working 20 hours is one half of an FTE. Similarly, two part-time employees working 20 hours per week is equivalent to one employee working 40 hours per week. These two part time employees equal one FTE. All of the regularly scheduled hours for the week are added then divided by the full-time work week hours to arrive at the total number of FTEs for the department. Example: In this example, the department staff are scheduled to work 115 hours per week. The full-time work week is 40 hours. Therefore the employee complement is 2.875 FTEs (115 divided by 40). Some people who work in the HIM department are employed by an agency or company that “contractually” agrees to perform certain job functions for the HIM department or health care facility. These employees are paid by the agency or company, not the health care facility. A facility might choose to make this arrangement to acquire specialized help in a particular HIM function such as release of information (ROI), transcription, or coding. This type of contractual arrangement is also called outsourcing, whereby the work is performed by workers other than those employed by the facility. These categories are discussed in more detail later in the chapter, with regard to the HIM department structure. One method used by health care facilities to describe the arrangement of departments and positions is the organization chart. The organization chart illustrates the relationships among departments, positions, and functions within the organization. The traditional structure of an organization chart resembles a pyramid, in which there are more departments and personnel at the bottom than at the top. An organization chart uses boxes and lines to represent departments and positions within the facility (Figure 13-1). Each box indicates a department or position. The higher the box is located within the chart, the higher the authority and responsibility of the position or department that it represents. Boxes on the same level indicate similar levels of authority or responsibility. Lines connecting the boxes indicate relationships. Solid lines indicate a direct relationship. Broken lines indicate an indirect (or shared) relationship. The lines in the organization chart illustrate the subordination of positions in the chain of command. The chain of command refers to the order in which decisions are made within the facility. For decisions that require approval, the organization chart describes who must give that approval. Therefore the organization chart also represents the reporting structure; it indicates which individuals manage or have authority over another employee or department. The traditional health care facility is composed of departments with specialized personnel or services; these are related to the health care professions discussed in Chapter 1. Figure 13-1 is a useful reference when you are considering the organization chart of a medium-sized acute care facility. The box at the top of the chart represents the ultimate authority and responsibility within the organization. This authority is usually called the governing body, board of directors, or board of trustees. Every health care facility has this type of authority at the top of the organization. There are typically 8 to 25 members on the board, depending on the size of the facility. Members of the board include the chief executive officer (CEO), members of the medical staff, and members of the community. The board meets regularly to review the business of the health care facility, set direction, and monitor progress. The board has two distinct relationships, as shown in Figure 13-1. One is their delegation of authority to the CEO for the daily operations of the facility. The other is the relationship with the facility’s medical staff. The medical staff is organized as a membership group of physicians governed by the facility’s medical staff bylaws, rules, and regulations. They admit patients to the health care facility and provide care during the patient stay. In addition, the medical staff has a responsibility to aid the administration in the longer-term planning of the health care facility. An example of medical staff structure is shown in Figure 13-2. The CEO, under the governing board, is given the authority to oversee the daily management of the health care facility. The CEO must guide, motivate, and lead the organization, receiving direction of the governing board. Below the CEO are several administrative positions. These positions have authority over specific departments within the organization. These administrators report to the CEO and are accountable for the operations of their departments. This level of the administration is also known as the chiefs, or the “C-Suite”: chief operating officer (COO), chief nursing officer (CNO), chief financial officer (CFO), chief information officer (CIO); and assistant administrators, or vice presidents of finance, nursing, information, and quality. The personnel responsible for managing specific departments report to the aforementioned administrators. The managers of the departments are known as directors, department heads, or managers. Below department directors are supervisors, and then staff employees. The managers of each department have authority over the supervisors within their