chapter 7
Maternity Nursing
After studying this chapter, the student should be able to:
1 Correctly use terminology appropriate in maternal child nursing.
2 Identify the signs and symptoms of labor in all three stages.
3 Using the nursing process, describe the care required for a “pregnant family” in all four trimesters of pregnancy.
4 Develop a nursing care plan for both the normal postpartum family and families experiencing complications of pregnancy.
5 Describe causes of high-risk pregnancy and the nursing interventions involved.
6 Explain the nursing care involved in the entire process of labor.
 http://evolve.elsevier.com/Mosby/comprehensivePN
http://evolve.elsevier.com/Mosby/comprehensivePN
EVOLUTION OF MODERN OBSTETRICS
A Contributors in the United States:
1. Anne Hutchinson (1634): midwife who delivered many babies of early settlers
2. William Shippen: established first lying-in hospital and midwifery school in the United States in 1762
3. Oliver Wendell Holmes (1809-1894): stressed cleanliness and handwashing before caring for new mothers
4. Margaret Sanger Research Bureau (1923): first organization to address question of contraception and planned parenthood
B U.S. legislation affecting mothers and children
1. 1921: Sheppard Towner Act: promoted health and welfare for mothers and children
2. 1936: First Social Security benefits; later to include entitlement benefits for mothers and their dependent children
3. 1943: Emergency Maternal and Infant Care Act to assist families of soldiers during World War II
4. 1973: Supreme Court legalized abortion.
5. 1974: Women, Infants, and Children (WIC) Program: federally funded nutritional program providing supplementary food to eligible pregnant, lactating, or postpartum women; their infants; and children under 5 years of age
6. 1995-1996: Several states enacted legislation to lengthen a postpartum stay to 48 hours for a vaginal delivery and 96 hours for a caesarean birth; early discharge would be voluntary.
DEFINITIONS COMMONLY USED IN OBSTETRICS
STATISTICS
Birth rates: number of live births per 1000 population
Fetal death (stillborn): fetus of 20 weeks or more gestational age who dies in utero before birth
Infant mortality rate: number of deaths before the first birthday per 1000 live births
Maternal mortality rate: number of mothers dying in or because of childbirth per 100,000 live births
Neonatal death: death within first 4 weeks of life
Neonatal death rate: number of deaths within the first 4 weeks of life per 1000 live births
Note: Statistics are important to identify problem areas and trends in the health care setting.
ABBREVIATIONS (LIMITED LISTING)
ABC: alternative birthing center
AIDS: acquired immunodeficiency syndrome
ARM, AROM: artificial rupture of membranes
CPD: cephalopelvic disproportion
DIC: disseminated intravascular coagulation
EDC: estimated date of confinement; due date for birth
EDD: estimated date of delivery
G: gravida; number of pregnancies
GH: gestational hypertension (formerly known as pregnancy-induced hypertension [PIH])
GTPAL: gravida, term, premature, abortions, living children; identification of pregnancy status
hCG: human chorionic gonadotropin
HELLP: hemolysis, elevated liver enzymes, low platelet count; extension of pathological factors related to severe preeclampsia
HIV: human immunodeficiency virus
LDRP: labor, delivery, recovery, postpartum: All phases of maternal and child care occur in the same room with the same staff member.
