19 Pediatric Trauma
Pearls
• Differences between adult and pediatric trauma care relate directly to the differences in physiology, anatomy, and mechanism of injury. The care of victims of all ages requires the same fundamental sequences of assessment and care (primary and secondary ABCDE surveys), but slight differences in their application.
• The most common serious complications of pediatric trauma are problems with airway and breathing rather than bleeding and shock, because the most serious pediatric trauma is blunt trauma involving the head.
Introduction
Trauma is the leading cause of pediatric mortality and morbidity in the United States,7 and it is a common reason for admission to a pediatric critical care unit (PCCU). Managing the child with multisystem trauma requires specific knowledge, precise management, and keen attention to detail.1,59 This chapter reviews essential aspects of nursing care of the pediatric trauma victim. Chapters 2, 3, 6, 9 and 11 contain additional helpful information.
Epidemiology and incidence of pediatric trauma
Frequency of Injuries
Although often preventable, injury continues to be the leading cause of death and disability for children older than 1 year.3,17 Nearly 3000 children 0 to 14 years old die every year as the result of injuries—more deaths than all diseases combined.45,47 Leading causes of injury death are falls, motor vehicle crashes, burn injuries, pedestrian injuries, and drowning.45,47 For additional information, see Epidemiology and Incidence of Pediatric Trauma in the Chapter 19 Supplement on the Evolve Website.
Intentional (Inflicted) Versus Unintentional Injuries
Injuries in the child can be categorized as either intentional or unintentional.19 Intentional injuries are inflicted injuries (i.e., child abuse) or injuries that result from neglect (see Intentional Injuries/Inflicted Trauma, later in the chapter). Unintentional injuries, such as many burns, drowning, and traffic-related injuries are often preventable.
Eighty to ninety percent of life-threatening pediatric trauma is blunt injury, resulting from motor vehicle-related causes and falls4,7; approximately half of motor vehicle-related injuries and fatalities are thought to be preventable with the use of age-appropriate safety restraints.27,60 Children can also sustain motor vehicle-related injuries as pedestrians or on bicycles. Although bicycle riding is a common childhood activity, it can be dangerous. The most severe head injuries are sustained when children who are not wearing bicycle helmets collide with motor vehicles.48,50,68 When a child is in a bicycle crash, a helmet will likely decrease the severity of head injuries.27
Role of Nurses and Healthcare Providers in Injury Prevention
Prevention of unintentional injuries requires an understanding of risk factors at each child’s developmental stage, and knowledge of risk-reducing actions.15,46,70 Nurses should use every “teachable moment” with families to increase parental awareness49 of the risk of unintentional injuries and to promote the use of appropriate safety equipment. A teachable moment can occur during encounters such as a well-child checkup or a parent visit to the school,20,35,60 but is probably not present when the child is in the PCCU after an injury occurred. Nurses will need to select the best opportunities and methods to teach injury prevention strategies. See the Chapter 19 Supplement on the Evolve Website, for information about injury prevention.
Physiologic differences affecting manifestation and treatment of injuries
Airway and Ventilation
Larynx and Advanced Airways
The larynx in infants and children is smaller and is more anterior and cephalad than the larynx in adults. Intubation of children is difficult and should not be attempted by inexperienced practitioners (see Chapter 9). Unless the injured child has upper airway injury, edema, or obstruction, bag-mask ventilation usually provides adequate short-term oxygenation and ventilation. However, if the duration of transport is long, continued bag-mask ventilation is suboptimal, and skilled personnel should insert an advanced airway before transport.
The laryngeal mask airway (LMA) is an acceptable advanced airway when used by experienced providers for supporting a comatose patient.16 The LMA can be inserted blindly and, when properly positioned, isolates the trachea and produces less gastric distension than bag-mask ventilation. The LMA cannot be inserted in a patient with a cough or gag reflex.
