2Children’s Respiratory/Community Nurse Specialist, Nottingham Children’s Hospital
- pharmacodynamics
- respiratory drug therapy
- the importance of monitoring patients for unwanted effects
- the nurse’s role in drug administration.
Introduction
Safe, effective prescribing and administration of medications is a cornerstone of good practice. There are several important references with which all practitioners should be familiar. The British National Formulary for Children (BNFc; Royal Pharmaceutical Society 2011) is the single most important reference in the UK at present. Additional guidance is also available from the National Institute for Health and Clinical Excellence (NICE). Locally, most institutions have their own guidelines, usually for specific groups of patients such as those with cystic fibrosis or those on intensive care.
Prescribing and administration guidelines allow for the safe administration of medicines. There is increased risk with prescribing for children, because many medications are relatively understudied in children, and also doses require adjustment for each child (usually according to their age or weight). Pharmacology is the study of the modes of action, effects and side-effects and uses of drugs (Neal 2005). An understanding of pharmacology is essential to the safe prescription and administration of drugs.
How drugs work
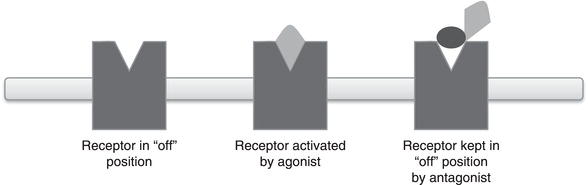
The ideal drug is usually one which has a specific action on a specific organ to do a specific job with minimal side-effects or toxicity. So, after administration of the drug, it has to be transported through the body to the target organ (or, in the case of some respiratory medicines, it is administered directly to the lungs). At the target organ, the drug binds with a component of the organ’s cellular machinery (often a specific protein or cell surface receptor). This binding causes the drug’s effect. A receptor can be thought of as a kind of biological switch which turns a process in a cell on or off. A drug which turns a receptor on is an agonist, and one which blocks a receptor, stopping it from being turned on, is an antagonist (Figure 9.1). After binding, the drug is often metabolised into breakdown products, and following this the drug is excreted from the body.
Figure 9.1 Schematic of agonist and antagonist action. Receptors can be located on the cell surface or within the cell. An agonist binds to the receptor and activates it, turning on a process within the cell. An antagonist binds to the receptor and prevents the body’s natural agonists from activating the receptor.
Absorption
Absorption is the process by which a drug passes from the site of administration (often the gastrointestinal tract after being taken orally) into the bloodstream. For orally administered drugs, the small intestine is usually the site of absorption. Intravenous drugs are administered directly into the bloodstream and do not require absorption.
A key feature of absorption is that not all the drug administered by the oral route will be absorbed – some will pass directly through the gut without interacting with the body. The fraction of the drug which is absorbed is termed its bioavailability. Many intravenous drugs are given via the intravenous route because their oral bioavailability is low. Aminoglycoside antibiotics are an example of these. Oral absorption is slow and so the onset of action of oral drugs occurs after an equivalent dose of an intravenous drug. So if rapid analgesia is required, intravenous preparations of morphine are preferred over oral morphine.
Oral drugs are generally absorbed over 1–3 h but gut absorption is affected by foods given at the same time as the drugs, largely due to the effect of food on gut motility (the speed at which things pass through the gut) and the acid content of the stomach.
Distribution
After passing into the blood, a drug is then distributed through the various tissues of the body. Drugs are rarely evenly distributed between body tissues – for example, some antibiotic drugs do not penetrate into the brain, and some antibiotics such as gentamicin are actively taken up into the kidneys.
Metabolism
Metabolism occurs when the body chemically alters a drug into metabolites. These metabolites are often easier to excrete from the body. The process of metabolism changes the chemical structure of the drug, and often this means that the metabolites do not have the same properties as the original drug. The liver is usually the site of metabolism.
Some metabolism of a drug can occur before it gets into the body’s circulation for orally administered drugs. After being absorbed in the gastrointestinal tract, the drug enters the portal veins which drain into the liver. Some drug is metabolised in the liver as the drug passes through it, reducing the amount of blood which gets into the systemic circulation. This is termed ‘first-pass metabolism’ and it reduces the bioavailability of orally administered drugs (Rang et al. 2007).
Elimination
Most drugs are removed from the body by the kidneys. Some drugs can be excreted by the lungs, for example gaseous anaesthetic agents administered during a general anaesthetic. Drugs can be removed in the urine in their original form, such as gentamicin, which has an increased risk of toxicity and has been shown to cause damage to the kidneys (Bertenshaw et al. 2007; Detlef et al. 2009). However, often only their metabolites are removed by the kidneys.
The kidneys and liver are important for drug metabolism and elimination
As most drugs are metabolised by the liver and most are excreted by the kidneys, decreased kidney and liver function can lead to accumulation of drugs in the body. For this reason, dosages of drugs are often adjusted for patients with kidney damage or liver failure.
At different ages, children’s kidney and liver function varies. For example, preterm neonates have low kidney function compared to term infants. For this reason drug doses are adjusted not just for weight but also for the age of the child.