departments, and finally the staff employees within each department report to their respective supervisors. In an organization chart, the number of positions or employees shown below the box for an administrator, manager, or supervisor indicates the span of control for that position. The span of control is the number of employees or departments that report to one individual. The span of control for one supervisor must be appropriate so that management is efficient and effective. Too many varied responsibilities or employees under one supervisor can lead to ineffective management. A large facility may require more managers than a small facility because of the number of employees needed to accomplish tasks or functions. It is equally important that any individual employee reports to only one manager. This concept is called unity of command. If one employee has two supervisors, this can cause a dilemma as to which manager’s authority is higher or which manager’s rules and requests take precedence. If both managers have deadlines, which one must be met first? Who decides? If the employee has only one manager, the employee knows that he or she is accountable to that manager according to the role and responsibility of the position. In an increasingly challenging health care environment, it is not always possible or practical to maintain strict unity of command. Further, with performance improvement and other quality efforts crossing all aspects of a facility, the functional responsibility for a project may result in an employee, particularly a manager, reporting to multiple higher level individuals, either formally or informally. This type of cross-departmental chain of command is called matrix reporting. Matrix reporting is typically represented by broken or dotted lines on an organization chart, if the reporting line is permanent and inherent in the duties of the employee. Less formal matrix reporting that results from project work is not generally represented on the table of organization. The issues mentioned in the previous paragraph are inherent in matrix reporting. Clear communication, documentation of responsibilities, and measurable performance objectives are common ways to overcome these issues. Delegation describes what a manager does when he or she assigns responsibility to an employee to complete a project or task. The employee to whom the task is being delegated may need some authority to get the job done (e.g., signing forms, making changes in a process, and disciplining employees). Delegating empowers an employee with the responsibility and the necessary authority to accomplish the project or task. Delegation is not only a tool that managers use to accomplish multiple tasks; it is also an important motivator. It shows the employee that the manager trusts him or her to do a good job and allows the employee to take ownership of the project. Figure 13-3 illustrates a table of organization within the HIM department. This is an organization chart for an HIM department with 30 employees. The box at the top of the chart represents the department director. The person in this position has the delegated authority from the administration of the facility to act as the custodian of health information. This position also has the responsibility and authority to manage the daily operations of the HIM department. Figure 13-3 shows a department with one director, one assistant director, three supervisors, and 32 staff employees. Keep in mind that job titles for positions within the HIM department vary among facilities. In addition, the organization chart in Figure 13-3 shows a department that is organized into three supervised sections of health information functions. Each supervisor is responsible for specific functions within the department. There is a supervisor for the assembly, analysis, release of information (ROI), and filing functions, also known as the clerical, or ROI, supervisor. Another supervisor, called the coding supervisor, oversees the coding and abstracting functions. The third supervisor, the transcription supervisor, is responsible for the transcription function. Supervisors work at the staff level to ensure that the daily tasks in the HIM department are accomplished in a timely and accurate manner. Supervisors typically work in close proximity to or with the employees they supervise. They are on hand to handle in a timely manner issues, questions, and situations that arise. Responsibilities of the supervisor positions differ in each department, but they may include scheduling, hiring, training, disciplining, and terminating. The supervisor is responsible for ensuring that staff employees are performing their functions efficiently and consistently with the policies of the department. Within the HIM department, employees are further identified by the positions that they hold or job functions that they perform. HIM departments have clerical and technical staff positions (Table 13-2). The director of the HIM department or the human resources department determines the title for employee positions. Some titles are generic (e.g., HIM Tech I), whereas other titles describe the employee’s responsibilities (e.g., inpatient coder, outpatient coder, scanning technician, ROI clerk, revenue cycle supervisor). TABLE 13-2 STAFF POSITIONS