LGA: large for gestational age
P: para; number of viable births
PROM: premature rupture of membranes
Q: quadrant; one of four equal parts into which abdomen is divided to designate position of fetus in uterus
RhoGAM: antibody against Rh factor given early prenatally or within 72 hours postpartum to mother
SGA: small for gestational age
TORCHES: a group of intrauterine infections, including toxoplasmosis, rubella, cytomegalovirus, herpes, and syphilis; commonly associated with high infant mortality
COMMON OBSTETRICAL TERMINOLOGY
Advanced maternal age: age older than 35 years of age for a woman giving birth to her first child
Ante: prefix meaning before, e.g., antepartum: time before delivery
Apgar score: method of evaluating infant immediately after delivery; usually determined at 1 minute and 5 minutes
Braxton-Hicks contractions: painless uterine contractions felt throughout pregnancy, becoming stronger and more noticeable during second and third trimesters
Caput: head; cephalic portion of infant
Dystocia: long, painful labor and delivery
Gestation: developmental time of embryo, fetus in utero
Grand multipara: having had more than five children
Gravida: any pregnancy, regardless of duration, including the present one
High risk: describes a pregnant woman with preexisting problems that can jeopardize the pregnancy, the fetus, or herself; younger than 18 years of age or older than 35 years of age with no prenatal care (any one or more of these conditions)
Lightening: moving of the fetus and uterus downward into the pelvic cavity during the last 2 weeks before EDC (usually just before labor in multiparas)
Low birth weight: weight less than 5½ pounds (2500 g) because the baby is preterm (premature) or because of intrauterine growth retardation
Low risk: describes a pregnant woman with normal history between ages 18 and 34 years with no medical, psychological, or other preexisting problems and under good prenatal care
Meconium: first bowel movement of the newborn—thick, tarlike, greenish-black substance
Multigravida: a woman who has been pregnant more than one time
Multipara: a woman who has given birth to more than one child
Para: number of births after 20 weeks’ gestation, whether infants were born alive or dead
Postmature infant: an infant born after 42 weeks’ gestation
Premature infant: an infant born any time before 37 weeks’ gestation
Primigravida: a woman who is pregnant for the first time
Primipara: a woman who is giving birth to her first child
Quickening: first movements of the fetus felt by the mother (16 to 18 weeks’ gestation)
Secundines: afterbirth of placenta and membranes
Term infant: an infant born between 38 and 42 weeks’ gestation
Vernix caseosa: cheesy material covering the fetus and newborn that acts as a protection to the skin
Viable: capable of developing, growing, and sustaining life, such as a normal human fetus at 24 weeks’ gestation. The current legal age of viability is 24 weeks.
Vis a tergo: external pressure on the fundus to assist in the delivery of the infant
TRENDS
A Cost containment: Rising health care costs are a national concern. Increased home care, shortened stays, and increased emphasis on prenatal care are interventions to help control cost and maintain quality. Regionalization of services for high-risk childbearing families and managed care are newer methods to attempt to control costs.
B Prenatal care: Emphasis must be placed on improving access to prenatal care, particularly for low-income women. Prenatal care can avoid many conditions (complications) that can be prevented with adequate monitoring during pregnancy.
C Legislation has been passed at a federal level that guarantees women who give birth vaginally a minimum stay of 48 hours. Women who have a caesarean birth are guaranteed 72 hours.
D High-technology care: Technological developments, including fetal surgery, ultrasonography, and genetic testing, have often outpaced society’s ability to determine ethical implications of their use. Advancements in technology have enabled many infants to survive today who would not have done so in the past.
E Changing demographics: Women are waiting longer in life to have their first babies; nurses need to be familiar with effects of pregnancy on older women.
F Teen pregnancy: Nurses need to identify and implement strategies to decrease incidence of adolescent pregnancy.
G Changing cultures: Nurses need to be sensitive to ideas and health practices of different cultures. Examples in which culture plays an important part include pain expression, choice of support person, and preference for a female health care provider. Many cultures view childbirth as a natural experience; therefore it does not require any special care. Specific cultural and genetic groups are associated with different genetic conditions. An example of this would be sickle cell anemia, which is common in African Americans.
H Prepared childbirth experience: Mother and father (or alternate) jointly attend childbirth education classes to prepare for the child and for the childbearing and childbirth experience.
I Alternative birth centers (ABCs)
Birthing centers outside of hospital:
Individual’s home: The number of home births has remained small in the United States.
Use of the birthing chair instead of traditional table
Birthing room: Labor, delivery, and postpartum hospital stay are incorporated into one cheerful, homelike room set up with necessary labor and delivery equipment.
J Variety of positions used to assist labor and delivery (e.g., squat, side position)
K Showering during first or second stage of labor; some hospitals have whirlpool for early labor.
