chapter 8
Pediatric Nursing
After studying this chapter, the student should be able to:
1 Explain the developmental changes that occur in each age group from birth through adolescence.
2 Describe two congenital defects or hereditary disorders for each major body system.
3 List three major infections (fungal or bacterial) commonly seen in children.
4 Explain three disorders specific to each age group (e.g., infancy, toddler) as presented under each major body system.
5 List three common poisonous substances accounting for deaths in young children (ages 1 to 4).
6 Identify recommended immunizations given during the first 2 years of life.
7 Differentiate between the types of traction and their uses.
8 Discuss factors that affect nursing care of the hospitalized child.
 http://evolve.elsevier.com/Mosby/comprehensivePN
http://evolve.elsevier.com/Mosby/comprehensivePN
ASSESSMENT OF CHILD AND FAMILY
A Functions and structure of family
1. The functions and structure of the family are vital to the normal growth and development of the child.
2. Three primary functions of the family
B Physical assessment of child
1. Obtaining family health history, including the child’s history and current complaints or problems, is done by the nurse, physician, or nurse practitioner.
2. Assessing of child’s physical growth and developmental level is done by the physician or nurse practitioner.
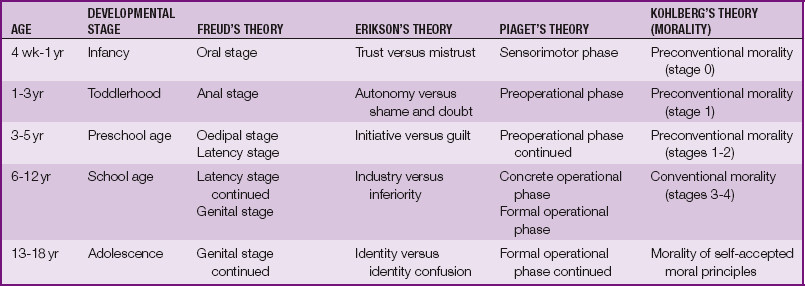
C Concepts of child development (Table 8-1)
1. Freud’s theory of development is based on the child’s psychosexual development.
2. Erikson’s theory of development is based on psychosocial development as a series of developmental tasks.
3. Piaget’s theory of development is based on intellectual (cognitive) development: how the child learns and develops his or her intelligence.
4. Kohlberg’s theory of moral development is based on the concept that the acceptance of values and rules of society shapes a child’s behavior.
CONGENITAL DEFECTS AND HEREDITARY DISORDERS
Gastrointestinal System
Cleft Lip and Palate
A Definition: abnormal openings in the lip or palate. The defects may occur unilaterally or bilaterally.
B Symptoms: A cleft lip has a notched vermilion border, which may involve the alveolar ridge and dental abnormalities. A cleft palate includes a midline or bilateral cleft with variable extension from the uvula, soft and hard palates, exposed nasal cavities, and nasal distortion.
C Diagnosis: based on observation and examination at birth; may also be diagnosed by in utero ultrasound
D Treatment and nursing interventions: based on the severity of the defect
1. Modified techniques for feeding are used to promote adequate nutrition and growth.
2. Surgery to repair the cleft lip is done as early as possible, usually at age 3 to 6 months.
3. Surgery to repair the cleft palate depends on the deformity and size of the child and is usually done by 1 year of age.
4. Recurrent otitis media is treated as needed.
5. Parent-child bonding is promoted, and emotional support is provided for parents throughout the process.
6. Other practitioners involved in the care of these children may include ear, nose, and throat specialist; speech and occupational therapists; psychologist; audiologist; orthodontic surgeon and dentist.
Gastroesophageal Reflux
A Definition: regurgitation of gastric contents into the esophagus. It can be physiological (infrequent emesis), functional (frequent emesis after meals), or pathological (failure to thrive [FTT], aspiration pneumonia, coughing, choking, dyspnea, frequent emesis).
B Symptoms: Emesis after meals, hiccups, and recurrent otitis media from secretions pooled in the nasopharynx are common to all types of gastroesophageal reflux (GER). Other manifestations include FTT, respiratory infections, weight loss, and irritability.
C Diagnosis: After other illnesses have been ruled out, GER may be confirmed by barium swallow, upper gastrointestinal (GI) study, ultrasound, or endoscopy.
D Treatment and nursing interventions: based on symptoms
1. Provide small frequent feedings of predigested infant formula (Nutramigen, Pregestimil) or hydrolyzed formula in which protein content has been broken down.
2. Position infant in prone position with head slightly elevated or in right side-lying position (these positions are considered appropriate for infants with GER).
