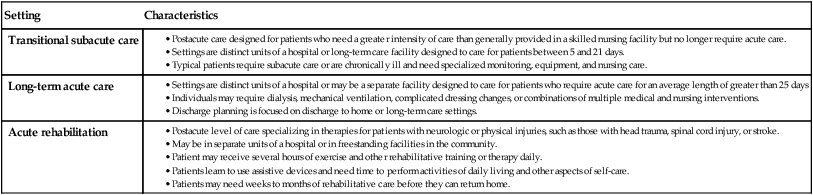
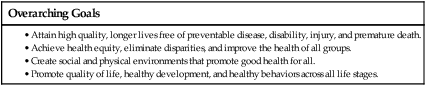
Chapter 1 1. Describe professional nursing practice in terms of domain, definitions, and recipients of care. 2. Compare the different scopes of practice available to professional nurses. 3. Analyze the effect of expanding technology and knowledge, changing populations, consumerism, and evolving health care systems on professional nursing practice. 4. Describe the role of critical thinking skills and use of the nursing process to provide patient-centered care. 5. Explain how standardized nursing terminologies for nursing diagnoses, patient outcomes, and nursing interventions can be used and linked. 6. Evaluate the role of informatics and technology in nursing practice. 7. Apply concepts of evidence-based practice to nursing practice. 8. Discuss the role of integrating safety and quality improvement processes into nursing practice. 9. Explore the role of the professional nurse in delegating care to licensed practical/vocational nurses and unlicensed assistive personnel. Nursing practice today consists of a wide variety of roles and responsibilities necessary to meet society’s health care needs. As a nurse, you are the frontline professional of health care (Fig. 1-1). You practice in virtually all health care settings and communities across the country. You have never been more important to health care than you are today. As a nurse, you (1) offer skilled care to those recuperating from illness or injury, (2) advocate for patients’ rights, (3) teach patients so that they can make informed decisions, (4) support patients and their caregivers at critical times, and (5) help them navigate the increasingly complex health care system. Although the majority of nurses are employed in acute care facilities, many nurses practice in long-term care, home care, primary and preventive care, ambulatory clinics, and community health. Wherever you practice, recipients of your care include individuals, groups, families, or communities. eTABLE 1-1 PRACTICE SETTINGS FOR TRANSITIONAL CARE eTABLE 1-2 PRACTICE SETTINGS FOR LONG-TERM CARE eTABLE 1-3 OVERVIEW OF DELEGATION, ASSIGNMENT, AND SUPERVISION 1. Assess and plan the delegation based on patient needs and the available resources. 2. Communicate directions to the delegatee, including unique patient requirements and characteristics, as well as clear expectations regarding what to do, what to report, and when to ask for assistance. 3. Know the surveillance and supervision of the delegation, including the level of supervision needed for the particular situation and the implementation of that supervision, including follow-up to problems or a changing situation. 4. Evaluate and provide feedback to consider about the effectiveness of the delegation, including any need to adjust the plan of care. 1Motacki K, Burke K: Nursing delegation and management of patient care, St Louis, 2011, Mosby. 2National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA): In Joint statement on nursing delegation. 2006. Retrieved from www.ncsbn.org/1056.htm. The American Nurses Association (ANA) declares that the authority for the practice of nursing is based on a contract with society that acknowledges professional rights and responsibilities, as well as mechanisms for public accountability.1 The knowledge and skills that comprise nursing practice are derived from society’s expectations and needs. Nursing practice continues to evolve according to society’s health needs and as knowledge and technology expand. This chapter introduces concepts and factors that affect professional nursing practice. • Nursing is putting the patient in the best condition for nature to act (Nightingale).2 • The nurse’s unique function is to assist patients, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that they would perform unaided if they had the necessary strength, will, or knowledge—and to do this in such a way as to help them gain independence as rapidly as possible (Henderson).3 In 1980 the ANA defined nursing as “the diagnosis and treatment of human responses to actual and potential health problems.”1 In this context, a nurse caring for a person with a fractured hip would focus on the patient’s possible responses to immobility, pain, and loss of independence. Nursing theorists are in widespread agreement that an individual has physiologic (or biophysical), psychologic (or emotional), sociocultural (or interpersonal), spiritual, and environmental components or dimensions. In this text the human individual is considered “a biopsychosocial spiritual being in constant interaction with a changing environment.”4 The individual is composed of dimensions that are interrelated and not separate entities. Thus a problem in one dimension may affect one or more of the other dimensions. An individual’s behavior is meaningful and oriented toward fulfilling needs, coping with stress, and developing one’s self. However, at times an individual needs help to meet these needs, cope successfully, or develop his or her unique potential. The extent that individual nurses engage in the scope of practice depends on their educational preparation, experience, and role, and is guided by individual state laws. To enter into practice, a nurse must complete an accredited program and pass an examination verifying the nurse has the skills necessary to provide competent care. Entry-level nurses with associate or baccalaureate degrees are prepared to function as generalists. At this level, nurses provide direct health care and focus on ensuring coordinated and comprehensive care to patients in a variety of settings. They work collaboratively with other health care providers to manage the needs of individuals and groups.5,6 With experience and continued study, nurses may specialize in an area of practice. Certification is a formal way for nurses to obtain professional recognition for their expertise in a specialty area. A variety of nursing organizations offer certification in a number of nursing specialties.7 Certification usually requires a certain amount of clinical experience and successful completion of an