IN THE HEALTH INFORMATION MANAGEMENT DEPARTMENT HIM, health information management; ROI, release of information; STAT, immediate. Clerical employees are responsible for the functions known as scanning (or assembly), indexing and data validity (analysis), and release of information (filing). Technical employees perform functions such as coding, abstracting, and transcription. (Table 13-2 describes possible job titles.) Such positions are sometimes referred to as HIM Tech II. These staff employees typically report to the first or lowest level of management, either the HIM supervisor or a team leader. The titles, roles, and responsibilities of positions within the HIM department vary. Smaller facilities with few patient admissions have fewer positions as well as fewer levels of management. However, larger health care facilities have several employees performing one function, and they require more supervisors and levels of management to oversee daily functions. The collection, organization, coding, abstracting, analysis, storage, and retrieval of patient health information are organized into a workflow within each health care organization to best suit that facility. Workflow is the order in which tasks are organized to progress from one function to the next. Efficient workflow allows department employees to accomplish their functions in a timely, accurate, and complete manner. Although managers should continually look for ways to remove obstacles and streamline the workflow in their departments, workflow analysis, or a careful look at how work is performed, is especially crucial when a facility is implementing new software, or in the process of migrating to an electronic health record (EHR). Because every HIM department is different, this section covers general workflow concepts such as the management and organization of HIM functions with only a few variations. Variations in the workflow among different facilities are necessary to accommodate the type, size, and structure of each health care facility. First let’s review HIM functions and responsibilities as they are commonly conceived in health care facilities that use paper-based records. As shown in Figure 13-4, health records undergo several distinct processes which enable the current and future use of the data they contain: Storage—the filing methods used to maintain records for future use Retrieval—the function that locates a record for future use following patient care Figure 13-5 shows a typical HIM department layout and the locations where these actions might occur for the most efficient workflow. These HIM functions occur sequentially and are typically grouped into sections under a supervisor for efficient management (see Figure 13-3). The need for supervisors within a department, as discussed previously, is determined by the number of employees in the HIM department and their varied functions. Typically, supervisors oversee 6 to 12 employees, depending on the functions performed by the group and the employees’ need for direct supervision. If there are 12 transcriptionists, only one supervisor may be necessary. However, if the department is relatively small and there are only 12 employees total, 6 of whom are clerical workers, 3 of whom are coders, and 3 of whom are transcriptionists, the department may have 3 supervisors, 1 each for the clerical, coding, and transcription sections. In this situation the supervisor is likely an employee who performs the job functions well and actually leads the others to ensure the work is performed. Other areas where it can be important to have a supervisor is over revenue cycle (all processes that help generate revenue from the time of discharge), and another may be over release of information with responsibility for patient interaction, audits, and HIPAA. Each department must have a method for completing its workload. The amount of work in the HIM department is determined by the number of discharges, by the type (e.g., outpatient, inpatient, rehab), and length of stay (LOS). The number of patients discharged each day will be equal to the number of records that must be processed. The patient type (e.g., inpatient, outpatient, rehab, psych) determines the extent of the processing. For instance, ambulatory/outpatient records are very brief and are relatively easy/quick to process. Ambulatory surgery records require less time to review than inpatient stays. Likewise, the LOSs for patients who have been discharged affect the length of time that it will take to process (and code) the patients’ charts. If a patient has an LOS in the facility of 2 days, the record is relatively thin (e.g., approximately 1 inch). However, if the patient remains in the facility for 21 days, the record is relatively thick (approximately 2 to 3 inches) and may require two folders to contain the papers for that one stay. If your facility has many discharges with long LOSs, then the assembly process will take longer than in a facility that has few discharges with short LOSs. Supervisors may use time studies to determine the appropriate number of employees for the workload. A time study can be accomplished by monitoring the employee(s) performing the function and the time that it takes to complete each task. This helps the supervisor identify how much work can be done by