3. For infants with pathological reflux, antacids, H2-receptor antagonists, mucosal protectants, and other medications may be used (see Chapter 3).
4. Surgery (fundoplication) to prevent future reflux may be done in up to 15% of infants with GER.
Hirschsprung Disease
A Definition: distention of a portion of the lower colon caused by a congenital lack of nerve cells in the wall of the colon just below the distended section (Figure 8-1)
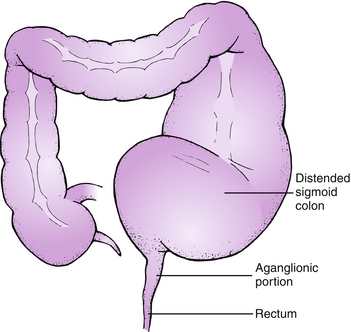
FIGURE 8-1 Hirschsprung disease. (From Hockenberry MJ, Wilson D: Wong’s nursing care of infants and children, ed 9, St Louis, 2011, Mosby.)
B Symptoms: constipation (including a lack of meconium stool in the newborn in the first 24 hours), abdominal distention, bile-stained mucus and emesis, inadequate weight gain
C Diagnosis: based on the symptoms, results of barium enema, rectal biopsy, anorectal manometry, or any combination
D Treatment and nursing interventions: based on the type of surgery (bowel resection, sometimes with temporary colostomy); surgery performed in two or three stages
a. Observation of stools: color, amount, and consistency
b. Intravenous (IV) fluids and electrolytes as ordered; if infant is malnourished, total parenteral nutrition (TPN) may be given before surgery.
a. Nasogastric (NG) tube to low-suction or gravity drainage
c. Routine colostomy care as necessary (pro re nata [p.r.n.])
d. Monitor vital signs as ordered. Axillary temperatures should be taken; avoid taking rectal temperatures.
f. Maintain nothing by mouth (NPO) status. Resume diet as ordered.
g. Record intake and output (I&O) every shift (Foley catheter may be necessary).
h. Observe stools and record amount and characteristics.
i. Observe for rectal bleeding and abdominal distention.
j. Teach parents to provide care at home (colostomy care, dressing changes, skin care).
Omphalocele
A Definition: Abdominal organs protrude through an abnormal opening in the abdominal wall and form a sac lying on the abdomen.
B Diagnosis: based on symptoms and physical examination findings
C Treatment and nursing interventions
a. Keep the omphalocele covered with sterile gauze moistened with normal saline and a plastic drape until surgery can be performed; minimize movement of the infant and the intestines.
b. Maintain sterile technique as much as possible in caring for the omphalocele.
c. Maintain proper body temperature; a warmer or an Isolette may be used.
Imperforate Anus
A Definition: Rectal pouch ends blindly at a distance above the anus. In some cases no anal opening is present. Various forms of this defect have been found.
B Symptoms: no stools in the first 24 hours after birth. Rectal thermometer cannot be inserted properly.
C Diagnosis: made by digital rectal examination, intestinal x-ray examination, and endoscopy, or antegrade endoscopic transillumination
D Treatment and nursing interventions
Esophageal Atresia, Tracheoesophageal Fistula
A Definition: Upper end of the esophagus ends in a blind pouch; lower end may also end in a blind pouch or may be connected to the trachea by fistula defect (tracheoesophageal fistula) (Figure 8-2).
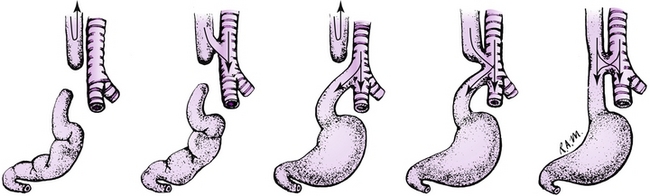
FIGURE 8-2 The five most common types of esophageal atresia and tracheoesophageal fistula. (From Hockenberry MJ, Wilson D: Wong’s nursing care of infants and children, ed 9, St Louis, 2011, Mosby.)
B Symptoms: excessive salivation and drooling, coughing and choking during feedings, regurgitation of all feedings
C Diagnosis: based on symptoms and passage of an NG tube or catheter down the esophagus to test for patency. Exact anomaly is determined by x-ray film studies.
