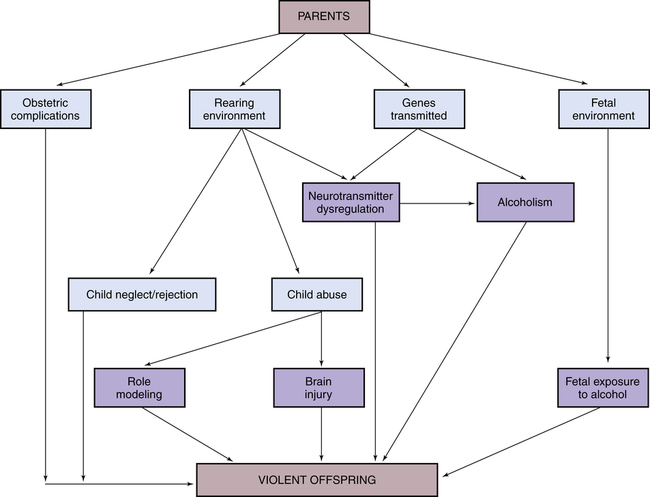
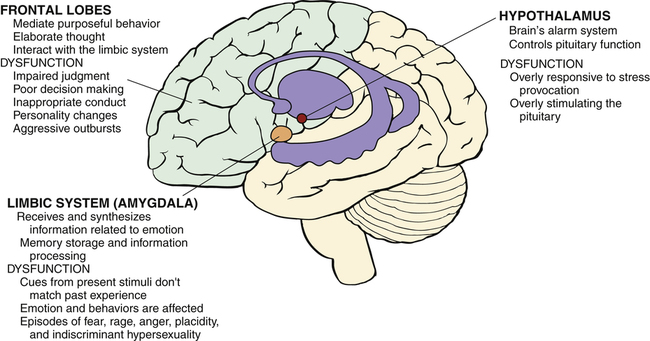
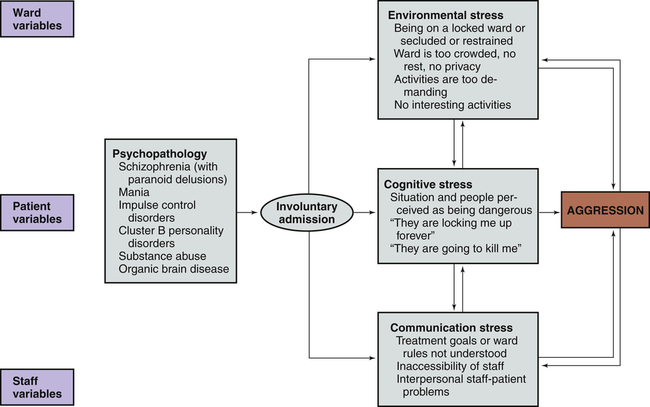
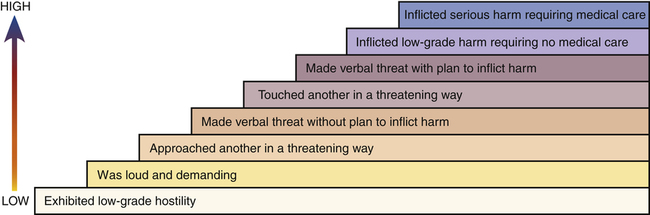
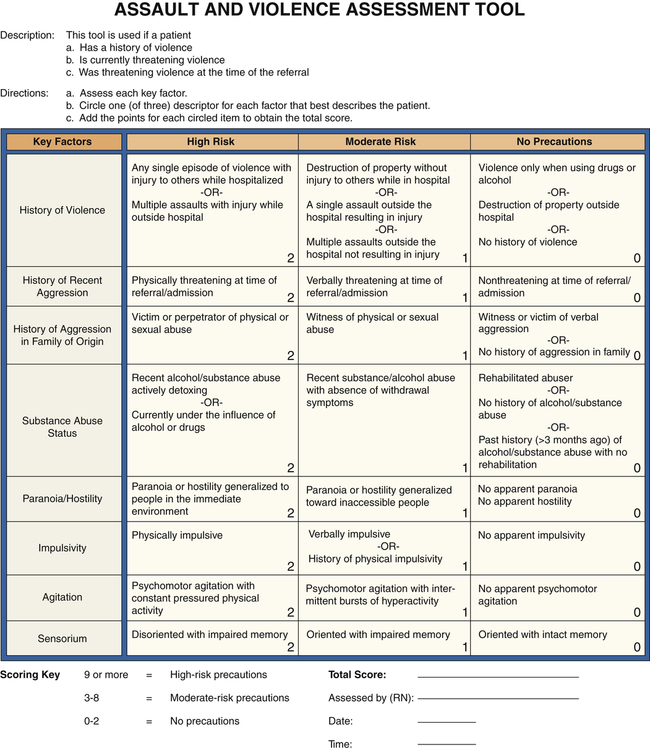
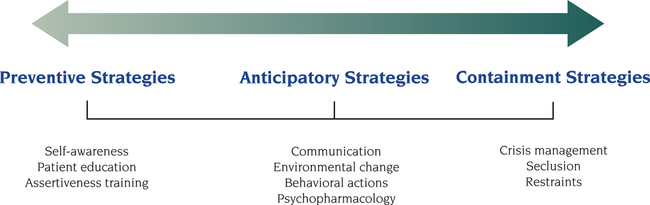
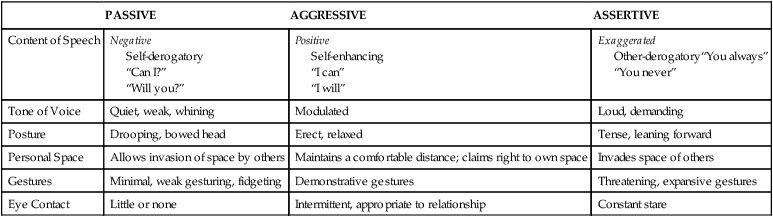
1. Compare passive, assertive, and aggressive behavioral responses. 2. Describe theories on the development of aggressive behavior. 3. Identify factors useful in predicting aggressive behavior among psychiatric patients. 4. Assess patients for aggressive behavioral responses. 5. Analyze nursing interventions for preventing and managing aggressive behavior. 6. Develop a patient education plan to promote patients’ appropriate expression of anger. 7. Describe the implementation of crisis management techniques. 8. Evaluate prevention strategies related to the workplace, including addressing lateral violence and staff education and support. People who enter the health care system are often in great distress and may exhibit maladaptive coping responses. Nurses who work in settings such as emergency departments (EDs), critical care areas, and trauma centers often care for people who respond to events with angry and aggressive behavior that can pose a significant risk to themselves, other patients, and health care providers (Lanza et al, 2009). Thus, preventing and managing aggressive behavior are important skills for all nurses. Violence against ED nurses is common, with reports of 25% to 50% of ED nurses reporting that they have experienced physical violence (Gacki-Smith et al, 2009). Psychiatric nurses also are at risk for violence as they work with patients who have inadequate coping mechanisms for dealing with stress. Patients admitted to an inpatient psychiatric unit are usually in crisis and not thinking clearly, so their coping skills are even less effective. During these times of stress, acts of physical aggression or violence can occur. 1. Passive and fearful and to flee 2. Aggressive and angry and to fight 3. Assertive and self-confident and to confront the situation directly The situation and the characteristics of the people involved determine the appropriate response. Table 28-1 summarizes the major characteristics of passive, aggressive, and assertive behaviors. TABLE 28-1 COMPARISON OF PASSIVE, ASSERTIVE, AND AGGRESSIVE BEHAVIORS The psychological view of aggressive behavior suggests the importance of predisposing developmental factors or life experiences that limit the person’s ability to use nonviolent coping mechanisms. Some of these experiences are listed in Box 28-1. They may limit a person’s ability to use supportive relationships, leave the person very self-centered, or make the person particularly vulnerable to a sense of injury that can easily be provoked into rage. Figure 28-1 shows how these factors can contribute to an intergenerational transmission of violent behavior. Box 28-2 presents background information about the patient that also may be associated with violence. • Patients with active psychotic symptoms. In particular, those patients who have symptoms related to a perceived threat or an overriding of internal controls, such as delusions of thought control, are at increased risk of committing violence. • Patients with substance abuse disorders. The prevalence of violence is 12 times greater for those with alcohol abuse or dependence and 16 times greater for those with other drug dependence compared with those who have no psychiatric diagnosis. Co-morbid substance abuse has an added effect in increasing the