one employee in a specific period. It also determines the percentage of accuracy with which the work should be completed. If the supervisor is actually present while the employee performs the job, the employee may become nervous or irritated. Likewise, a supervisor does not want to waste valuable time watching employees work. Other methods exist to capture this information without physically watching employees. Employees can fill out forms to indicate their performance, productivity, and time (Figure 13-6). In an electronic system or with document conversion, data may be available from the system through reporting. The standards set for the department must comply with organizational, professional, licensing, and regulatory requirements. These standards determine when many of the functions must be performed (e.g., scanning/assembly and analysis within 24 hours of discharge and coding within 48 hours of discharge; Table 13-3). Some internal standards may lead the way for new processes, such as concurrent analysis or coding, to successfully accomplish department functions within the set time frame. TABLE 13-3 TYPICAL HIM DEPARTMENT STANDARDS* *Note: These standards are for example only; standards in HIM departments may vary. The standards, along with the amount and type of work, dictate the operating hours of the HIM department and the scheduling of the employee(s) work hours. Some departments in large health care facilities are open 24 hours a day, 7 days a week. Other departments have limited hours (Monday through Friday 7 AM to 9 PM and part-time on weekends) and use cross-trained staff (i.e., nursing) to cover emergency issues when the department is closed (see Table 13-2). Workload is also affected by the amount of computerization in the HIM department. In some instances, technology reduces the complexity of a function, making it easier to complete HIM processes in a timely manner, and at other times it increases the steps in the process to complete a function. For example, in a hybrid record, the time needed to process a record for scanning and indexing can add complexity to the process formerly called assembly and analysis. Prioritization of health information functions can occur once the department has established its goals and objectives. Earlier in the chapter, Table 13-3 provided a list of potential HIM department standards. Standards for department functions are necessary to keep the processes flowing. For example, in this textbook HIM functions are discussed in the following order: assembly, analysis, or postdischarge processing (Chapter 5), coding (Chapter 6), and filing (Chapter 9). However, coding may actually be a function that should occur very early in the workflow. The department may have a goal to reduce accounts receivable (AR) days, a measure of the average length of time it takes to collect on outstanding accounts, which may be lessened by prioritized coding in the workflow. Typically, though, scanning and analysis are the first tasks performed to organize the record for the other HIM processes like coding, abstracting, and record review. The HIM director must also make sure that the records are analyzed for deficiencies quickly to meet The Joint Commission (TJC) or state standards for record completion—whichever is the most stringent. TJC standards require a complete record within 30 days of discharge, although some states preempt this standard, requiring a completed record within 14 days of discharge. The longer it takes for HIM staff to analyze a record, the less time is available to get the record completed by a physician. The manager also sets standards for functions such as ROI and transcription. Timely completion of requests for ROI can affect continuity of patient care and possibly reimbursement, if the request is related to payment. The transcription team processes the dictated patient health information into a report that is used in communication and decision making during patient care. Timely completion of transcription affects patient care. Department standards set the framework for efficient and effective management of health information. The standards direct the employees within the department workflow to accomplish their tasks in a timely manner. Sometimes, the task affects patient care directly; at other times, the task is part of department workflow and could impact the revenue cycle or customer service. Standards can then be used to evaluate the function of the HIM department. It is important that supervisors and managers continually evaluate their departments according to department goals, objectives, and standards. If the standard is to assemble and analyze records within 24 hours, then the HIM manager must ensure that his or her employees are doing that. Evaluation of goals and objectives takes place annually, but employee-specific productivity should be evaluated at least monthly to ensure quality in the HIM department. HIM managers and supervisors continually monitor the effectiveness and efficiency of the department through employee productivity reports (Figure 13-7) and through quality assurance monitoring. These measures alert the supervisors to any problems. Significant problems can then be addressed through employee training, performance improvement, or quality improvement efforts.