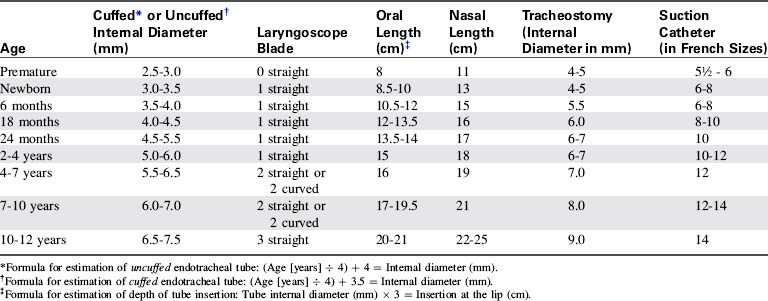
Either cuffed or uncuffed endotracheal tubes may be used in children, and cuffed tubes may be more appropriate if the child’s lung compliance is low (e.g., as following a pulmonary contusion) or if the child has high airway resistance or a large glottic air leak. If a cuffed tube is used, the cuff inflation pressure must be monitored and maintained at the pressure recommended by the manufacturer (typically less than 20-25 cm H2O).9a,38a
Providers can determine approximate airway equipment sizes (including endotracheal tubes) using a color-coded, length-based tape (e.g., a Broselow Pediatric Emergency Tape; Armstrong Medical Industries, Lincolnshire, IL).54 A table containing these approximate sizes is included on the inside back cover of this book.
Chest Wall
The chest wall of infants and children is highly compliant, so rib fractures occur in only approximately one third of children with blunt thoracic trauma.13 The child may sustain significant intrathoracic injuries, yet may not have rib fractures.3 If a rib fracture is present, it suggests that major thoracic trauma has occurred involving substantial force and energy transfer,13 and the trauma team should suspect that underlying organs including the liver, spleen, and lungs may be injured. Upper rib injuries are associated most commonly with pulmonary and major vessel injuries, whereas lower rib fractures typically are associated with liver, spleen, lung, and kidney injury.44
Cardiovascular Function and Circulating Blood Volume
Circulating Blood Volume
Tachycardia is an early sign of hemorrhage in children. Significant hemorrhage (10%-15% of circulating blood volume) will produce signs of poor systemic perfusion (e.g., mottled color, cool extremities, delayed capillary refill, thready peripheral pulses). Because the child can initially compensate for blood loss by increasing the heart rate and systemic vascular resistance, hypotension often does not develop unless the child acutely loses 20% to 25% or more of circulating blood volume.54
Neurologic Function
Spinal Cord Injury
Many children with spinal cord injury have ligamentous injury with no evidence of vertebral fracture or other radiographic abnormalities on routine (anteroposterior and lateral) spine radiographs or CT scan.42a These children have spinal cord injury without radiographic abnormality (SCIWORA), and many of these patients develop permanent neurologic injury.3,23
Nurses should carefully assess movement and sensation in all extremities on admission and at frequent intervals throughout the child’s hospitalization (see Chapter 11). The mechanism of injury should increase the index of suspicion of spinal cord injury. For example, a child wearing a lap belt without a shoulder strap who presents with abrasions or contusions on the lower abdomen may have an acute flexion injury of the lower spine (with or without a Chance fracture).
Data from the National Trauma Data Bank51 indicates that 66% of cervical spine injuries in children younger than 3 years are caused by motor vehicle crashes, and only 15% are from falls. In the National Trauma Data Bank, cervical spine injuries were present in approximately 2.3% of all children less than 3 years of age injured in motor vehicle crashes.51 However, cervical spine injuries in children younger than 3 years were still relatively uncommon.51
Fluid Administration
Vascular Access
If IV access cannot be achieved, intraosseous (IO) access is established; this route of access can be used for emergency fluid resuscitation and drug administration in patients of all ages.14 IO needles can be placed in the proximal or distal tibia or distal femur. Other placement options include the radius, ulna, pelvis, clavicle, and calcaneus. Medications and drugs can be given intraosseously until suitable venous access is achieved. Fluid may be delivered by infusion pump into an IO catheter, and bolus infusions can be provided through a syringe, an infusion pump, or a pressure bag (inflated up to 300 mm Hg). IO fluid boluses in children may be given as rapidly as 20 mL/kg over 5 min.