examination. Recertification usually requires ongoing clinical experience and continuing education. Common nursing specialties include ambulatory care; cardiovascular care; critical care; women’s health; diabetes education; nursing informatics; and geriatric, medical-surgical, perinatal, emergency, psychiatric/mental health, and community health nursing. Additional formal education and experience can prepare nurses for advanced practice. An advanced practice nurse (APN) or advanced practice registered nurse (APRN) is a nurse with at least a master’s degree in nursing; advanced education in pathophysiology, pharmacology, and health assessment; and expertise in a specialized area of practice. Examples of APNs/APRNs are clinical nurse specialists, clinical nurse leaders, nurse practitioners, nurse midwives, and nurse anesthetists. In addition to managing and delivering direct patient care, APNs/APRNs have roles in health promotion, case management, administration, research, and interdisciplinary health systems.7 Nurses with a PhD typically serve as faculty in schools of nursing, policy analysts, and researchers. However, they are being increasingly employed in clinical settings as clinical experts and health care system executives. In response to patient care needs and in anticipation of the needs of the current and future health care system, the doctorate of nursing practice (DNP) degree was endorsed in 2004 by the American Association of Colleges of Nursing (AACN). The DNP moves the educational preparation for advanced nursing practice from the master’s degree to the doctoral level. It is designed for nurses seeking a practice-focused terminal degree in nursing. The DNP degree moves nursing in the direction of other health professions that offer practice doctorates (e.g., pharmacy [PharmD], psychology [PsyD], and physical therapy [DPT]).8 Health care is a consumer-focused business. Patients today are active participants in their health care and expect high-quality, coordinated, and financially reasonable care. Health information is readily available. Many patients eagerly seek information about their health problems and health care from media and Internet sources. They gather information so that they can have a voice in making decisions about their health care. As a nurse, you must be able to help patients access and use appropriate health care information (Fig. 1-2). These same third-party payers demand outcome-based quality care that is provided at a price affordable for both individuals and society. Payment for health care services or pay-for-performance programs reimburse hospitals for their performance on quality-of-care measures. These measures include clinical outcomes, patient safety, patient satisfaction, adherence to evidence-based practice, and adoption of information technology. Payment for care can be withheld if a patient develops certain health care conditions during a hospital stay (e.g., pressure ulcer) or if something happens to the patient that is considered preventable (e.g., acquiring a catheter-related urinary tract infection).9 For the past 30 years the U.S. government has been active in establishing goals and objectives for promoting health and health care delivery for the nation through an initiative known as Healthy People.10 The vision of Healthy People is a society in which all people live long, healthy lives. Healthy People is a broad-based program that involves government, private, public, and nonprofit organizations. Individuals, groups, and organizations are encouraged to integrate Healthy People goals and focus areas into current programs, special events, publications, and meetings. These activities can further the health of all members of a community. The overarching goals of the Healthy People 2020 initiative are presented in Table 1-1. Healthy People boxes related to these goals are integrated throughout this book. TABLE 1-1 Source: US Department of Health and Human Services: Healthy People 2020. Retrieved from www.healthypeople.gov. The Healthy People initiative is a significant challenge for nursing. Both nursing education programs and clinical nursing practice must respond to major trends in health care. Educational programs for entry-level nurses now place a greater emphasis on health promotion; maintenance; and cost-effective care that responds to the needs of older adults, culturally diverse groups, and underserved populations. Today’s nurses must address the identified health problems, developments in health care delivery, research outcomes, and new technologies in order to meet Healthy People goals. As a reflection of nursing’s contract with society, you are responsible for improving the health status of the public and reducing health disparities. (Health disparities are discussed in Chapter 2.) In 2003 the Institute of Medicine (IOM) commissioned an interdisciplinary task force to study the educational preparation of health care professionals to see whether new graduates were prepared for today’s reality of practice.11 What they found was that all health professions, including nursing, needed to review and revise their curricula and focus on developing specific competencies that serve as a basis for practice. In nursing this is done through a project known as Quality and Safety Education for Nurses (QSEN) (www.qsen.org). QSEN consists of six core competencies: (1) patient-centered care, (2) informatics and technology, (3) evidence-based practice, (4) quality improvement, (5) safety, and (6) teamwork and collaboration. The remainder of this chapter discusses how professional nursing practice is focusing on acquiring the knowledge, skills, and attitudes within each competency. In a primary nursing model, you are responsible for a patient or caseload of patients over a period of time.12 You provide care during assigned shifts, and coordinate and communicate all aspects of patient care with other disciplines and those who provide care when you are absent. Care delivered within a primary care model strengthens the nurse-patient relationship through a focus on continuity of care and interdisciplinary collaboration.