D Treatment and nursing interventions
1. Maintenance of NPO status with administration of IV fluids as ordered
2. Suctioning of nose and mouth as needed
3. Insertion of an NG tube to drain mucus and fluid from the blind pouch
4. Antibiotic therapy as ordered (for probable aspiration pneumonia)
5. Surgical repair to correct the defects and reconnect the ends of the esophagus
6. Emotional support for the family; parent or caregiver teaching for home care
Intussusception
A Definition: telescoping of one portion of the bowel into a distal portion; ileocecal valve most common site; usually occurs between 3 and 12 months of age
B Symptoms: appear suddenly; pallor, sharp colicky pain that causes infant to draw up legs and cry out (this occurs every 5 to 10 minutes), vomiting, stools with blood and mucus (“red currant jelly” stools), signs of shock
C Diagnosis: based on symptoms; definitive diagnosis made radiographically with barium enema
D Treatment and nursing interventions: This is an emergency that requires immediate treatment. The initial treatment of choice is hydrostatic reduction by enema with water-soluble contrast or barium and air pressure; if this is not effective, surgery is necessary.
a. Careful observation and frequent recording of vital signs
b. IV fluids with electrolytes as ordered
d. NG tube to remove gastric contents
e. Emotional support for parents; explanation of all procedures; answering questions
f. Observation for passage of normal brown stool (indicates the intussusception has reduced itself); report to physician immediately.
Nervous System
Hydrocephalus
A Definition: disorder caused by an obstruction of cerebrospinal fluid (CSF) drainage or impaired absorption of CSF in the subarachnoid space; characterized by an excess of CSF within the cranial cavity, which causes an enlarged head and potential brain damage or retardation. It occurs in association with several other anomalies (developmental defects; complication of meningitis, tumor, or hemorrhage) (Figure 8-3).
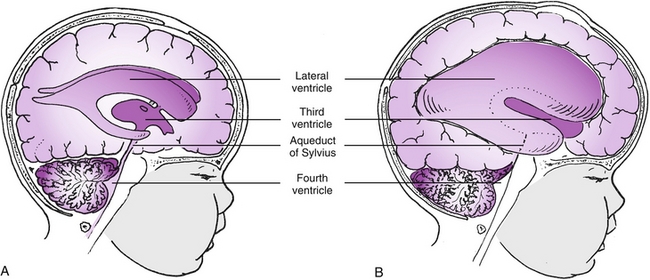
FIGURE 8-3 Hydrocephalus: a block in flow of cerebrospinal fluid. A, Patent cerebrospinal fluid circulation. B, Enlarged lateral and third ventricles caused by obstruction of circulation and stenosis of aqueduct of Sylvius. (From Hockenberry MJ, Wilson D: Wong’s nursing care of infants and children, ed 9, St Louis, 2011, Mosby.)
B Symptoms: bulging of the anterior fontanel, enlargement of the head, irritability, lethargy, setting-sun sign (sclera can be seen above the iris because of increased intracranial pressure), lower extremity spasticity, opisthotonus
C Diagnosis: based on the symptoms, frequent measurements of head circumference, computed tomography (CT), and magnetic resonance imaging (MRI)
D Treatment and nursing interventions
1. Surgical repair is necessary to relieve the obstruction or to shunt the CSF from the ventricles of the brain into the abdomen (ventriculoperitoneal shunt).
2. Postoperative care includes frequent position changes to prevent pressure on the head, care of the shunt, general postoperative care, and observation for complications (infection, shunt malfunction, return of increased intracranial pressure).
Down Syndrome
A Definition: an abnormality caused by extra chromosome 21 (trisomy 21). Children with Down syndrome (DS) are born to women of all ages. The risk is usually higher in women age 35 years and over, but some statistics indicate that more infants with DS are born to women age 35 years and under simply because that age group has more pregnancies. The incidence of DS in women age 40 years and older is approximately 1 in 100, however, one source indicated that women age 45 years have a 1 in 35 chance of having an infant with DS.
B Symptoms: hypotonia; small, low-set ears; slanted eyes; protruding tongue; small, flattened nose; short, broad neck; single transverse palmar (simian) crease; dry, cracked skin; congenital heart defects; and mental retardation
C Diagnosis: based on the physical defects. Chromosome studies are done to determine specific defects.
D Treatment and nursing interventions
1. Provide emotional support for parents; they expected a “normal” infant.
2. Assist family in preventing physical problems (respiratory, integumentary, nutrition).
3. Promote the child’s developmental progress, and help parents set realistic goals for the child.
4. Encourage activity and intellectual stimulation for the child through early intervention programs and school.
Genitourinary System
Epispadias and Hypospadias
A Definition: congenital conditions in male infants in which the urethra ends on the underside (hypospadias) or the top side (epispadias) of the penis rather than at the end
B Symptoms: obvious physical defects evident on physical examination; abnormal stream of urine
C Diagnosis: based on physical examination findings
D Treatment and nursing interventions
1. The surgery to extend the urethra to the end of the penis is usually done in several stages when the child is 6 to 18 months of age; the infant should not be circumcised because foreskin may be needed for later surgery.