risk of violence for people with major psychiatric disorders. Situational and environmental factors also are important in escalating patient behavior from dangerous to violent. These factors include aspects of the physical facilities and the presence of staff and other patients (Hamrin et al, 2009). Several studies have found that the number of violent incidents is greater when patients move or gather in groups, are overcrowded, lack privacy, or are inactive. Clinicians may intentionally or inadvertently precipitate an outbreak of violence because staff attitudes and actions have a powerful impact on patient behavior. Inexperienced staff, provocation by staff, poor milieu management, understaffing, close physical encounters, inconsistent limit setting, and a norm of violence may all negatively affect the inpatient environment (Knutzen et al, 2011). Finally, a patient’s appraisal of a situation and level of perceived stress affect one’s response. When an environment is interpreted as hostile, the response is likely to be hostile in return. Those with psychiatric illness, substance abuse, past traumatic experiences, or brain damage may have distorted perceptions that can lead to aggressive responses. A model for the development of aggression in inpatient settings that incorporates these various factors is presented in Figure 28-3. Accurate prediction of patient violence is not possible. For this reason it is important for psychiatric nurses to be alert for symptoms of increasing agitation that could lead to violent behavior (Box 28-3). Using a hierarchy of aggressive behaviors (Figure 28-4) in which lower levels of aggression may lead to more violent behavior is helpful in evaluating patients. Some of these early behaviors include motor agitation, such as pacing, inability to sit still, clenching or pounding fists, and tightening of jaw or facial muscles. Verbal clues also may be present, such as threats to real or imagined objects, intrusive demands for attention or swearing (Stone et al, 2011). Speech may be loud and pressured, and posture may become threatening. In summary, psychiatric nurses should carefully assess all patients for their potential for violence. A screening or assessment tool can be particularly useful (Fluttert et al, 2011). One such tool is presented in Figure 28-5. Once completed, a violence assessment tool can help the nurse do the following: The nurse can implement a variety of interventions to prevent and manage aggressive behavior. These interventions can be thought of as existing on a continuum (Figure 28-6). They range from preventive strategies, such as self-awareness, patient education, and assertiveness training, to anticipatory strategies, such as verbal and nonverbal communication, environmental changes, behavioral interventions, and the use of medications. If the patient’s aggressive behavior escalates despite these actions, the nurse may need to implement crisis management techniques and containment strategies, such as seclusion or restraints. When dealing with potentially aggressive patients it is important to be able to assess the situation objectively despite the positive or negative countertransference that might be present. Countertransference is an emotional reaction of the nurse to some aspect or behavior of the patient (Chapter 2). Both positive and negative countertransference reactions may lead to nontherapeutic responses on the part of the staff. Ongoing self-awareness and supervision can assist the nurse in ensuring that patient needs, rather than personal needs, are