CHAPTER 13 The sympathetic nervous system has three main functions: • Maintenance of blood flow to the brain • Redistribution of blood flow during exercise • Compensation for loss of blood, primarily by causing vasoconstriction • Increasing heart rate and blood pressure • Shunting blood away from the skin and viscera and into skeletal muscles • Dilating the bronchi to improve oxygenation • Dilating the pupils (perhaps to enhance visual acuity) • Mobilizing stored energy, thereby providing glucose for the brain and fatty acids for muscles In many organs that receive dual innervation, the influence of sympathetic nerves opposes that of parasympathetic nerves. For example, in the heart, sympathetic nerves increase heart rate, whereas parasympathetic nerves slow heart rate (Fig. 13–1). In summary, there are three basic patterns of autonomic innervation and regulation: • Innervation by both divisions of the autonomic nervous system in which the effects of the two divisions are opposed • Innervation by both divisions of the autonomic nervous system in which the effects of the two divisions are complementary • Innervation and regulation by only one division of the autonomic nervous system Figure 13–2 depicts a feedback loop typical of those used by the autonomic nervous system. The main elements of this loop are (1) a sensor, (2) an effector, and (3) neurons connecting the sensor to the effector. The purpose of the sensor is to monitor the status of a physiologic process. Information picked up by the sensor is sent to the central nervous system (spinal cord and brain), where it is integrated with other relevant information. Signals (instructions for change) are then sent from the central nervous system along nerves of the autonomic system to the effector. In response to these instructions, the effector makes appropriate adjustments in the process. The entire procedure is called a reflex. Feedback (reflex) control of blood pressure is achieved as follows: (1) Baroreceptors located in the carotid sinus and aortic arch monitor changes in blood pressure and send this information to the brain. (2) In response, the brain sends impulses along nerves of the autonomic nervous system, instructing the heart and blood vessels to behave in a way that restores blood pressure to normal. Accordingly, when blood pressure falls, the baroreceptor reflex causes vasoconstriction and increases cardiac output. Both actions help bring blood pressure back up. Conversely, when blood pressure rises too high, the baroreceptor reflex causes vasodilation and reduces cardiac output, thereby causing blood pressure to drop. The baroreceptor reflex is discussed in greater detail in Chapter 43 (Review of Hemodynamics). Although we know a great deal about the anatomy of the peripheral nervous system, very little of this information helps us understand peripheral nervous system drugs. The few details that do pertain to pharmacology are summarized in Figure 13–3. Pharmacologically relevant aspects of parasympathetic anatomy are shown in Figure 13–3. Note that there are two neurons in the pathway leading from the spinal cord to organs innervated by parasympathetic nerves. The junction (synapse) between these two neurons occurs within a structure called a ganglion. (A ganglion is simply a lump created by a group of nerve cell bodies.) Not surprisingly, the neurons that go from the spinal cord to the parasympathetic ganglia are called preganglionic neurons, whereas the neurons that go from the ganglia to effector organs are called postganglionic neurons. The anatomy of the parasympathetic nervous system offers two general sites at which drugs can act: (1) the synapses between preganglionic neurons and postganglionic neurons and (2) the junctions between postganglionic neurons and their effector organs. Pharmacologically relevant aspects of sympathetic nervous system anatomy are illustrated in Figure 13–3. As you can see, these features are nearly identical to those of the parasympathetic nervous system. Like the parasympathetic nervous system, the sympathetic nervous system employs two neurons in the pathways leading from the spinal cord to organs under its control. As with the parasympathetic nervous system, the junctions between those neurons are located in ganglia. Neurons leading from the spinal cord to the sympathetic ganglia are termed preganglionic neurons, and neurons leading from ganglia to effector organs are termed postganglionic neurons. Pharmacologically relevant anatomy of the somatic motor system is depicted in Figure 13–3. Note that there is only one neuron in the pathway from the spinal cord to the muscles innervated by somatic motor nerves. Because this pathway contains only one neuron, peripherally acting drugs that affect somatic motor system function have only one site of action: the neuromuscular junction (ie, the junction between the somatic motor nerve and the muscle). To understand peripheral nervous system pharmacology, it is necessary to know the identity of the transmitter employed at each of the junctions of the peripheral nervous system. This information is summarized in Figure 13–4. As indicated, acetylcholine is the transmitter employed at most junctions of the peripheral nervous system. Acetylcholine is the transmitter released by (1) all preganglionic neurons of the parasympathetic nervous system, (2) all preganglionic neurons of the sympathetic nervous system, (3) all postganglionic neurons of the parasympathetic nervous system, (4) all motor neurons to skeletal muscles, and (5) most postganglionic neurons of the sympathetic nervous system that go to sweat glands. Much of what follows in this chapter is based on the information summarized in Figure 13–4. Accordingly, I strongly urge you to learn (memorize) this information now. Not all cholinergic receptors are the same; likewise, not all adrenergic receptors are the same. For each of these two major receptor classes there are receptor subtypes. There are three major subtypes of cholinergic receptors, referred to as nicotinicN, nicotinicM, and muscarinic.* And there are four major subtypes of adrenergic receptors, referred to as alpha1, alpha2, beta1, and beta2.