2. Postoperative care includes inspection of the operative site for bleeding, catheter care, emotional support for the child and parents, and general postoperative care.
Cryptorchidism
A Definition: failure of one or both testes to descend into the scrotal sac. Sterility may result if not treated.
B Symptoms: Testes not palpable in the scrotal sac on physical examination.
C Diagnosis: based on symptoms
D Treatment and nursing interventions
1. The testes usually descend by 1 year of age (in 75% of affected infants).
2. Hormonal therapy (human chorionic gonadotropin [hCG]) may be used at an early age to promote descent of the testes into the scrotum.
3. Surgical intervention (orchiopexy), usually done at 6 to 24 months of age, is often necessary to bring the testes down the inguinal canal and into the scrotum. Postoperative care is routine.
Wilms Tumor (Nephroblastoma)
A Definition: tumor in the kidney region
B Symptoms: sometimes asymptomatic, discovered on routine examination; occasional occurrence of hematuria and elevated blood pressure; swelling or mass in the abdomen
C Diagnosis: often palpable through the abdominal wall; occurs most often in children younger than 2 years and is usually found by the caregiver before the child reaches the age of 3 years
D Treatment and nursing interventions
1. Surgery to remove the tumor is performed within 48 hours of diagnosis. Routine postoperative care is given.
2. Radiation therapy is given after surgery as ordered (for children with large tumors, metastasis, or recurrence).
3. Chemotherapy is given as ordered. The most effective agents are actinomycin D and vincristine.
4. Emotional support and education for parents are provided.
E Prognosis is good with early diagnosis and treatment for children under 2 years of age.
F Alert: Do not palpate abdomen preoperatively as this may cause trauma to the mass and release cancer cells into the patient’s system.
Musculoskeletal System
Congenital Clubfoot (Talipes Equinovarus)
A Definition: defect in which the entire foot is inverted, heel is drawn up, and front of foot is adducted; can affect one or both feet (Figure 8-4)
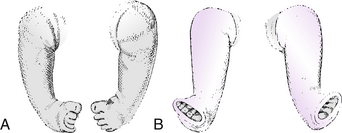
FIGURE 8-4 Feet in casts for correction of bilateral congenital talipes equinovarus. A, Before correction. B, Undergoing correction in plaster casts. (From Brashear HR, Raney RB: Handbook of orthopaedic surgery, ed 10, St Louis, 1986, Mosby.)
B Symptoms: obvious physical defect evident on physical examination
C Diagnosis: based on the presence of the physical defect on examination
D Treatment and nursing interventions
Developmental Dysplasia of the Hip
A Definition: group of disorders related to abnormal development of the hip in which a shallow acetabulum, subluxation, or dislocation is present; may result from laxity of the supporting capsule or an abnormality of the acetabulum
B Symptoms: limited hip abduction, apparent shortening of femur, asymmetry of gluteal and thigh folds (Figure 8-5)
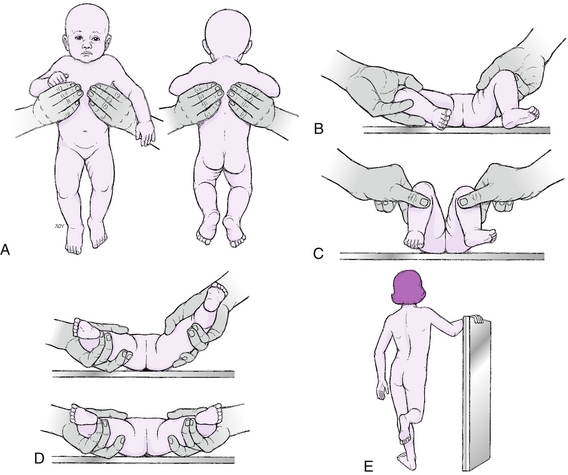
FIGURE 8-5 Signs of developmental dysplasia of the hip. A, Asymmetry of gluteal and thigh folds. B, Limited hip abduction, as seen in flexion. C, Apparent shortening of the femur, as indicated by the level of the knees in flexion. D, Ortolani click (if infant is younger than 4 weeks). E, Positive Trendelenburg sign or gait (if child is weight bearing). (From Hockenberry MJ, Wilson D: Wong’s nursing care of infants and children, ed 9, St Louis, 2011, Mosby.)