Professional Nursing Practice
Professional Nursing Practice
Domain of Nursing Practice


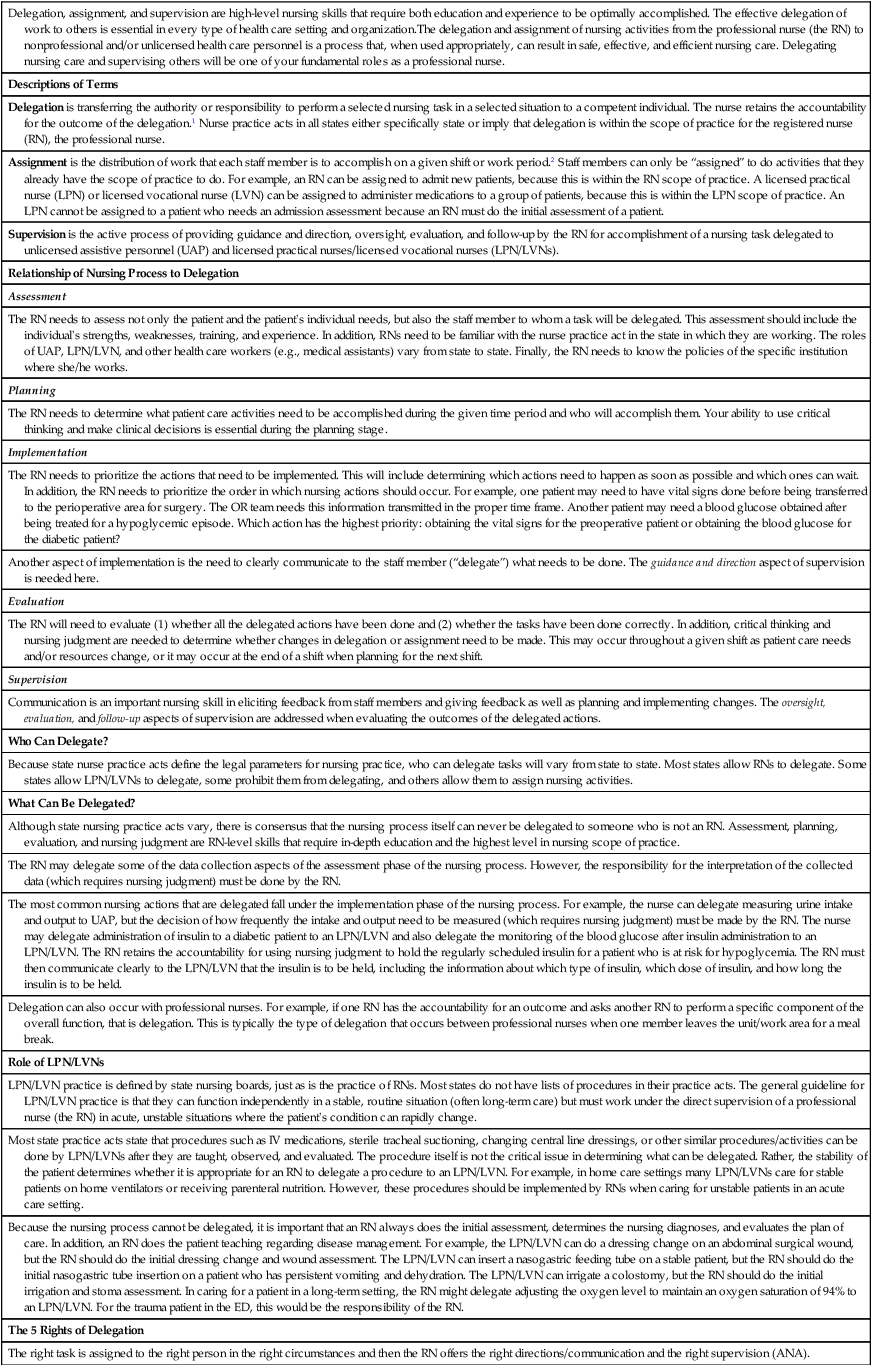
Delegation, assignment, and supervision are high-level nursing skills that require both education and experience to be optimally accomplished. The effective delegation of work to others is essential in every type of health care setting and organization.The delegation and assignment of nursing activities from the professional nurse (the RN) to nonprofessional and/or unlicensed health care personnel is a process that, when used appropriately, can result in safe, effective, and efficient nursing care. Delegating nursing care and supervising others will be one of your fundamental roles as a professional nurse.