Physiology of the peripheral nervous system
Overview of autonomic nervous system functions
Functions of the sympathetic nervous system
Basic mechanisms by which the autonomic nervous system regulates physiologic processes
Patterns of innervation and control
Feedback regulation
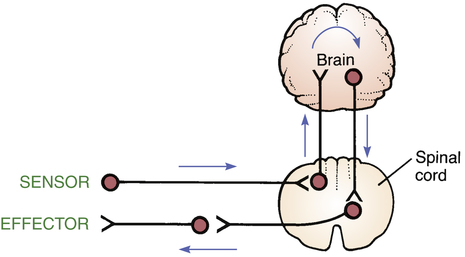
 Feedback loop of the autonomic nervous system.
Feedback loop of the autonomic nervous system.
Baroreceptor reflex.
Anatomic considerations
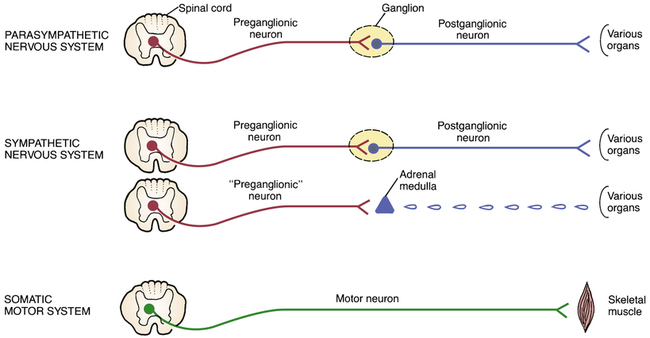
 The basic anatomy of the parasympathetic and sympathetic nervous systems and the somatic motor system.
The basic anatomy of the parasympathetic and sympathetic nervous systems and the somatic motor system.
Parasympathetic nervous system
Sympathetic nervous system
Somatic motor system
Introduction to transmitters of the peripheral nervous system
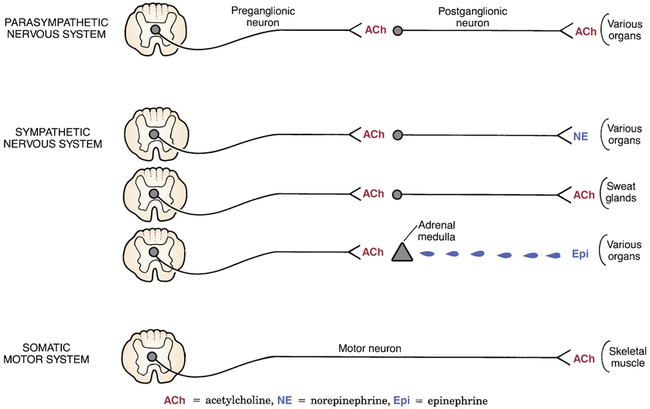
 Transmitters employed at specific junctions of the peripheral nervous system.
Transmitters employed at specific junctions of the peripheral nervous system.
Summary:
1.All preganglionic neurons of the parasympathetic and sympathetic nervous systems release acetylcholine as their transmitter.
2.All postganglionic neurons of the parasympathetic nervous system release acetylcholine as their transmitter.
3.Most postganglionic neurons of the sympathetic nervous system release norepinephrine as their transmitter.
4.Postganglionic neurons of the sympathetic nervous system that innervate sweat glands release acetylcholine as their transmitter.
5.Epinephrine is the principal transmitter released by the adrenal medulla.
6.All motor neurons to skeletal muscles release acetylcholine as their transmitter.
Introduction to receptors of the peripheral nervous system
Subtypes of cholinergic and adrenergic receptors
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Physiology of the peripheral nervous system
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access