L Inclusion of father or alternate: Support person stays in labor and delivery area for both vaginal and caesarean deliveries.
M Rooming-in: allows newborn in room with mother for the day; fathers allowed unlimited visiting time
N Sibling visits: designated hours that children may visit and see baby
O Use of midwives: Many hospitals and birthing centers throughout the United States now have nurse-midwives as the primary care person conducting prenatal, labor, delivery, and follow-up care.
P Caesarean deliveries: more frequent now because of sophisticated fetal monitoring. The practice is controversial because the number has been increasing in recent years.
Q Breast-feeding: accepted and encouraged. Societies such as La Leche League and the popularity of natural foods encourage breast-feeding. Lactation practitioners are available in many facilities to assist women with nursing.
R Genetic counseling: Increasingly accurate, safe amniocentesis and advances in genetics encourage counselors to advise couples with genetic concerns. The human genome project is an effort to identify the genes that can cause genetic disorders. Identification and replacement of genes are still not routine.
S In vitro method of fertilization to assist pregnancy and fetal development: usually chosen by couples with fertility problems after exploring various methods, including fertility drugs and other insemination practices. Newborn screening is standard in many countries.
T Sex selection: available before conception by separating sperm. Many ethical concerns surround this practice.
U Students are advised to review U.S. Department of Health and Human Services: Healthy People 2020: National Health Promotion and Disease Prevention Objectives, http://www.healthypeople.gov/2020/default.aspx.
PROCEDURES TO DIAGNOSE MATERNAL AND FETAL PROBLEMS
A Alpha-fetoprotein (AFP) test
1. Screening procedure, not diagnostic
2. Serum from maternal blood sample tested; best results if sample is taken at 16 to 18 weeks’ gestation; identifies unrecognized high-risk pregnancies
3. Elevated levels in maternal serum: indicate 5% to 10% of open neural tube defects (spina bifida) in developing fetus
4. Recommend two samples be tested, followed by ultrasound and amniocentesis to confirm findings; genetic counseling availability if confirmed
5. Other causes of elevated AFP levels: multiple gestation, missed abortions, other abnormalities (elevated levels may indicate Down syndrome)
B Hemoglobin electrophoresis identifies presence of sickle cell trait in women of African or Mediterranean descent.
C Ultrasound: can be performed endovaginally or abdominally
1. Performed when high risk of fetal loss is suspected
2. Used to evaluate pregnancy and determine the age of the fetus
D Amniocentesis: invasive procedure during which a needle is inserted through abdomen and uterus to withdraw amniotic fluid; usually done after fourteenth week
1. Used for determining gender, defects in fetus (e.g., Down syndrome, Tay-Sachs disease), and fetal status (Rh isoimmune problem, fetal maturity, other tests as listed in this section)
2. Lecithin/sphingomyelin ratio (L/S ratio): used to determine fetal lung maturity by testing surfactant by thirty-fifth week of pregnancy; lecithin level two times greater than sphingomyelin level indicates that lungs are mature.
3. Creatinine level: used to test fetal muscle mass and renal function; 0.2 mg/100 mL amniotic fluid at 36 weeks is normal level; large amount may also indicate a large fetus such as the fetus of the mother with diabetes.
4. Bilirubin level: used for determination of fetal liver maturity; should decrease as term progresses.
5. Cytological testing: determines percentage of lipid globules present in amniotic fluid; indicates fetal age
1. Permits first-trimester testing for biochemical and chromosomal defects; invasive and high-risk procedure during which a plastic catheter is inserted vaginally into the uterus; ultrasound guides catheter to chorionic frondosum.
2. Can be done 9 to 11 weeks after LMP
3. Done earlier than amniocentesis. Recent evidence shows that test may increase risk of babies born with missing toes and fingers or shortened digits.