Descriptions of Terms
Delegation is transferring the authority or responsibility to perform a selected nursing task in a selected situation to a competent individual. The nurse retains the accountability for the outcome of the delegation.1 Nurse practice acts in all states either specifically state or imply that delegation is within the scope of practice for the registered nurse (RN), the professional nurse.
Assignment is the distribution of work that each staff member is to accomplish on a given shift or work period.2 Staff members can only be “assigned” to do activities that they already have the scope of practice to do. For example, an RN can be assigned to admit new patients, because this is within the RN scope of practice. A licensed practical nurse (LPN) or licensed vocational nurse (LVN) can be assigned to administer medications to a group of patients, because this is within the LPN scope of practice. An LPN cannot be assigned to a patient who needs an admission assessment because an RN must do the initial assessment of a patient.
Supervision is the active process of providing guidance and direction, oversight, evaluation, and follow-up by the RN for accomplishment of a nursing task delegated to unlicensed assistive personnel (UAP) and licensed practical nurses/licensed vocational nurses (LPN/LVNs).
Relationship of Nursing Process to Delegation
Assessment
The RN needs to assess not only the patient and the patient’s individual needs, but also the staff member to whom a task will be delegated. This assessment should include the individual’s strengths, weaknesses, training, and experience. In addition, RNs need to be familiar with the nurse practice act in the state in which they are working. The roles of UAP, LPN/LVN, and other health care workers (e.g., medical assistants) vary from state to state. Finally, the RN needs to know the policies of the specific institution where she/he works.
Planning
The RN needs to determine what patient care activities need to be accomplished during the given time period and who will accomplish them. Your ability to use critical thinking and make clinical decisions is essential during the planning stage.
Implementation
The RN needs to prioritize the actions that need to be implemented. This will include determining which actions need to happen as soon as possible and which ones can wait. In addition, the RN needs to prioritize the order in which nursing actions should occur. For example, one patient may need to have vital signs done before being transferred to the perioperative area for surgery. The OR team needs this information transmitted in the proper time frame. Another patient may need a blood glucose obtained after being treated for a hypoglycemic episode. Which action has the highest priority: obtaining the vital signs for the preoperative patient or obtaining the blood glucose for the diabetic patient?
Another aspect of implementation is the need to clearly communicate to the staff member (“delegate”) what needs to be done. The guidance and direction aspect of supervision is needed here.
Evaluation
The RN will need to evaluate (1) whether all the delegated actions have been done and (2) whether the tasks have been done correctly. In addition, critical thinking and nursing judgment are needed to determine whether changes in delegation or assignment need to be made. This may occur throughout a given shift as patient care needs and/or resources change, or it may occur at the end of a shift when planning for the next shift.
Supervision
Communication is an important nursing skill in eliciting feedback from staff members and giving feedback as well as planning and implementing changes. The oversight, evaluation, and follow-up aspects of supervision are addressed when evaluating the outcomes of the delegated actions.
Who Can Delegate?
Because state nurse practice acts define the legal parameters for nursing practice, who can delegate tasks will vary from state to state. Most states allow RNs to delegate. Some states allow LPN/LVNs to delegate, some prohibit them from delegating, and others allow them to assign nursing activities.