The inhaled route of drug administration
Many therapies given in respiratory practice need to get to the lungs to effect their action. For example, salbutamol is given in asthma to dilate the airways, improving airflow and gas exchange in the lung. The site of action of salbutamol is a cell surface receptor called the β2-receptor. In the lungs, activation of the β2-receptor causes bronchodilation. β-Receptors are also present in the heart, where activation of the receptor causes the heart rate to increase. Salbutamol is usually given by the inhaled route, as it gets directly to the site where it is needed in the lungs. This allows low doses to be used. Some drug does get absorbed via the lungs into the bloodstream but because the dose given is low, very little gets to the heart, so tachycardia (a side-effect) is minimised. In contrast, if inhaled salbutamol is not effective for an asthma attack, a salbutamol infusion is often given. This requires a higher dose (as not all the drug will be distributed to the lungs) and so more drug gets to the heart, and the tachycardia is greater with the intravenous route.
Because many children cannot co-ordinate their breathing, inhaled drugs from an inhaler are usually given with a spacer. Nebulised therapies are usually delivered in hospital, although some patients such as those with cystic fibrosis receive nebulised therapies at home.
Frequently administered respiratory drugs
A comprehensive discussion of respiratory drugs prescribed for children is beyond the scope of this chapter. However, an outline of several respiratory drugs may be helpful.
In asthma, therapy is geared towards minimising inflammation and bronchoconstriction (narrowing of the airways). Patients are usually prescribed a bronchodilator such as salbutamol or ipratropium bromide, which temporarily dilates the airways. Longer acting bronchodilators are also given, such as salmeterol. Oral therapies can also be given such as theophylline and montelukast. Montelukast is a leucotriene receptor antagonist (an antagonist turns off a receptor). It prevents leucotrienes from interacting with their receptor. Their normal job seems to be to turn on inflammation, so by inhibiting their receptor, montelukast reduces inflammation.
Inhaled corticosteroids are frequently used in asthma, to reduce the symptoms between an asthma attack and the risk of an asthma attack. They reduce inflammation in the lung. Frequently prescribed inhaled steroids are beclomethasone, budesonide and fluticasone. There are many side-effects of inhaled steroids and for this reason, the dose is often adjusted up or down when the patient is seen in clinic to get the best response with the smallest dose. Oral steroids are used with some caution as their side-effect profile is much more severe than that of inhaled steroids (Sharek and Bergman 2000). However, oral steroids are highly effective when given as a short course for an asthma attack.
Oral antibiotics are frequently administered for pneumonia. Intravenous antibiotics are usually reserved for patients who require oxygen or those who are not tolerating oral antibiotics, for example due to vomiting. Paracetamol is frequently given for fever associated with chest infections but this is to relieve symptoms rather than to treat the underlying infection.
Patients with cystic fibrosis (CF) receive numerous medications, including nebulised antibiotics, nebulised sputum mucolytics (such as dornase), nebulised hypertonic saline, oral antibiotics and intravenous antibiotics. They are frequently admitted to hospital for a period of intensive antibiotic therapy, physiotherapy and dietetic and specialist nursing care. Due to the polypharmacy involved (numerous drugs given at the same time), extra care needs to be taken with their prescriptions. Children with CF often require different dosages of drugs compared to other patient groups. Many units will have their own guidelines.
Some of these drugs need careful monitoring of drug levels; in particular, aminoglycosides such as tobramycin and gentamicin (which is less frequently used in CF) require blood level monitoring. If levels are too high, kidney damage (nephrotoxicity) is a risk, and even with careful monitoring nephrotoxicity can still occur.
The nurse’s role in drug administration
The Nursing and Midwifery Council (NMC 2010) clearly outlines the professional responsibility and accountability of practitioners when administering medicines; it is ‘not solely a mechanistic task. It requires thought and professional judgement’ (p. 1). Although training provides the basis for safe drug administration, it is ultimately the responsibility of each professional to adhere to their local policy.
Human factors will no doubt contribute to errors with drug administration so the Department of Health (Department of Health 2004) suggests that practitioners should take into account the ‘five rights’ of safe drug administration (Box 9.1). Adopting this approach ensures that practitioners provide safe and accurate care. Local policy also supports and incorporates the principle of the ‘five rights’ in order to carry out all the necessary checks of the drug administration process listed in Table 9.1.
When administering medicines to children, it is important to get co-operation from the child but equally important is the need to involve the family (Trounce et al. 2004). It is also important to acknowledge other considerations such as the significance of correct doses in children and the need to adhere to local medicines administration policy. These points are outlined in Table 9.1. It is also good practice to question prescribers and clarify the correct dose to be given before administration to children (Trounce et al. 2004).
Pharmacology training for nurses is now an integral part of the modern health service. This enables nurse prescribers to work closely with other healthcare professionals locally in support of their extended role, such as specialist pharmacists when appropriate (Trounce et al. 2004). It is also good practice for all nurses, irrespective of their level of knowledge, to acknowledge the need to check drug doses with the BNFc on every occasion before administration, as a safety mechanism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