F Fetoscopy: invasive procedure involving transabdominal insertion of metal cannula into abdomen; visualization of fetus and placenta for developing abnormalities and to obtain fetal skin or blood samples
1. High-risk procedure; complications include spontaneous abortion and premature labor.
2. Limited usage, only if defect cannot be detected otherwise
G Umbilical cord technique: evaluates condition of fetus
1. Superior technique because fetal blood can be analyzed as early as eighteenth week of gestation
2. Can evaluate blood count, liver function, blood gases, acid-base status
3. Invasive procedure; limited use because of risk of injury to fetus
H Estriol level study: 24-hour urinalysis of urine from mother; determines estriol level to ascertain fetal well-being and placental functioning
1. Performed at third trimester (32 weeks)
2. Level of 12 mg of estriol in 24 hours is good; below 12 mg indicates that infant is in jeopardy (related to decreased placental functioning).
3. Decreasing estriol levels can be used in combination with other diagnostic tests to indicate a compromised placenta or fetus.
I Heterozygote testing (mother’s blood): done to detect clinically normal carriers of mutant genes
1. Tay-Sachs disease: common fatal genetic disease affecting children of Ashkenazi Jews (Eastern Europe)
2. Sickle cell anemia: common disorder among black Americans of African descent; 1 in 10 African Americans is a carrier.
3. Cooley anemia (β-thalassemia): genetic disorder frequent among Mediterranean ethnic groups: Italians, Sicilians, Greeks, Turks, Middle Eastern Arabs, Asian Indians, Pakistanis
J Contraction stress test (CST): late-trimester test to measure placental insufficiency and fetal reaction to uterine contractions (potential fetal compromise)
1. Usually done after EDC has passed
2. Invasive procedure during which intravenous (IV) oxytocin is administered; baseline recorded on monitor; takes 20 to 60 minutes
3. Breast stimulation techniques done in some health care settings in place of oxytocin infusion during a CST
4. Results: Late decelerations during contraction for at least three contractions indicate a positive test result. No decelerations during three successive contractions within 10 minutes indicate a negative test result. Occasionally inconsistent decelerations indicate suspicious conditions.
K Nonstress test (NST): assesses and evaluates FHT response to uterine movement or increased fetal activity
L Ultrasound procedure: use of high-frequency sound waves to determine fetal size, estimate amniotic fluid volume, detect neural tube defects, assess for limb abnormalities, evaluate fetal presentation, and diagnose breech presentation
1. Usually a second-trimester procedure
2. Procedure is noninvasive and relatively comfortable.
3. Acoustic sound waves can be used to help stimulate an inactive fetus during an NST.
M Biophysical profile: Using ultrasound and an NST, this profile evaluates five fetal variables—breathing movements, body movements, muscular tone, qualitative amniotic fluid volume, FHR.
N Doppler flow studies: use of ultrasound techniques to evaluate blood flow studies in deep-lying vessels. These are particularly useful in managing high-risk pregnancies.
O Fetal movement: noninvasive method of determining fetal well-being. Patterns that deviate from normal pattern may be an indication for further studies.
ANATOMY AND PHYSIOLOGY OF REPRODUCTION
OBSTETRICAL PELVIS
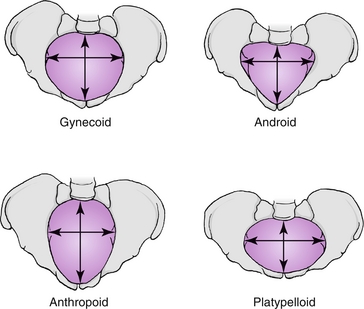
FIGURE 7-1 Female pelvis: pure types. (From Leifer G: Maternity nursing: an introductory text, ed 11, St Louis, 2012, Mosby.)
1. Gynecoid: “true” female pelvis—considered the ideal pelvis for a vaginal birth
2. Anthropoid: narrow from side to side
3. Android: male pelvis (not adequate for vaginal delivery)
4. Platypelloid: flat pelvis that is narrow from front to back (not adequate for vaginal delivery)
1. Ilium: flat or lateral, flaring part of pelvis or hip. Iliac crest is top part of ileum.
2. Ischium: inferior dorsal or lower part of hip bone. The ischial spines, sharp projections of the ischium, are important in obstetrics because they are landmarks to measure progress of presenting part of fetus.
