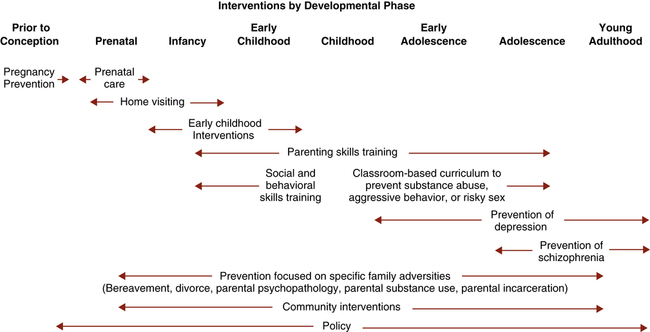
1. Describe the aims and activities of mental health promotion and mental illness prevention. 2. Compare and contrast the public health, medical, and nursing models of primary prevention. 3. Assess the vulnerability of various groups to developing maladaptive coping responses. 4. Analyze the levels of intervention and activities related to the following primary prevention nursing interventions: health education, environmental change, social support, and stigma reduction. 5. Assess the importance of evaluation of the nursing process when applied to primary prevention. Mental and emotional well-being is essential to overall health. In Healthy People 2020 (Healthy People Gov, 2011), mental health is defined in a positive way: For too long the major emphasis in the United States has been on the treatment rather than on the prevention of mental disorders and promotion of mental health. Only recently is prevention emerging as a major force in health care. One of the reasons it is gaining momentum is because the health care system is beginning to provide some economic incentive for preventing illness rather than treating it. Another reason is that it has been found that good mental health improves the quality of life for people with physical illnesses and may contribute to longer life in general (New Freedom Commission on Mental Health [NFCMH], 2003; Centers for Disease Control and Prevention, 2011). • Mental health promotion aims to promote positive mental health by increasing psychological well-being, competence, and resilience and by creating supporting living conditions and environments. • Mental illness prevention has as its goal the reduction of symptoms and ultimately of mental disorders. It uses mental health promotion strategies as one of the means to achieve these goals. The aims of mental health promotion are to enhance an individual’s ability to: • Achieve developmentally appropriate tasks • Acquire a sense of self-esteem, mastery, well-being, and social inclusion Mental health promotion considers mental health as a resource, as a value on its own, and as a basic human right essential to social and economic development. Mental health promotion aims to have an impact on the social determinants of health in order to increase positive mental health, reduce inequalities, build social capital, and narrow the gap in health expectancy between groups (World Health Organization [WHO], 2004). Mental health promotion involves actions to create living conditions and environments that support mental health and allow people to adopt and maintain healthy lifestyles. There is solid research evidence indicating that anxiety, mood (e.g., depression), and impulse control disorders are associated with a higher probability of risk behaviors (e.g., tobacco, alcohol and other drug use, risky sexual behavior), intimate partner and family violence, many other chronic and acute conditions (e.g., obesity, diabetes, cardiovascular disease, HIV/sexually transmitted infections [STIs]), and premature death. Thus, the National Prevention Strategy (Healthy Care Gov, 2011) has identified the following four priorities for mental and emotional well-being: 1. Promote positive early childhood development, including positive parenting and violence-free homes. 2. Facilitate social connectedness and community engagement across the life span. 3. Provide individuals and families with the support necessary to maintain positive mental well-being. 4. Promote early identification of mental health needs and access to quality services. Prevention is often described with slogans such as “An ounce of prevention is worth a pound of cure” or “Curing is costly; prevention is priceless.” Preventive interventions work by focusing on reducing risk factors and enhancing protective factors associated with mental illness (Beardslee et al, 2011). The aims of mental illness prevention are to reduce the: • Incidence, prevalence, and recurrence of mental disorders • Risk factors for developing a mental illness • Impact of the illness in the affected person, their families, and the society A study by the National Research Council and the Institute of Medicine (2009) reviewed the research on the prevention of mental disorders and substance abuse among young people and recommended multiple strategies for enhancing the psychological and emotional well-being of young people. Research demonstrates the value of: • Strengthening families by teaching effective parenting skills, improving communication, and helping families deal with potential problems (such as substance use), disruptions (such as divorce), and adversities (such as parental mental illness or poverty). • Strengthening individuals by building resilience and skills and improving cognitive processes and behaviors. • Promoting mental health in schools by offering support to children encountering serious stresses; modifying the school environment to promote socially adaptive behavior; developing students’ skills at decision making, self-awareness, and conducting relationships; and coping with potential violence, aggressive behavior, and substance use. • Promoting mental health through health care and community programs by promoting and supporting socially adaptive behavior, teaching coping skills, and targeting modifiable lifestyle factors that can affect behavior and emotional health, such as sleep, diet, activity and physical fitness, sunshine and light, and television and computer use. Figure 12-1 shows the developmental phases and the related opportunities for preventive intervention strategies. Box 12-1 lists mental health prevention recommendations made by Healthy People 2020 and the U.S. Preventive Services Task Force 2010-2011. Thus, prevention activities in psychiatric nursing care have five basic aims: • To identify and reduce risk factors for illness • To help people cope with stressors adaptively • To change the resources and policies of the environment so that they do not cause stress but rather enhance people’s functioning In the public health prevention model, the “patient” is the community rather than the individual, and the focus is on the amount of mental