addressed. Teaching patients about communication and the appropriate way to express anger can be one of the most successful interventions in preventing aggressive behavior (Table 28-2). Many patients have difficulty identifying their feelings, needs, and desires and even more difficulty communicating these to others. Thus, teaching healthy anger management skills is an important area of nursing intervention. TABLE 28-2 PATIENT EDUCATION PLAN Teaching patients that feelings are not right or wrong or good or bad can allow them to explore feelings that may have been bottled up, ignored, or repressed. The nurse can then work with patients on ways to express their feelings and evaluate whether the responses they select are adaptive or maladaptive (Son and Choi, 2010). Providing patients with available choices in managing anger, such as those listed in Box 28-4, may be effective in reducing more restrictive interventions. Assertive behavior is a basic interpersonal skill that includes the following:
Preventing and Managing Aggressive Behavior
Behavioral Responses
Assertive Behavior
PASSIVE
AGGRESSIVE
ASSERTIVE
Content of Speech
Negative
Self-derogatory
“Can I?”
“Will you?”
Positive
Self-enhancing
“I can”
“I will”
Exaggerated
Other-derogatory“You always”
“You never”
Tone of Voice
Quiet, weak, whining
Modulated
Loud, demanding
Posture
Drooping, bowed head
Erect, relaxed
Tense, leaning forward
Personal Space
Allows invasion of space by others
Maintains a comfortable distance; claims right to own space
Invades space of others
Gestures
Minimal, weak gesturing, fidgeting
Demonstrative gestures
Threatening, expansive gestures
Eye Contact
Little or none
Intermittent, appropriate to relationship
Constant stare
Theories on Aggression
Psychological
Predicting Aggressive Behavior
Nursing Assessment
Nursing Interventions
Self-Awareness
Patient Education
Appropriate Expression of Anger
CONTENT
INSTRUCTIONAL ACTIVITIES
EVALUATION
Help the patient identify anger.
Focus on nonverbal behavior.
Role play nonverbal expression of anger.
Label the feeling using the patient’s preferred words.
Patient demonstrates an angry body posture and facial expression.
Give permission for angry feelings.
Describe situations in which it is normal to feel angry.
Patient describes a situation in which anger would be an appropriate response.
Practice the expression of anger.
Role play fantasized situations in which anger is an appropriate response.
Patient participates in role playing and identifies behaviors associated with expression of anger.
Apply the expression of anger to a real situation.
Help identify a real situation that makes the patient angry.
Role play a confrontation with the object of the anger.
Provide positive feedback for successful expression of anger.
Patient identifies a real situation that results in anger.
Patient is able to role play expression of anger.
Identify alternative ways to express anger.
List several ways to express anger, with and without direct confrontation.
Role play alternative behaviors.
Discuss situations in which alternatives would be appropriate.
Patient participates in identifying alternatives and plans when each might be useful.
Confront a person who is a source of anger.
Provide support during confrontation if needed.
Discuss experience after confrontation takes place.
Patient identifies the feeling of anger and appropriately confronts the object of the anger.
Assertiveness Training
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Preventing and Managing Aggressive Behavior
Get Clinical Tree app for offline access