Initial stabilization of the pediatric trauma patient
Field Triage and Scoring
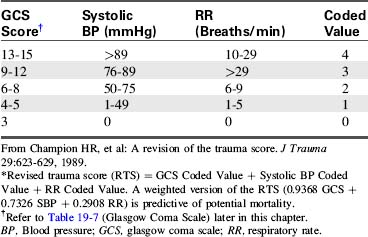
The trauma score (TS) is designed for scoring injury severity in the field; it uses the GCS score and the scoring of four additional physiologic parameters: systolic blood pressure, capillary refill, respiratory rate, and respiratory effort. Each category is scored and then totalled.10
The revised trauma score (RTS) was created to identify patients for triage to a trauma center.11 It requires evaluation of fewer physiologic parameters than the TS. To calculate the RTS, the provider assigns a coded value to the GCS score, the systolic blood pressure, and the respiratory rate and then adds these three values together (Table 19-1). A weighted version of the RTS is a predictor of mortality; an RTS of less than four is correlated with a probability of survival of less than 60%, and should prompt consideration for transfer to a trauma center.2
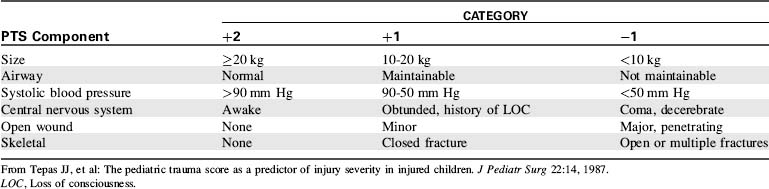
The pediatric trauma score (PTS) was developed to better identify the manifestations of injuries in children and better quantify their severity. The PTS evaluates the following six parameters: (1) patient size, (2) airway stability, (3) systolic blood pressure, (4) mental status, (5) wounds, and (6) skeletal injuries (Table 19-2).
In the PTS, large size and optimum status result in a score of 2 for each parameter; extremely small size or systemic dysfunction results in a score of −1 for each parameter. The highest possible score is a 12 and the lowest possible score is a −6.67 Children with a PTS totaling 8 or less have the highest potential for preventable mortality and morbidity, and they should be transported to a facility with the resources necessary to provide optimal pediatric care (e.g., a pediatric trauma center).67
The PTS is a conservative scoring system and will result in the triage of some children who have only moderate injuries; however, conservative triage is generally thought to be appropriate for injured children. The PTS has not been shown to be consistently superior to the RTS, so many centers continue to use the RTS for the triage of children and with good results. Because vital signs (e.g., particularly blood pressures) are often not evaluated in the field,22,38 a simple scoring system that uses fewer vital signs (e.g., the RTS) can be used more consistently than one requiring evaluation of heart rate and respiratory rate in addition to blood pressure (i.e., the PTS).
In 2006, the National College of Surgeons Committee on Trauma convened a panel of national experts on trauma field triage to develop consensus trauma triage criteria for adults and children based on physiologic criteria (GCS score, systolic blood pressure, and respiratory rate), anatomy of the injury (e.g., penetrating trauma to the head, neck, or torso; flail chest; two or more long bone fractures; amputation; pelvic fractures; open or depressed skull fractures), the mechanism of injury (e.g., falls of 10 feet [3.048 m], or a distance of more than twice or threefold the child’s height, high risk auto crashes, motor vehicle vs. pedestrian crashes, motorcycle crashes), special patient or system considerations (e.g., children should be preferentially triaged to pediatric trauma centers; patients with associated anticoagulation or bleeding disorders; the EMS provider judges transport is indicated59), and protocols.