health or illness in the community as a whole, including factors that promote or inhibit mental health (Power, 2009). The emphasis in the public health model is on reducing the risk of mental illness for an entire population by providing services to high-risk groups. Use of the public health model requires that mental health professionals be familiar with skills such as community needs assessment, identifying and prioritizing target or high-risk groups, and intervening with treatments such as consultation, education, and crisis intervention. • Social indicators infer need for service from descriptive statistics found in public records and reports, especially statistics that are highly correlated with poor mental health outcomes. Examples of statistics most commonly used are income, race, marital status, population density, crime, and substance abuse. • Key informants are people knowledgeable about the community’s needs. Typical key informants are public officials, clergy, social service personnel, nurses, and primary care physicians. • Community forums invite members of the community to a series of public meetings where they can express their ideas and beliefs about mental health needs in their community. The public health model applies three levels of preventive intervention to mental illness and emotional disturbance (Caplan, 1964): • Primary prevention is lowering the incidence of a mental disorder by reducing the rate at which new cases of a disorder develop. • Secondary prevention involves decreasing the prevalence of a mental disorder by reducing the number of existing cases through early case finding, screening, and prompt, effective treatment. • Tertiary prevention attempts to reduce the severity of a mental disorder and its associated disability through rehabilitative activities. Each of these levels of intervention has implications for psychiatric nursing practice. • Primary prevention is the focus of this chapter. • Secondary prevention is addressed in Chapter 13, “Crisis and Disaster Intervention.” • Tertiary prevention is described in Chapter 14, “Recovery Support.” 1. Identify a disease that warrants the development of a preventive intervention program. Develop reliable methods for its diagnosis so that people can be divided into groups according to whether they do or do not have the disease. 2. Through use of a series of epidemiological and laboratory studies, identify the most likely cause of the disease. 3. Launch and evaluate an experimental preventive intervention program based on the results of those studies. • Acute health problems, such as overdose or delirium tremens • Chronic health problems, such as cirrhosis of the liver • Casualties, such as accidents on the road, in the home, or elsewhere, and suicide • Violent crime and family abuse • Problems of demeanor, such as public drunkenness and use of alcohol by teenagers • Default of major social roles (work or school and family roles) • Problems of feeling state (demoralization, depression, and experienced loss of control) • Assessment: identify risk and protective factors and stressors that may result in maladaptive responses • Planning: identify ways to build resilience, enhance coping and minimize the negative consequences of the stressors • Implementation: apply selected nursing interventions aimed at enhancing adaptation • Evaluation: determine the effectiveness of the nursing interventions based on short- and long-term outcomes, use of resources, and comparison with other prevention strategies Three types of preventive interventions based on target populations have been identified (Mrazek and Haggerty, 1994): 1. Universal: targeted to the general population group without consideration of risk factors 2. Selective: targeted to individuals or groups with a significantly higher risk of developing a particular disorder 3. Indicated: targeted to high-risk individuals identified as having symptoms foreshadowing a specific mental disorder or biological markers indicating predisposition for the disorder The Stuart Stress Adaptation Model presented in Chapter 3 is a useful tool for the nurse that can help in planning strategies for primary prevention. The overall nursing goal is to promote constructive coping mechanisms and maximize adaptive coping responses. Thus prevention strategies should be directed toward influencing predisposing factors, precipitating stressors, appraisal of stressors, coping resources, and coping mechanisms through the following interventions: Competence building is also referred to as resilience. The report of the New Freedom Commission on Mental Health, Achieving the Promise: Transforming Mental Health Care in America (NFCMH, 2003), offers this definition of resilience: Resilience means the personal and community qualities that enable us to rebound from adversity, trauma, tragedy, threats, or other stresses—and to go on with life with a sense of mastery, competence, and hope. We now understand from research that resilience is fostered by positive individual traits, such as optimism, good problem-solving skills, and treatments (Kobau et al, 2011). Closely knit communities and neighborhoods are also resilient, providing supports for their members. Competence building or resilience may be the single most important preventive strategy. A competent individual or community is aware of resources and alternatives, can make informed decisions about issues, and can cope adaptively with problems. Coping in the face of adversity involves emotional intelligence and resilience, both of which can be developed through support and education (Luthar, 2008). Other clinical strategies include early intervention and promoting a social and familial climate, self-esteem, support building, and social/life and vocational skills. Four categories of resilience strengths are presented in Box 12-2.
Prevention and Mental Health Promotion
Promotion and Prevention
Mental Health Promotion
Mental Illness Prevention
Public Health Prevention Model
Community Needs Assessment
Interventions
Medical Prevention Model
Nursing Prevention Model
Assessment
Risk Factors and Protective Factors
Target Populations
Planning and Implementation
Health Education