3. Sacrum: triangular bone between the two hip bones; flat part of the lower back (spine)
4. Coccyx: two to five rudimentary vertebrae that are fused and attached to lower part of sacrum (tailbone)
FERTILIZATION AND IMPLANTATION
1. Fertilization: occurs when the sperm and ovum join, usually at the distal third of the fallopian tube within 12 to 48 hours after intercourse
2. Zygote: product of the union of a sperm and ovum
3. Implantation: occurs when zygote burrows into the endometrium of the uterus, approximately 7 days after fertilization
1. Mitosis: rapid cell division
2. Blastoderm: first division of the zygote
3. Morula: ball-like structure of the blastoderm; sometimes referred to as mulberry-like
4. Blastocyst: The ball-like structure (morula) becomes the blastocyst as it enters the uterus.
5. Trophoblast: As blastocyst implants in the uterus, the wall becomes the trophoblast.
6. Chorionic villi: Trophoblasts develop villi that become fetal portion of the placenta.
7. Decidua: Endometrium undergoes a change when pregnancy occurs.
8. Decidua vera: portion of the decidua that becomes the lining of the uterus, except for around implantation site
9. Decidua basalis: where implantation occurs and chorionic villi become frondosum, or the beginning of the placental formation
10. Decidua capsularis: covers blastocyst and fuses to form fetal membranes
11. Amnion: inner membrane, which comes from the zygote and blends with the cord
12. Chorion: outer membrane, which comes from the zygote and blends with the fetal portion of the placenta
DEVELOPMENT OF HUMAN ORGANISM
A Ovum stage: preembryonic stage from conception until the primary villi appear (first 14 days)
B Embryo: end of ovum stage to 8 weeks from LMP; period of rapid cellular development. Disruption causes developmental abnormality.
C Fetus: from end of embryonic stage (8 weeks) to term
D Placenta: membrane weighing approximately 1 pound (450 g); develops cotyledons that act as areas for nourishing fetus; maternal surface beefy and red; fetal surface shiny and gray
E Amnionic cavity: fills with fluid (1000 mL) that is replaced every 3 hours; shelters and protects fetus
GENDER DETERMINATION
A Normal sperm; carries 22 autosomes and 1 sex chromosome (either an X or a Y chromosome)
B Normal ovum: carries 22 autosomes and 1 sex chromosome (always an X chromosome)
C Combined number of chromosomes: 44 autosomes and 2 sex chromosomes (at conception)
D Genetic component of sperm determines gender of child (Box 7-1).
E Chromosome carries genes plus deoxyribonucleic acid (DNA) and proteins
F Genes: factors in chromosomes carrying hereditary characteristics
PHYSIOLOGY OF THE FETUS
A Membranes and amniotic fluid
1. Protect from blows and bumps mother may experience
2. Maintain even heat to fetus
4. Supply oral fluid for fetus
1. Transport organ: passes nutrients from mother to fetus and relays excretory material from fetus to mother
2. Formation completed by 3 months.
3. Functions: acts as kidneys, lungs, stomach, and intestines during fetal life
4. Requirement: adequate oxygen from mother to function well
1. Embryonic stage (first to eighth weeks)
a. Beginning: pulsating heart, spinal canal formation: no eyes or ears; buds for arms and legs
b. By end: just more than 1 inch (2.5 cm) long; eyelids fused; distinct divisions of arms, legs; cord formed; tail disappears
c. The yolk sac begins feeding stem cells to the liver in the fifth week. The actual formation of blood begins in the fetal liver during the sixth week.
d. The liver and biliary tract develop during the fourth week of gestation.
e. The respiratory system begins development during the embryonic stage and continues through childhood.
f. The kidneys form during the fifth week and begin to function approximately 4 weeks later.
g. The nervous system originates from the ectoderm during the third week after fertilization. The open neural tube forms during the fourth week. It usually closes at what will be the junction of the brain and the spinal cord. The neural tube further delineates during the fifth week. The structures that will become the brain and the spine are formed.
h. The thyroid gland develops along with structures in the head and neck during the third and fourth weeks.
