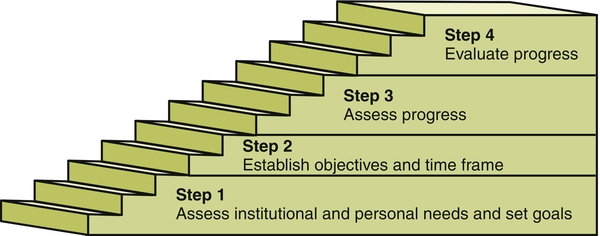
Performance is defined as the execution of an action; something accomplished; the fulfillment of a promise, claim, or request (www.merriam-webster.com, 2012). Performance appraisal means evaluating the work of others. It is the process by which a manager examines and evaluates an employee’s work behavior by comparing it with preset standards, documents the results of the comparison and uses the results to provide feedback to the employee to show where improvements are needed and why (www.businessdictionary.com, 2012). The employee’s work is measured against standards, much like the quality improvement process. Standards, whether explicit or not, are applied to what ought to be or to what is superior, excellent, average, or unacceptable performance. Peer review in nursing (defined in 1988 by the American Nurses Association and still applicable today) is the process by which nurses systematically evaluate the quality of nursing care provided by peers as measured against professional standards (American Nurses Association, 1988, p. 3). The process of performance appraisal includes assessing needs and setting goals, establishing objectives and time frames, assessing progress and evaluating performance, and then starting over again (Figure 23-1). At the start of a new job, core competencies (knowledge and skills) of the individual need to be evaluated. During the orientation program, progress should be tracked, and competence needs should be reassessed periodically throughout employment, at least annually. The employee’s work is measured against some standard for the purpose of determining the level of quality of the job performance. The guides to evaluation criteria include governmental standards such as Medicare/Medicaid regulations, professional standards published by the American Nurses Association or other specialty organizations, nursing care audits, client feedback in various forms, evidence-based guidelines, and departmentally developed standards. Organizational standards are more prevalent as systems undertake service and operational excellence initiatives to improve customer service, the employee experience, quality, financial performance, and growth. Organizational pillars to “hardwire excellence” provide a platform for all employees to understand and buy into the mission, vision, and values of the organization (Studer, 2003). Ideally, a performance appraisal measures performance and motivates the person. However, performance appraisal is not the only or major source of motivation for most nurses. Measuring performance is not easy, and motivating someone else is an art. Cultural sensitivity is important to consider as the nursing workforce becomes more diversified (Smith-Trudeau, 2008). The performance appraisal process can create a lot of stress for individuals if it is not managed well by both the manager and the employee (Duncan, 2007). For example, job satisfaction and organizational commitment were found to be positively correlated to satisfaction with the feedback from performance appraisals (Jawahar, 2006). Integral components of a comprehensive performance appraisal system provide an overarching framework for the process. The tools and methods for a comprehensive performance appraisal system involve a clear determination of the abilities required for the position (job description); a match of the key requirements for the position with the individual’s capabilities (personnel selection); development of the abilities of the employee (staff development); and use of a motivational reward system to enhance employee performance (reward system). Box 23-1 outlines the key components of the performance appraisal process. Performance attributes of an individual are determined by two elements: ability and motivation. Ability is made up of a collection of physical and mental capacities that enable a person to exhibit a skill or set of skills. Knowledge, experience, and skill form the ability to successfully complete a task (Hersey et al., 2008). Thus ability is an innate capacity that is molded by experience and training. Motivation is a willingness to work and a desire to achieve. Given the national concerns about patient safety and quality of care, it is important to look at organizational culture as a factor influencing performance appraisal for change and improvement. The change of an error-prone health care system involves leadership and organizational learning, which requires significant strategic commitment and administrative direction. An environment that values and creates a shared vision and purpose can lead to reflection and learning, which then enables and strengthens organizational culture toward creative and effective solutions in health care delivery (Carroll & Edmondson, 2002). Culture consists of shared norms, behaviors, and values. Schein (1992) defined the culture of a group as “a pattern of shared basic assumptions that the group learned as it solved its problems of external adaptation and internal integration, that has worked well enough to be considered valid and, therefore, to be taught to new members as the correct way to perceive, think, and feel in relation to those problems” (p. 12). The learning that occurs within the system over time influences organizational culture. The quality of care and the quality of work life are driven by the culture within a health care organization (Gershon et al., 2004). Culture is reflected in “the way things are done” in an organization (Stetler, 2003), and it surrounds all individuals and influences leadership. Characteristics of the culture are manifested differently in subgroups and by the various stakeholders within the organization, which warrants more in-depth assessment to fully understand. Socialization of new members into an organization is an important way to learn the rules and norms of a group. New members need to learn the assumptions of the group, which are not always transparent. Group behaviors and perceptions may reveal some elements of the culture, and some of the rituals and processes undertaken within the organization may reflect the assumptions that are held. Groups that are stable and have a history of shared learning are likely to have developed some degree of culture, but groups with significant turnover of members and leaders may lack shared assumptions (Schein, 1992). Organizational culture has been referred to as the social glue that binds the organization, in which the deeper meanings of the way things are done in the organization are learned (Cameron & Quinn, 1999; Detert et al., 2000). Evaluation of organizational culture needs to consider both the larger organization and the smaller unit within which a member belongs. Exploring the microsystem within a health care system reveals the unique disciplinary focus of each department and treatment setting (Donaldson & Mohr, 2000). The performance characteristics of academic departments, clinics, and hospital units and departments highlight the different functions and shared assumptions that members bring to the patient care setting. These varying perspectives enrich the mix of the organization by enabling diverse contributions, attitudes, and skills to be developed. The most direct goal of any performance appraisal system is the improvement of performance. Considering the process of performance appraisal systems, the outcome for the system should lead to positive organizational outcomes. Used effectively, the performance appraisal offers the opportunity for numerous organizational goals to be achieved. Box 23-2 provides an overview of the goals of the process of performance appraisal. Leaders who reward positive behavior and punish individuals who behave negatively in the workplace practice transactional leadership. By shifting toward a transformational style of leadership, organizational learning can occur from errors and system issues, and an empowered staff of nurses can work toward the innovations needed in the health care system (Wenberg, 2010). Self-appraisal as an important component in the appraisal process and promotes individual input, personal responsibility, and feedback regarding job performance. Appraisal is a structured process of facilitated self-reflection, which allows individuals to review their professional activities comprehensively and to identify areas of real strength, professional goals, and needs for development (Conlon, 2003). Managers who create a healthy work environment offer adequate time for feedback and input. Audit and feedback are important mechanisms to provide objective data to the nurse regarding the quality of care provided. To improve clinical practice and motivate nurses to learn, individual self-esteem must be at a level that promotes motivation (Ward, 2003). The imperative for nurse managers is to recognize that the use of feedback in the performance appraisal process may influence an individual’s self-esteem, which may affect practice. Providing feedback is a delicate art of nursing management, which should be performed with the goal of encouraging and motivating the individual to improve his or her individual care provision.
Performance Appraisal
![]() http://evolve.elsevier.com/Huber/leadership/
http://evolve.elsevier.com/Huber/leadership/
DEFINITIONS
PERFORMANCE APPRAISAL PROCESS
ORGANIZATIONAL CULTURE AS A CATALYST TO IMPROVING PERFORMANCE
SUBCULTURES AND STAKEHOLDERS
GOALS FOR PERFORMANCE APPRAISAL
Manager’s Role
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access