The criteria contained in the National College of Surgeons Committee on Trauma guidelines are included in Box 19-1. A detailed explanation of these guidelines was published by the Centers for Disease Control and Prevention in 2009.56 A link to this publication is available in Triage of Injured Patients in the Chapter 19 Supplement on the Evolve Website.
Physical and Physiologic Findings
• Shock unresponsive to one bolus (defined as hypotension, with systolic BP less than 60 mm Hg in infants and less than 90 mm Hg in children) or associated with persistent prolonged capillary refill (systolic BP less than 90 mm Hg is contained in the NCS-Committee On Trauma Expert Panel Guidelines for transfer*)
• Clinical evidence of altered level of consciousness (GCS score less than 14*); coma is an absolute indication for transfer
• Respiratory rate less than 10/min or greater than 29/min*
• Any cardiac arrhythmias (including bradycardia)
• Diffuse abdominal tenderness following trauma
Types and Anatomy of Injuries
• Virtually any penetrating injury of the head, thorax, abdomen, neck or extremities proximal to the elbow and knee*
• Unstable chest wall (flail chest)*
• Two or more proximal long bone fractures*
• Crushed, degloved, or mangled extremity*
• Amputation proximal to the wrist or ankle*
• Open or depressed skull fracture*
Mechanism of Injury and Evidence of High-Energy Impact
• Fall from height greater than 10 feet (3.048 m) or a distance of twice or three-fold the child’s height*
• Intrusion into vehicle greater than 1 foot (0.3 m) into passenger space or 1.5 feet (0.46 m) on any side*
• Death in same passenger compartment*
• Vehicle telemetry data consistent with high risk of injury*
• Motor vehicle versus pedestrian or bicyclist thrown or run over or with significant (greater than 20 mph) impact*
Special Patient or System Considerations
• Anticoagulation or bleeding disorder*
• Time-sensitive extremity injury*
• End-stage renal disease requiring dialysis*
• Pregnancy greater than 20 weeks’ gestation*
BP, Blood pressure; EMS, emergency medical services; GCS, glasgow coma scale.
Modified from PCCC Transport Criteria, Harbor-UCLA Medical Center, Los Angeles, 1990; and Sasser SM, et al: Guidelines for field triage of injured patients: Recommendations of the National Expert Panel on Field Triage. Morbidity and Mortality Weekly Report 2009; 58 (RRO1):1-35.
Management of the pediatric trauma victim in the emergency department
Emergency Department Stabilization and Transfer
General indications for transfer of the critically ill child to a trauma center with a PCCU include multisystem trauma, shock requiring multiple transfusions or vasoactive drug therapy, head injury accompanied by alteration in level of consciousness, multiple long bone fractures, rib fractures in the young child, penetrating injuries, traumatic amputations, significant burns, and anticipated need for prolonged mechanical ventilation (see Box 19-1).56
Initial survey, resuscitation, and stabilization
The following information may apply to care in the ED, the acute care unit, or the PCCU. For further information regarding cardiopulmonary resuscitation in children, refer to Chapter 6.
Airway
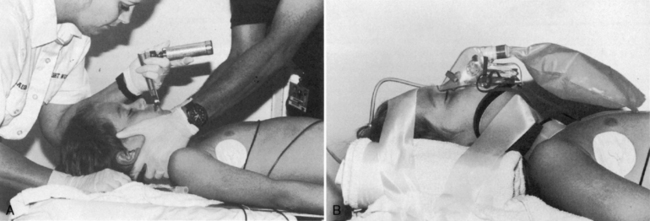
Positioning, Jaw Thrust
The first priority of stabilization and management is to establish a patent airway. The tongue of the infant and small child is large relative to the size of the oral cavity and posterior pharynx. When the patient is unconscious, the tongue can fall into the posterior pharynx, causing obstruction.54 The sniffing position (head tilt, chin lift) usually opens the airway; however, this procedure should be performed as the initial airway maneuver only if cervical spine injury has been ruled out.