2. Fetal stage (ninth week to term)
a. Between 20 and 24 weeks is considered the legal threshold for viability, the age at which the fetus is capable of surviving outside of the uterus. Infants with 22 to 23 weeks of gestation have a better chance of surviving owing to advances in medical care.
b. The embryo or fetus is most vulnerable to damaging effects of teratogenic agents during the first trimester (12 weeks); tetracycline, caffeine, and many over- the-counter drugs are examples of drugs that are teratogenic. The fetus is vulnerable to central nervous system (CNS) depressants during the entire pregnancy.
c. At 3 months: 3 inches (7.5 cm) long; weighs 1 oz (28 g); fully formed arms, legs, fingers; distinguishable sex organs.
d. At 4 months: development of muscles, movement; mother feels quickening; 6 to 7 inches (15 to 17.5 cm) long; weighs 4 oz (112 g); lanugo over body; head large. Until 17 weeks the skin is thin and wrinkled with blood vessels visible. The skin begins to thicken and all layers are present at term. At 32 weeks, subcutaneous fat begins to be deposited.
e. At 5 months: 10 to 12 inches (25 to 30 cm) long; weighs ½ to 1 pound (225 to 450 g); internal organs maturing; lungs immature; FHT heard on examination; eyes fused; rarely survives more than several hours The fetus is able to distinguish taste by the fifth month.
f. At 6 months: 11 to 14 inches (27.5 to 35 cm) long; weighs 1 to 1½ pounds (450 to 675 g); wrinkled “old man” appearance; vernix caseosa covers body; eyelids separated; eyelashes and fingernails formed.
g. At 7 months: begins to store fat and minerals; 16 inches (40 cm) long; may survive with excellent care The fetus can see. Eyes with both rods and cones are formed in the seventh month.
h. At 8 months: beginning of month weighs 2 to 3 pounds (900 to 1350 g); by end of month, 4 to 5 pounds (1800 to 2250 g); continues to develop; loses wrinkled appearance
i. At 9 months: 19 inches (47.5 cm) long; weighs 7 pounds (3200 g) (girl) or 7½ pounds (3400 g) (boy); more fat under skin; vernix caseosa; has stored vitamins, minerals, and antibodies; fully developed
a. Ductus venosus: passes through liver; connects umbilical vein to inferior vena cava (IVC); closes at birth
b. Ductus arteriosus: shunts blood from pulmonary artery to descending aorta; closes almost immediately after birth
c. Foramen ovale: valve opening that allows blood to flow from right to left atrium; functionally closes at birth. All three fetal structures previously listed allow blood to bypass the fetal lungs and liver.
d. Umbilical arteries (two): transport blood from the hypogastric artery to the placenta; functionally close at birth
e. Umbilical vein (one): transports oxygenated blood from the placenta to the ductus venosus and liver, and then to the IVC; closes at birth
2. Fetal circulation (Figure 7-2)
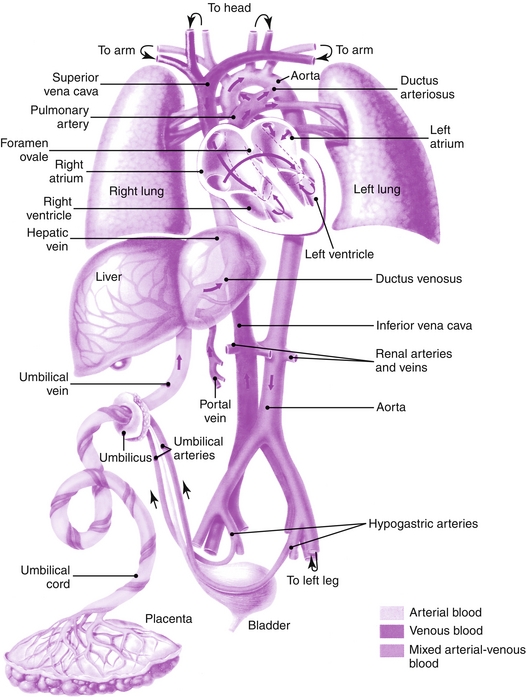
FIGURE 7-2 Fetal circulation. Before birth: Arterialized blood from the placenta flows into the fetus through the umbilical vein and passes rapidly through the liver into the inferior vena cava; it flows through the foramen ovale into the left atrium, soon to appear in the aorta and arteries of the head. A portion bypasses the liver through the ductus venosus. Venous blood from the lower extremities and head passes predominantly into the right atrium, the right ventricle, and then into the descending pulmonary artery and ductus arteriosus. Thus the foramen ovale and the ductus arteriosus act as bypass