What Can Be Delegated?
Although state nursing practice acts vary, there is consensus that the nursing process itself can never be delegated to someone who is not an RN. Assessment, planning, evaluation, and nursing judgment are RN-level skills that require in-depth education and the highest level in nursing scope of practice.
The RN may delegate some of the data collection aspects of the assessment phase of the nursing process. However, the responsibility for the interpretation of the collected data (which requires nursing judgment) must be done by the RN.
The most common nursing actions that are delegated fall under the implementation phase of the nursing process. For example, the nurse can delegate measuring urine intake and output to UAP, but the decision of how frequently the intake and output need to be measured (which requires nursing judgment) must be made by the RN. The nurse may delegate administration of insulin to a diabetic patient to an LPN/LVN and also delegate the monitoring of the blood glucose after insulin administration to an LPN/LVN. The RN retains the accountability for using nursing judgment to hold the regularly scheduled insulin for a patient who is at risk for hypoglycemia. The RN must then communicate clearly to the LPN/LVN that the insulin is to be held, including the information about which type of insulin, which dose of insulin, and how long the insulin is to be held.
Delegation can also occur with professional nurses. For example, if one RN has the accountability for an outcome and asks another RN to perform a specific component of the overall function, that is delegation. This is typically the type of delegation that occurs between professional nurses when one member leaves the unit/work area for a meal break.
Role of LPN/LVNs
LPN/LVN practice is defined by state nursing boards, just as is the practice of RNs. Most states do not have lists of procedures in their practice acts. The general guideline for LPN/LVN practice is that they can function independently in a stable, routine situation (often long-term care) but must work under the direct supervision of a professional nurse (the RN) in acute, unstable situations where the patient’s condition can rapidly change.
Most state practice acts state that procedures such as IV medications, sterile tracheal suctioning, changing central line dressings, or other similar procedures/activities can be done by LPN/LVNs after they are taught, observed, and evaluated. The procedure itself is not the critical issue in determining what can be delegated. Rather, the stability of the patient determines whether it is appropriate for an RN to delegate a procedure to an LPN/LVN. For example, in home care settings many LPN/LVNs care for stable patients on home ventilators or receiving parenteral nutrition. However, these procedures should be implemented by RNs when caring for unstable patients in an acute care setting.
Because the nursing process cannot be delegated, it is important that an RN always does the initial assessment, determines the nursing diagnoses, and evaluates the plan of care. In addition, an RN does the patient teaching regarding disease management. For example, the LPN/LVN can do a dressing change on an abdominal surgical wound, but the RN should do the initial dressing change and wound assessment. The LPN/LVN can insert a nasogastric feeding tube on a stable patient, but the RN should do the initial nasogastric tube insertion on a patient who has persistent vomiting and dehydration. The LPN/LVN can irrigate a colostomy, but the RN should do the initial irrigation and stoma assessment. In caring for a patient in a long-term setting, the RN might delegate adjusting the oxygen level to maintain an oxygen saturation of 94% to an LPN/LVN. For the trauma patient in the ED, this would be the responsibility of the RN.
The 5 Rights of Delegation
The right task is assigned to the right person in the right circumstances and then the RN offers the right directions/communication and the right supervision (ANA).