If the injured child is unconscious or if the child’s mechanism of injury or presentation suggests potential cervical spine injury, the cervical spine is stabilized at the same time the airway is opened. In these children, the “jaw thrust” should be used to relieve airway obstruction; the provider holds the head and neck steady while providing gentle forward-upward pressure at the angle of the mandible to open the airway.2 For some trauma victims, such as those with isolated injury of an extremity, a cervical spine injury is unlikely and no such precautions are needed. If the airway can’t be opened with a jaw thrust, a chin lift with a slight head tilt may be needed, because an adequate airway must be established.9a,38a
Suctioning
Relatively small amounts of foreign matter in the child’s hypopharynx can obstruct the airway. As a part of initial stabilization, providers should suction the airway to eliminate obstruction such as blood, mucus, loose teeth, or vomitus. Neonates and young infants are obligate nose breathers. In these infants, gentle nasal suctioning or opening of the airway may be the only intervention required to stimulate spontaneous ventilation.2
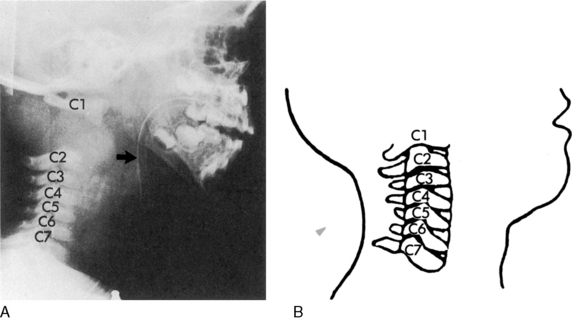
Spine Stabilization
Spinal cord injuries are less common in children than in adults. When these injuries occur in children, they are generally associated with motor vehicle-related crashes, falls, and inflicted head trauma and can result in injuries of the upper or lower cervical spine (Fig. 19-1).4
Spine stabilization and then immobilization is indicated after motor vehicle crashes, after pedestrian-related crashes, after crashes in which the child was unrestrained, for any unconscious trauma victim (because it is difficult to ascertain the extent of injury), and for any major trauma associated with head injury.2 Manual stabilization is provided initially, and then a device is used to immobilize the cervical spine during transport and initial evaluation (Fig. 19-2).
There are many acceptable methods for immobilizing the cervical spine. A semirigid collar (e.g., an extrication collar) immobilizes the cervical spine, but these collars are not recommended for use in children younger than 4 years.5 Foam collars can be applied easily and are available in small sizes, but they often provide no protection against head and neck movement. If an excessively large collar is applied, flexion of the neck may cause airway obstruction or hyperextension of the neck can result in the very movement and possible injury that the collar is designed to prevent.
Cervical spine immobilization in children requires a combination of a cervical collar (of the appropriate size) with a rigid spine board. The child’s head is supported in a neutral position on the board, using a board with head well or pads under the torso, and, foam blocks and straps. Towel rolls, and tape should be used to secure the torso and the head (see Fig. 19-2).3,25,29
If the mechanism of injury suggests thoracic spine trauma, providers should avoid any flexion or torsion of the torso. If lap belt injuries are suspected (see Secondary Survey, Abdomen), providers should prevent movement of the lumbar spine until further examination.55 The child should be log-rolled whenever turning is required until an injury to the spine is ruled out (i.e., the spine is cleared). If the child is sufficiently stable, the provider should evaluate and document movement and sensation of all extremities.