HIM Department Management
Chapter Objectives
Vocabulary
Human Resources
CLASSIFICATION
COMMON TERMS
DESCRIPTION
Full-time
FTE
Employee who works 32-40 hours each week, or 64-80 hours every 2 weeks, earning full benefits
Part-time
PT
Employee who typically work less than the minimum full-time hours; frequently less than 20 hours each week, occasionally earning benefits at half of the full-time rate
Temporary
Pool, PRN, per diem
Employee scheduled to work as necessary because of an increased workload
Sue
20 hours
James
15 hours
Mary
40 hours
Alison
40 hours
Total hours
115 hours
Organization Charts
Facility Organization
Span of Control
Unity of Command
Delegation
HIM Department Organization
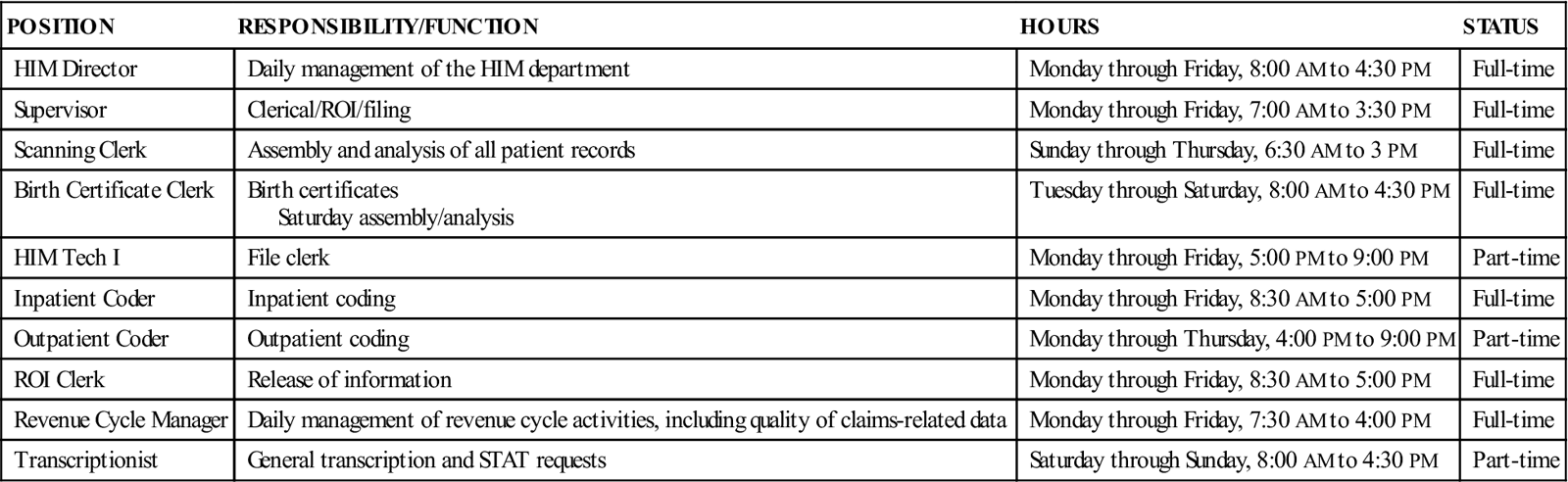
POSITION
RESPONSIBILITY/FUNCTION
HOURS
STATUS
HIM Director
Daily management of the HIM department
Monday through Friday, 8:00 AM to 4:30 PM
Full-time
Supervisor
Clerical/ROI/filing
Monday through Friday, 7:00 AM to 3:30 PM
Full-time
Scanning Clerk
Assembly and analysis of all patient records
Sunday through Thursday, 6:30 AM to 3 PM
Full-time
Birth Certificate Clerk
Birth certificates
Saturday assembly/analysis
Tuesday through Saturday, 8:00 AM to 4:30 PM
Full-time
HIM Tech I
File clerk
Monday through Friday, 5:00 PM to 9:00 PM
Part-time
Inpatient Coder
Inpatient coding
Monday through Friday, 8:30 AM to 5:00 PM
Full-time