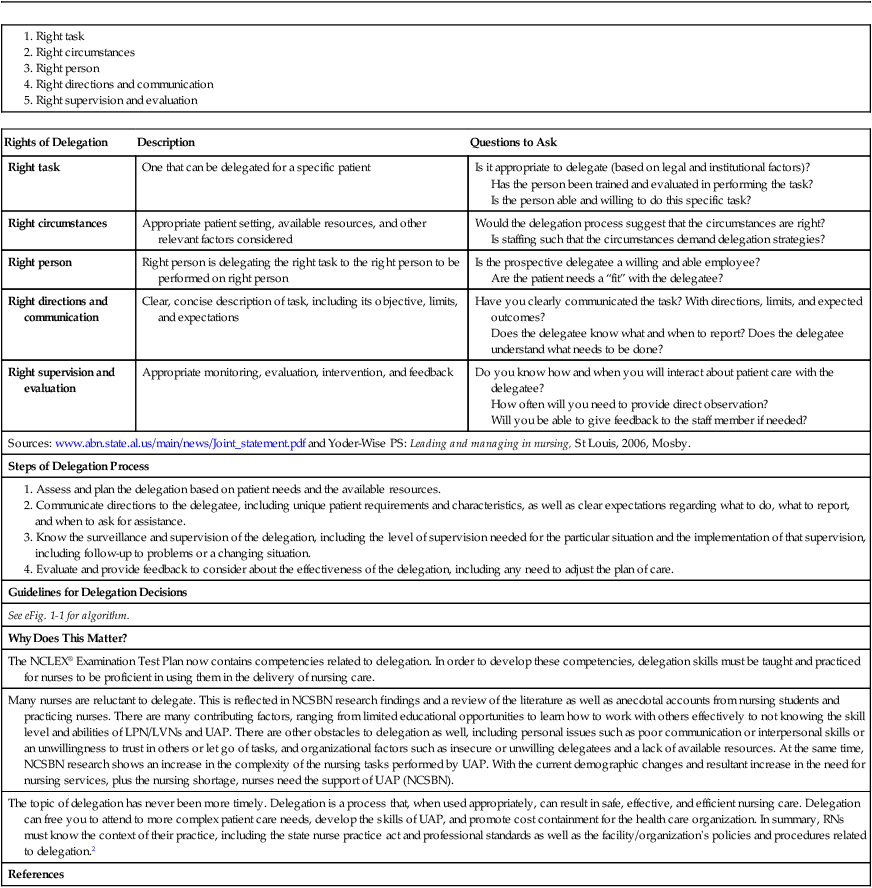
Rights of Delegation
Description
Questions to Ask
Right task
One that can be delegated for a specific patient
Is it appropriate to delegate (based on legal and institutional factors)?
Has the person been trained and evaluated in performing the task?
Is the person able and willing to do this specific task?
Right circumstances
Appropriate patient setting, available resources, and other relevant factors considered
Would the delegation process suggest that the circumstances are right?
Is staffing such that the circumstances demand delegation strategies?
Right person
Right person is delegating the right task to the right person to be performed on right person
Is the prospective delegatee a willing and able employee?
Are the patient needs a “fit” with the delegatee?
Right directions and communication
Clear, concise description of task, including its objective, limits, and expectations
Have you clearly communicated the task? With directions, limits, and expected outcomes?
Does the delegatee know what and when to report? Does the delegatee understand what needs to be done?
Right supervision and evaluation
Appropriate monitoring, evaluation, intervention, and feedback
Do you know how and when you will interact about patient care with the delegatee?
How often will you need to provide direct observation?
Will you be able to give feedback to the staff member if needed?
Sources: www.abn.state.al.us/main/news/Joint_statement.pdf and Yoder-Wise PS: Leading and managing in nursing, St Louis, 2006, Mosby.
Steps of Delegation Process
Guidelines for Delegation Decisions
See eFig. 1-1 for algorithm.
Why Does This Matter?
The NCLEX® Examination Test Plan now contains competencies related to delegation. In order to develop these competencies, delegation skills must be taught and practiced for nurses to be proficient in using them in the delivery of nursing care.
Many nurses are reluctant to delegate. This is reflected in NCSBN research findings and a review of the literature as well as anecdotal accounts from nursing students and practicing nurses. There are many contributing factors, ranging from limited educational opportunities to learn how to work with others effectively to not knowing the skill level and abilities of LPN/LVNs and UAP. There are other obstacles to delegation as well, including personal issues such as poor communication or interpersonal skills or an unwillingness to trust in others or let go of tasks, and organizational factors such as insecure or unwilling delegatees and a lack of available resources. At the same time, NCSBN research shows an increase in the complexity of the nursing tasks performed by UAP. With the current demographic changes and resultant increase in the need for nursing services, plus the nursing shortage, nurses need the support of UAP (NCSBN).
The topic of delegation has never been more timely. Delegation is a process that, when used appropriately, can result in safe, effective, and efficient nursing care. Delegation can free you to attend to more complex patient care needs, develop the skills of UAP, and promote cost containment for the health care organization. In summary, RNs must know the context of their practice, including the state nurse practice act and professional standards as well as the facility/organization’s policies and procedures related to delegation.2
References
Definitions of Nursing
Nursing’s View of Humanity
Scope of Nursing Practice
Influences on Professional Nursing Practice
Complex Health Care Environments
Expanding Knowledge and Technology.
Consumerism.

Influences on Health Care Systems
Health Care Financing.
Healthy People Initiative.
Supporting Professional Practice
Professional Nursing Organizations.
QSEN.
Patient-Centered Care
Delivery of Nursing Care
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access