C Diagnosis: symptoms found on physical examination by the physician or nurse practitioner
D Treatment and nursing interventions
1. Treatment is started as soon as the defect is diagnosed. The hip is manipulated into proper position, and an abduction device (Pavlik harness, Figure 8-6) or hip spica cast is applied. Modified Bryant traction or modified Buck extension may also be used.
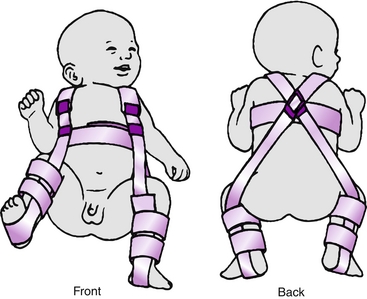
FIGURE 8-6 Child in Pavlik harness. (From Ball JW: Mosby’s pediatric patient teaching guides, St Louis, 1998, Mosby.)
2. Nursing care includes parent teaching regarding application of the harness and cast care.
Cardiovascular System
Congenital Heart Defects (Cyanotic and Acyanotic)
A Atrial septal defect (ASD): abnormal opening in the septum between the two atria, or a patent foramen ovale, that causes left-to-right shunting of the blood (acyanotic)
B Ventricular septal defect (VSD): abnormal opening in the septum between the two ventricles that causes left-to-right shunting of the blood (acyanotic)
C Patent ductus arteriosus (PDA): condition in which ductus arteriosus remains open after birth instead of closing off as normal, causing an overload of the left heart and a slight murmur (acyanotic)
D Coarctation of the aorta: constriction of the aortic arch, causing hypertension in the upper body and hypotension in the lower body (acyanotic)
E Tetralogy of Fallot: consists of four congenital defects—pulmonary stenosis, VSD, overriding of the aorta, and right ventricular hypertrophy (cyanotic)
F Classic symptoms of congenital heart defects: dyspnea, difficulty with feeding, clubbing of fingers, cyanosis (in certain defects), heart murmurs, rapid pulse, recurrent respiratory infections, edema
G Diagnosis: based on symptoms, electrocardiograms, echocardiograms, cardiac catheterizations, and chest x-ray examinations
H Treatment and nursing interventions
1. Most defects must be corrected by surgical intervention, often in stages. Some symptoms can be treated with medications as ordered.
2. Nursing care measures depend on the type of treatment or surgery. Most often, immediate postoperative care is given in intensive care units.
3. Patient and parent teaching should include instructing parents to help the child conserve energy without being overprotective.
Sickle Cell Anemia
A Definition: autosomal disease occurring mainly in African Americans and occasionally in Caucasians of Mediterranean descent; causes breakdown of red blood cells (RBCs) carrying an abnormal hemoglobin S, which leads to a severe hemolytic anemia. The disease may not be recognized until the toddler or preschool period.
B Symptoms: appear only in children who inherit the trait from both parents; fatigue, anorexia, decreased hemoglobin. Sickle cell crisis may occur, causing severe joint pain, abdominal pain, fever, and firm, distended abdomen (Figure 8-7). Because children with sickle cell disease do not have a properly functioning spleen, they are more susceptible to infection and sepsis.
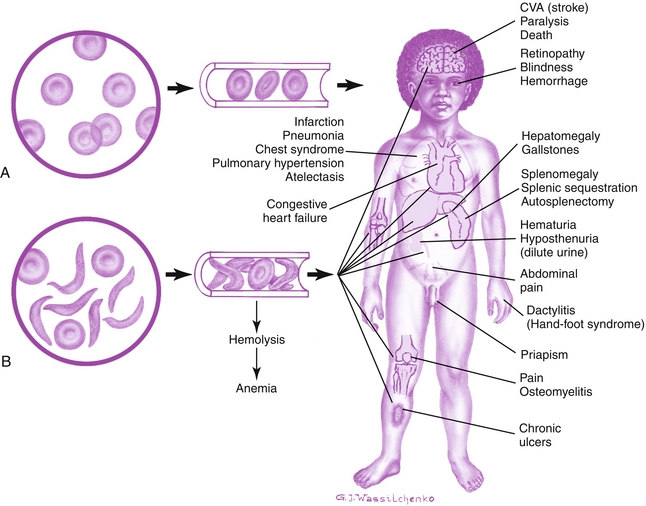
FIGURE 8-7 Differences between effects of normal (A) and sickled red blood cells (B) on circulation with selected consequences in a child. CVA, Cerebrovascular accident. (Modified from Hockenberry MJ, Wilson D: Wong’s nursing care of infants and children, ed 9, St Louis, 2011, Mosby.)