Airway Management
Oropharyngeal and nasopharyngeal airways can help to maintain a patent upper airway. Oral airways are reserved for the child with absent cough and gag reflex. Oral airways must be sized appropriately, because airways that are too small can push the tongue back into the oropharynx and those that are too long can obstruct the pharynx.54 The length of the airway should equal the distance from the mouth to the angle of the mandible. Nasal airways can be inserted in the alert child or the unresponsive child who has no facial trauma; they may facilitate suctioning.
Intubation
Intubation may be necessary to maintain a patent airway and prevent anticipated deterioration. Indications for intubation of the pediatric trauma victim (Box 19-2) include: (1) inability to ventilate the child’s lungs adequately using a bag-mask device, (2) need for prolonged airway control and prevention of aspiration, (3) severe head injury (in anticipation of a need for controlled ventilation and oxygenation), (4) flail chest, (5) severe facial burns, and (6) shock unresponsive to volume infusion.2,54
Box 19-2 Indications for Intubation in the Pediatric Trauma Victim
• Significant respiratory distress
• Hypoxemia despite oxygen therapy
• Signs of airway obstruction: stridor, increased work of breathing; suprasternal, supraclavicular retractions
• Injuries associated with potential airway obstruction (e.g., inhalation injuries, crushing facial or neck injuries)
• Head injury or signs of increased intracranial pressure
• Thoracic injury (rib fractures, pulmonary contusion, flail chest, penetrating injuries)
The nurse must be able to select intubation equipment of appropriate size. Formulas, tables, or a length-based tape that indicates the equipment sizes (i.e., the Broselow tape—see inside back cover) may be used (Table 19-3).54
In the past, only uncuffed tubes were used for children younger than 8 years, because there was concern that cuffed tubes could produce subglottic tracheal injury.2 However, for some children (e.g., those with noncompliant lungs, high airway resistance or large glottic air leak), the use of a cuffed tube may be preferable to an uncuffed tube, particularly if the child requires ventilation with high inspiratory pressure or maintenance of positive end-expiratory pressure.9a,38a Slightly different formulas are used to determine the internal diameter of a cuffed versus an uncuffed tube (see Table 19-3).
Gastric distension increases the risk of vomiting and aspiration, can stimulate a vasovagal reflex and bradycardia, compromises diaphragm movement, and can mimic or mask symptoms of abdominal injury. If gastric distension develops, providers should remove air through an orogastric tube. If the patient has craniofacial trauma with maxillofacial or basilar skull fracture, an orogastric tube is used for gastric decompression rather than a nasogastric tube. Case reports have documented intracranial migration of nasogastric tubes if they are inserted blindly.4,18
Sedation and administration of neuromuscular blockers are advisable before intubation of a conscious trauma victim, particularly if the child is struggling or has a full stomach. Rapid sequence intubation (also known as drug assisted intubation) is designed to reduce stimulation of gag reflex (and the associated risk of vomiting and aspiration) when the child has a full stomach or when the time of the last meal cannot be determined (for further information about rapid sequence intubation, see Chapter 9 and Box 9-11).
Cricothyrotomy and Tracheostomy
If positioning of the child, bag-mask ventilation, and intubation do not relieve airway obstruction and providers cannot deliver adequate ventilation, then injury to the larynx or trachea is likely to be present. Needle cricothyrotomy, although rarely necessary in the child, should be considered at this time.54 This procedure is challenging because it can be difficult to identify landmarks in the short neck of an infant or young child, and the needle is difficult to secure once it is inserted.
Ongoing Airway Assessment
If the intubated child’s condition suddenly deteriorates, the bedside nurse should provide bag-mask ventilation and quickly assess tube position and patency, and assess for complications such as a pneumothorax. The mnemonic D-O-P-E can be used to recall the causes of sudden deterioration in the child with an advanced airway: tube displacement, tube obstruction, pneumothorax, and equipment failure.9a,38a If the tube is no longer in the trachea, the nurse should remove it and provide bag-mask ventilation as needed until reintubation can be accomplished.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Be sure to check out the supplementary content available at
Be sure to check out the supplementary content available at