channels, allowing a large part of the combined cardiac output to return to the placenta without flowing through the lungs. Approximately 55% of the combined ventricular output flows to the placenta; 35% perfuses body tissues; and the remaining 10% flows through the lungs. After birth: The foramen ovale closes, the ductus arteriosus closes and becomes a ligament, the ductus venosus closes and becomes a ligament, and the umbilical vein and arteries close and become ligaments. (Used with permission of Ross Products Division, Abbott Laboratories, Columbus, Ohio.)
a. Oxygenated blood from the placenta goes through the umbilical vein, bypassing the portal system of the liver by way of the ductus venosus.
b. From the ductus venosus it goes to the ascending vena cava (inferior) to the heart, right auricle.
c. It goes from the right auricle through the foramen ovale.
d. It goes to the left auricle and then to the left ventricle.
e. Blood leaves the heart through the aorta to the arms and head.
f. It then returns to the heart, passing through the descending vena cava (superior).
g. It goes to the right auricle and then to the right ventricle.
h. It leaves the heart through the pulmonary arteries, bypassing the lungs.
i. It goes through the ductus arteriosus to the aorta and down to the trunk and lower extremities.
j. It then goes through the hypogastric arteries to the umbilical arteries on to the placenta, carrying carbon dioxide and waste materials.
NORMAL ANTEPARTUM (PRENATAL)
PHYSIOLOGICAL CHANGES DURING PREGNANCY
a. Perineum: increased vasculature; enlarges
b. Labia majora: change especially in parous woman; separate and stretch
c. Anal and vulvar varices: caused by increased pelvic congestion
a. Uterus: enlarges to accommodate growing fetus; walls thicken first trimester; Hegar sign (soft lower lip of uterus)
b. Cervix: Goodell sign (thickens, softens) 6 weeks from LMP because of vascular changes
c. Vagina: Chadwick sign (bluish-violet color); mucosal changes approximately 8 weeks from LMP. Estrogen activity may cause thick vaginal discharge.
a. Slight enlargement of heart resulting from increased blood volume
b. Increased circulation (47%)
c. Cardiac output increases 30% first and second trimesters, then levels off until term; increases during labor and delivery; approximately 13% above normal during postpartum period.
a. Increased red blood cell (RBC) count; decreased hemoglobin level
b. Increased tendency for blood to coagulate during pregnancy
c. Coagulation factors return to normal during postpartum period, increasing likelihood of thromboembolism.
4. Respiratory and pulmonary changes: enlarging uterus presses on diaphragm, causing difficulty breathing
5. Skin: increased pigmentation
a. Linea nigra: darkening line from below breast bone (sternum) down midline of abdomen to symphysis pubis
b. Chloasma gravidarum (mask of pregnancy): dark, frecklelike pigmentation over nose and cheeks; disappears after delivery
c. Striae gravidarum: stretching of skin with silvery to reddish, bluish stretch marks on breasts, abdomen, thighs; never disappears completely. Lotion, cocoa butter lubricants may help.
a. Traces of sugar in urine resulting from activity of lactiferous ducts
b. Even though glucosuria is common in pregnancy, all women should be screened for diabetes.
c. Transitory albumin: may be indication of pending GH
d. Cystitis: frequent because ureters lose some compliance or elasticity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