C Diagnosis: based on the symptoms; family history of the disease; and results of specific blood tests, including the sickle cell slide preparation, sickle turbidity test (Sickledex), and hemoglobin electrophoresis (fingerprinting)
D Treatment and nursing interventions
1. IV fluids and fluids by mouth (PO) as ordered
2. Oxygen therapy, especially during sickle cell crisis
5. Analgesics for pain as ordered
6. Blood transfusions as ordered (packed RBCs)
7. Prophylactic antibiotic therapy as needed
8. Education and genetic counseling for parents
9. Proper nutrition as tolerated, including folic acid
10. Avoidance of exposure to people with colds and infections
11. Avoidance of exercise at high altitudes because oxygen concentration in the blood is already severely reduced
Endocrine System
Hypopituitarism (Dwarfism)
A Definition; growth retardation resulting from deficiency of the growth hormone (GH)
B Symptoms: short stature, well-nourished appearance, delayed physical development
C Diagnosis: based on family history, child’s growth patterns, physical examination findings, x-ray film studies, and endocrine studies
D Treatment and nursing interventions
1. Replacement of the GH by subcutaneous injections
2. Early diagnosis and treatment to help prevent many physical and emotional problems that occur later in childhood
3. Provision of emotional support for the child and parents during diagnostic procedures and early stages of treatment (even after GH therapy is started, growth will be slower than normal)
Congenital Hypothyroidism (Cretinism)
A Definition: lack of thyroid function resulting from failure of the embryonic development of the thyroid gland
B Symptoms: usually do not appear until 6 to 12 weeks of age in bottle-fed infants and after weaning in breast-fed infants and include feeding problems; inactivity; anemia; thick, dry, mottled skin; bradycardia; relaxation of the abdominal muscles; and delayed development of the nervous system, which leads to mental retardation
C Diagnosis: based on the symptoms and results of tests of thyroid function, such as initial measurement of the newborn’s thyroxine (T4) and thyroid-stimulating hormone (TSH) levels
D Treatment and nursing interventions
Respiratory System
Cystic Fibrosis
A Definition: an autosomal-recessive hereditary disease of the exocrine glands causing those glands to produce abnormally thick secretions of mucus, increased sweat electrolytes, and increased activity of the autonomic nervous system causing obstruction. The glands most often involved are those in the lungs and pancreas and the sweat glands. The disorder is diagnosed in infancy or early childhood.
1. In newborns: meconium ileus, bile-stained emesis, distended abdomen, no stools, salty “taste” to the skin resulting from increased sodium in the perspiration
2. In infants and children: harsh, dry cough; frequent bronchial infections; malnutrition; distended abdomen; barrel chest; clubbed fingers; bulky, greasy, foul-smelling stools (steatorrhea)
C Diagnosis: based on family history, a history of FTT, the symptoms, lung changes revealed on chest x-ray films, an elevated sweat chloride level (increased sodium in the perspiration), and stool analysis for fat and enzymes
D Treatment and nursing interventions
1. Pancreatic enzymes given as ordered with food to improve digestion of fats and proteins
2. High-carbohydrate, high-protein, low-fat diet
3. Increased amounts of salt and water-soluble vitamins
4. Inhalation therapy: nebulizer treatments of bronchodilators (see Chapter 3) and recombinant human deoxyribonuclease (DNase) to decrease the viscosity of the mucus
5. Daily routine of chest physiotherapy and postural drainage to help in expectoration of mucus
6. Physical exercise to stimulate mucus secretion; avoid use of cough suppressants
7. Antibiotics for all pulmonary infections
8. Parent teaching regarding diet, medications, and inhalation therapy for proper home care after discharge
9. Referral to the Cystic Fibrosis Foundation for education and financial or emotional support
INFANCY (AGES 4 WEEKS TO 1 YEAR)
NORMAL GROWTH AND DEVELOPMENT
Physical Development
a. Weight: gains approximately 5 to 7 ounces (150 to 210 g) weekly during first 6 months of life
b. Height: gains approximately 1 inch (2.5 cm) per month for first 6 months of life
a. May lift head temporarily but generally needs support
b. Holds head parallel with body when placed prone
c. Can turn head from side to side when prone or supine
d. Domination of asymmetrical posture such as tonic neck reflex
e. Primitive reflexes still present and strong (grasp, Moro, tonic neck).