Outpatient Coder
Outpatient coding
Monday through Thursday, 4:00 PM to 9:00 PM
Part-time
ROI Clerk
Release of information
Monday through Friday, 8:30 AM to 5:00 PM
Full-time
Revenue Cycle Manager
Daily management of revenue cycle activities, including quality of claims-related data
Monday through Friday, 7:30 AM to 4:00 PM
Full-time
Transcriptionist
General transcription and STAT requests
Saturday through Sunday, 8:00 AM to 4:30 PM
Part-time
HIM Department Workflow
Workload and Productivity
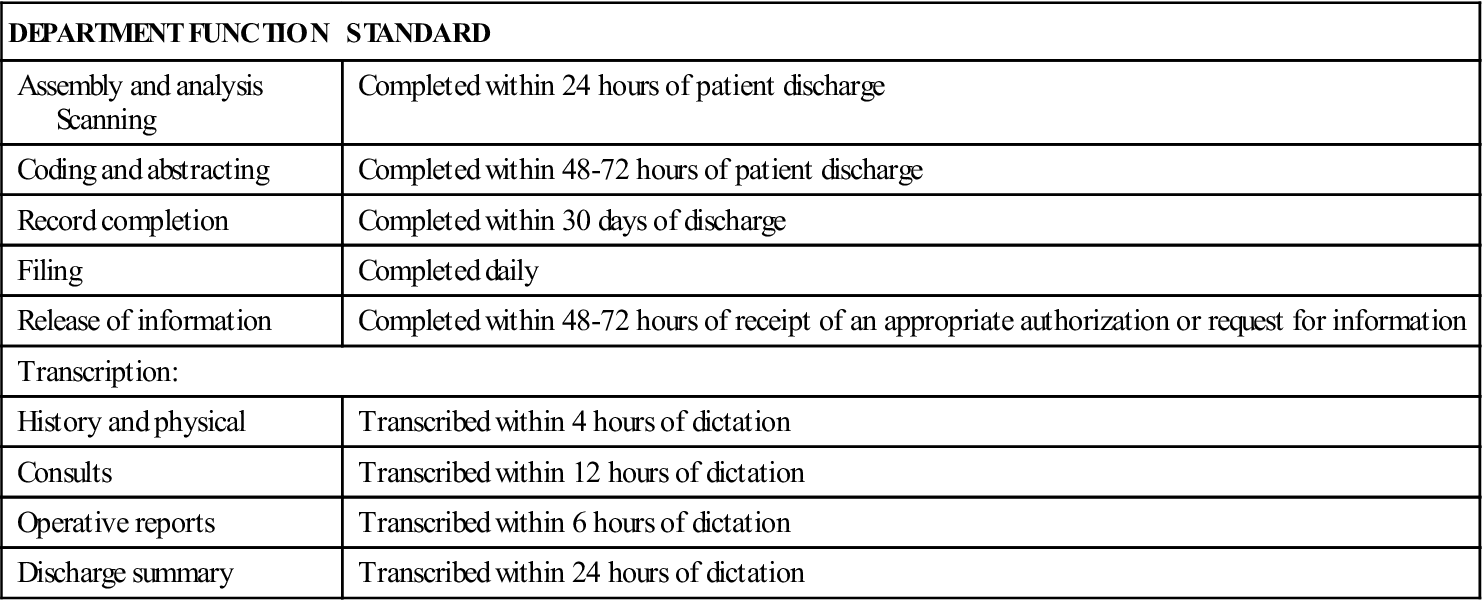
DEPARTMENT FUNCTION
STANDARD
Assembly and analysis
Scanning
Completed within 24 hours of patient discharge
Coding and abstracting
Completed within 48-72 hours of patient discharge
Record completion
Completed within 30 days of discharge
Filing
Completed daily
Release of information
Completed within 48-72 hours of receipt of an appropriate authorization or request for information
Transcription:
History and physical
Transcribed within 4 hours of dictation
Consults
Transcribed within 12 hours of dictation
Operative reports
Transcribed within 6 hours of dictation
Discharge summary
Transcribed within 24 hours of dictation
Prioritization of Department Functions
Evaluation of Department Operations and Services
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



HIM Department Management
Get Clinical Tree app for offline access