4. Socialization and vocalization
1. Physical: posterior fontanel closed
a. Holds head erect for a short time and can raise chest supported on forearms
b. Can carry hand or an object to the mouth at will
c. Reaches for attractive objects but misjudges distances
d. Grasp, tonic neck, and Moro reflexes fading
e. Can sit when the back is supported; knees flexed and back rounded
f. Disappearance of step or dance reflex
4. Socialization and vocalization
1. Physical: Drooling begins because salivary glands are functioning, but the child does not have sufficient coordination to swallow saliva.
a. Balances head well in a sitting position
b. Sits with little support; holds back straight when pulled to a sitting position
c. Predomination of symmetrical body position
d. Can sustain a portion of own weight when held in a standing position
e. Reaches for and grasps an object with the whole hand
f. Can roll over from back to side
g. Lifts head and shoulders at 90-degree angle when prone
h. Disappearance of primitive reflexes (e.g., grasp, tonic neck, Moro)
4. Socialization and vocalization
a. Weight: gains approximately 3 to 5 ounces (90 to 150 g) weekly during second 6 months of life; weight doubles by 6 months
b. Height: gains approximately 1⁄2 inch (1.25 cm) per month
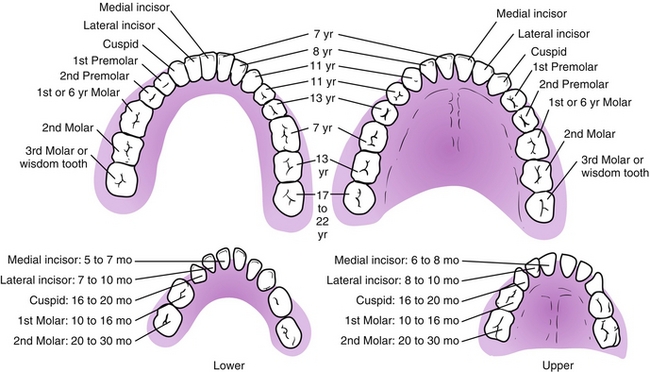
c. Teething may begin with eruption of two lower central incisors, followed by upper incisors (Figure 8-8).
a. Can turn over equally well from stomach or back
b. Sits fairly well unsupported, especially if placed in a forward-leaning position
c. Hitches or moves backward when in a sitting position
d. Can transfer a toy from one hand to the other
e. Can approach toy and grasp it with one hand
f. Plays with feet and puts them in mouth
g. When lying down, lifts head as if trying to sit up
4. Socialization and vocalization
b. Has good hand-to-mouth coordination
c. Develops pincer grasp, with preference for use of one hand over the other
d. Crawls and then creeps (creeping is more advanced because the abdomen is supported off the floor)
e. Can raise self to a sitting position but may require help to pull self to feet
3. Socialization and vocalization
a. Shows anxiety with strangers by turning or pushing away and crying
b. Definite social attachment is evident: stretches out arms to loved ones
c. Is voluntarily separating self from mother by desire to act on own
d. Reacts to adult anger: cries when scolded
e. Dislikes dressing, diaper change
f. No true words as yet but comprehends words such as “bye-bye, no-no”
a. Has tripled birth weight by 1 year
b. Eruption of upper and lower lateral incisors for total of six to eight teeth
c. Head and chest circumferences equal
d. Development of lumbar curve; lordosis evident when walking
a. Stands alone for short times
b. Walks with help; moves around by holding onto furniture
c. Can sit down from a standing position without help
d. Can eat from a spoon and drink from a cup but needs help; prefers using fingers
f. Can hold a crayon to make a mark on paper
4. Socialization and vocalization
a. Shows emotions such as jealousy, affection, anger
b. Enjoys familiar surroundings and will explore away from mother
c. Fearful in strange situation or with strangers; clings to mother
d. May develop habit of “security” blanket
e. Can say three to five words besides “dada” or “mama”
f. Understands simple verbal requests such as “Give it to me”
Psychosocial Development
A Infants are in Erikson’s stage of “trust versus mistrust”; infants develop a sense of trust or mistrust, depending on how their needs are met by their parents (or other caregivers).
B As infants grow, they slowly realize that they are separate from their environment and that they influence their environment with their actions.
C Infants’ early activities are mostly reflexes (e.g., crying, sucking, kicking). As the months progress, they learn to move in certain ways, follow with their eyes, and smile in response to a smile and soft words.
HEALTH PROMOTION
A Immunizations should be given on schedule (Figure 8-9).
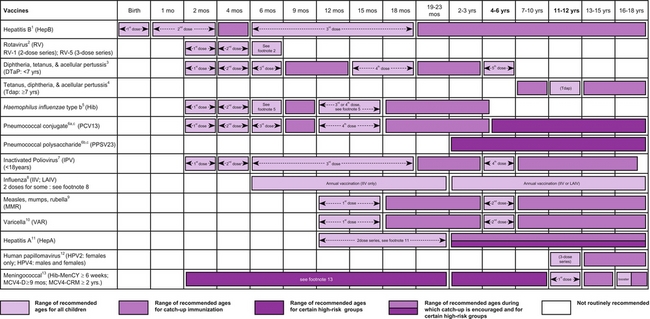
FIGURE 8-9 Recommended immunization schedule for persons aged 0 through 18 years—2013. See http://www.cdc.gov/vaccines/schedules for footnotes that accompany this schedule and for any updates to the schedule. (From Centers for Disease Control and Prevention: Recommended immunization schedules for persons aged 0 through 18 years, United States, 2013.)
B Nutrition appropriate to the age and needs of the infant should be provided.
1. Human milk is the most desirable complete diet for the first 6 months of life.
2. Introduction of strained foods may begin at 6 months of age, starting with strained fruits.
3. Solid foods should be introduced slowly, in small amounts and one at a time, to determine the infant’s likes and dislikes. This also helps detect possible allergies to certain foods. Allow 4 to 7 days between the introduction of each new food. Honey should be avoided during the first 12 months because of the risk of botulism.
4. Weaning from breast or bottle to a cup can begin at 5 to 6 months of age, although the infant cannot be weaned completely until 12 to 24 months of age.
C Safety and accident prevention includes a safe home environment, safe toys, use of car seats, and close attention to the infant who is crawling or walking.
HEALTH PROBLEMS
Nutritional Disorders
Failure to Thrive
A Definition: state of inadequate growth resulting from inability to obtain or use calories; leads to malnutrition
B Symptoms: below normal weight and height (below fifth percentile for age), listlessness, poor feeding habits, unresponsive to holding and attention, voluntary regurgitation, prolonged periods of sleep
1. Based on symptoms and a continued deviation from an established growth curve
2. Three general categories of FTT
D Treatment and nursing interventions (directed at correcting the malnutrition)
1. Correction of organic causes if possible
2. Development of a structured routine
4. Adequate food for weight gain; may include NG feedings and bottle feedings during early treatment
5. “Tender loving care” (TLC): holding and cuddling, talking to the infant
6. Teaching and encouraging the mother and father regarding feeding, infant care, and parenting skills
Colic
A Definition: paroxysmal abdominal pain or cramping that is exhibited by crying and drawing the legs up to the abdomen. Colic is most commonly seen in infants under the age of 3 months.
B Symptoms: episodes of loud crying accompanied by abdominal cramping. Despite obvious indications of pain, the infant usually tolerates feedings well and gains weight.
C Diagnosis: based on symptoms reported by parents or caregivers
D Treatment and nursing interventions
1. Take a thorough history of the infant’s daily activities, including the infant’s and breast-feeding mother’s diets; time of day when colic occurs; characteristics of crying; and activity before, during, and after crying.
2. If child is bottle-fed, investigate possibility of cow’s milk allergy; substitution of another formula (e.g., casein hydrosylate [Nutramigen]) may be tried.
3. Comfort measures that can be used by the parents and caregivers
a. Place infant prone over a covered hot-water bottle or covered heating pad (ensure that hot water bottle is warm, not hot).
c. Change infant’s position frequently.
d. Provide smaller, frequent feedings; burp infant during and after feedings, and place infant in an upright seat after feeding.
4. Pharmacological agents such as sedatives, antispasmodics, antihistamines, and antiflatulents are sometimes recommended.
Respiratory Disorders
Upper Respiratory Infection
A Definition: viral or bacterial infection affecting the upper respiratory tract. Nasopharyngitis or the “common cold” is particularly common in children of all ages.
B Symptoms: fever, sore throat, sneezing, nasal congestion, occasional cough, irritability, anorexia
C Diagnosis: based on symptoms
D Treatment and nursing interventions
1. Bed rest until free of fever
3. Antipyretics for fever (acetaminophen, ibuprofen; not aspirin)
4. Nose drops to relieve nasal congestion
5. Oral decongestants as ordered
6. Adequate nutrition for age. Infants and young children can better tolerate high-calorie fluids and soft foods.
7. Cool-air humidifier for moistened air (to assist in decreasing congestion)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree