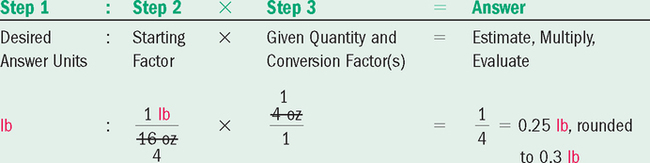
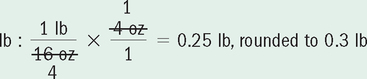
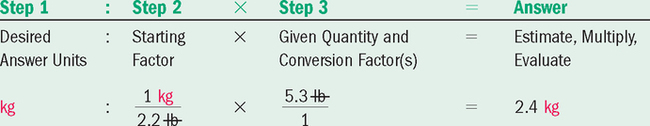
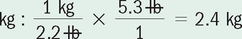
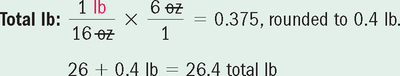
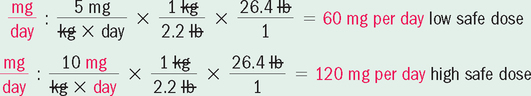
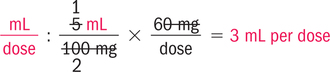
• Distinguish the milligram (mg), microgram (mcg), gram (g), and square meter (m2) units of measurement. • Evaluate orders for minimum and maximum pediatric SDR doses. • Calculate pediatric weight-based doses for oral and parenteral routes. • Calculate pediatric doses based on body surface area. • Calculate flow rates for IV volume-control devices. • State measures to prevent medication errors for pediatric patients. 1. Verifying that the order is within the SDR for the target population 2. Distinguishing microgram, milligram, and square meter units of measurement 3. Calculating accurate fractional doses and fluid needs for all routes 4. Identifying the correct patient when the patient cannot speak 5. Assessing side effects and complications in nonverbal patients The nurse has extra responsibilities to protect the safety of the pediatric patient. The preceding chapters provide a considerable foundation for mastering the calculations in this chapter. Weight-based orders and safe dose ranges for adults have been covered in Chapters 5 and 10. TABLE 13-1 IV Dose Comparison by Age Group for Selected Drugs *A neonate refers to an infant in the first 4 weeks of life. Consult drug references for child age-related dose guidelines. They vary. 1. Which of the recommended SDRs for amoxicillin is weight-based: the adult or the child? (Refer to Table 13-1) 1. Obtain the total body weight in the desired terms. 3. Compare and evaluate the order with the SDR. Contact the prescriber if the order is not within the SDR. • Note that once the total number of pounds is determined, it is entered in the SDR equations with the conversion formula to kilograms. 1. What are the four main steps in the sequence for evaluating and calculating the recommended safe dose? (State your answer using 1 to 3 key words for each step.) 1. A meter is just a little larger than a yard (1 meter = 1.09 yard). If you estimated your BSA in square yards, would you expect the amount to be very small? _____________________________________________ 2. What is my BSA? Use your weight and a calculator to apply one of the BSA formulas. Multiply the numerators, divide by the denominator, and then enter the square root sign. Does the term square meters provide a clue as to size of the result?
Pediatric Medication Calculations
Introduction
![]() Occasionally, young patients receive a higher-than-usual adult dose because of the severity of illness, the threat to life, or the lack of response to lower doses and other medications. The particular emphases for safe medication administration with pediatric populations, beyond the selection of appropriate equipment and sites for the medications, are:
Occasionally, young patients receive a higher-than-usual adult dose because of the severity of illness, the threat to life, or the lack of response to lower doses and other medications. The particular emphases for safe medication administration with pediatric populations, beyond the selection of appropriate equipment and sites for the medications, are:
![]() Pediatric patients cannot protect themselves from medication errors. Many cannot identify themselves and are not in a position to question medications and medication orders or to verbalize physical complaints. In addition to using printed identification bracelets, bar codes, and other methods, the nurse should have a family member verify the identity of a pediatric patient.
Pediatric patients cannot protect themselves from medication errors. Many cannot identify themselves and are not in a position to question medications and medication orders or to verbalize physical complaints. In addition to using printed identification bracelets, bar codes, and other methods, the nurse should have a family member verify the identity of a pediatric patient.
![]() Pediatric patients suffer a much higher rate of medication errors than adults.
Pediatric patients suffer a much higher rate of medication errors than adults.
Comparing Adult and Pediatric Medication Doses and Schedules
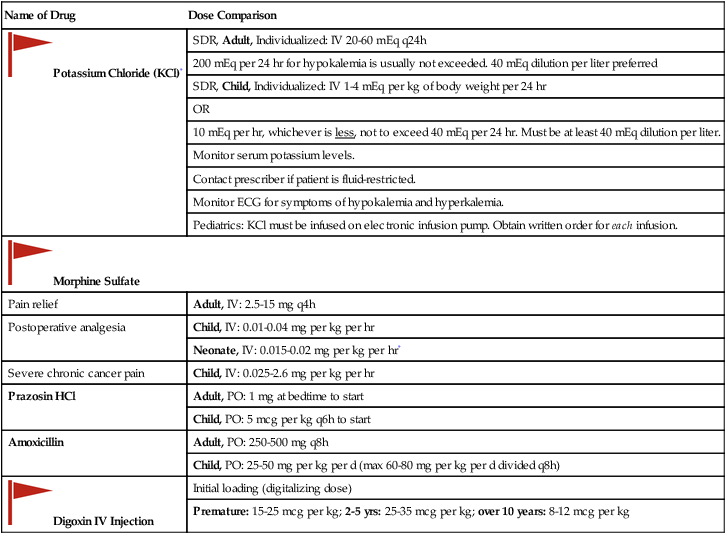
![]() Examine the selected examples in Table 13-1, and note the differences in dosing and units of measurement for adults and children.
Examine the selected examples in Table 13-1, and note the differences in dosing and units of measurement for adults and children.
Name of Drug
Dose Comparison
![]() Potassium Chloride (KCl)*
Potassium Chloride (KCl)*
SDR, Adult, Individualized: IV 20-60 mEq q24h
200 mEq per 24 hr for hypokalemia is usually not exceeded. 40 mEq dilution per liter preferred
SDR, Child, Individualized: IV 1-4 mEq per kg of body weight per 24 hr
OR
10 mEq per hr, whichever is less, not to exceed 40 mEq per 24 hr. Must be at least 40 mEq dilution per liter.
Monitor serum potassium levels.
Contact prescriber if patient is fluid-restricted.
Monitor ECG for symptoms of hypokalemia and hyperkalemia.
Pediatrics: KCl must be infused on electronic infusion pump. Obtain written order for each infusion.
![]() Morphine Sulfate
Morphine Sulfate
Pain relief
Adult, IV: 2.5-15 mg q4h
Postoperative analgesia
Child, IV: 0.01-0.04 mg per kg per hr
Neonate, IV: 0.015-0.02 mg per kg per hr*
Severe chronic cancer pain
Child, IV: 0.025-2.6 mg per kg per hr
Prazosin HCl
Adult, PO: 1 mg at bedtime to start
Child, PO: 5 mcg per kg q6h to start
Amoxicillin
Adult, PO: 250-500 mg q8h
Child, PO: 25-50 mg per kg per d (max 60-80 mg per kg per d divided q8h)
![]() Digoxin IV Injection
Digoxin IV Injection
Initial loading (digitalizing dose)
Premature: 15-25 mcg per kg; 2-5 yrs: 25-35 mcg per kg; over 10 years: 8-12 mcg per kg
![]() Taking 2 or 3 minutes to verify a safe dose order with a current pediatric drug reference and/or pharmacy may prevent a tragic error.
Taking 2 or 3 minutes to verify a safe dose order with a current pediatric drug reference and/or pharmacy may prevent a tragic error.
Sequence for Calculating Safe Dose Range (SDR)
![]() Review the logic and example of the multi-step process for evaluating an order for safe dose. A calculator is helpful.
Review the logic and example of the multi-step process for evaluating an order for safe dose. A calculator is helpful.
![]() 4 If the order is safe, estimate, calculate, and evaluate the dose.
4 If the order is safe, estimate, calculate, and evaluate the dose.
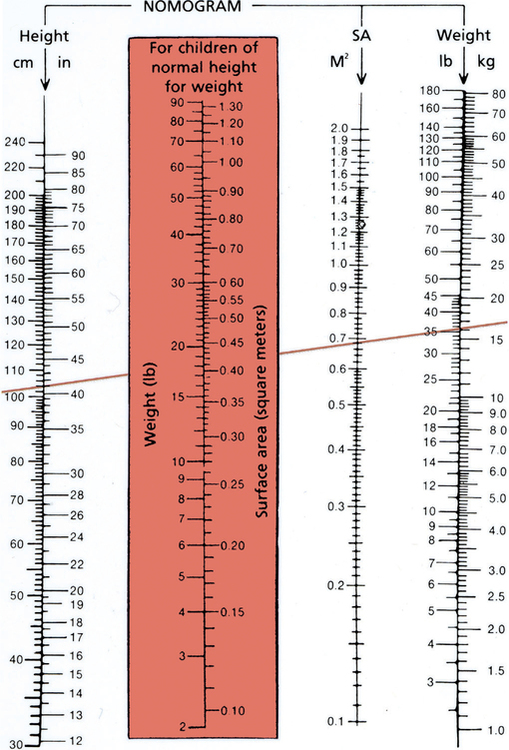
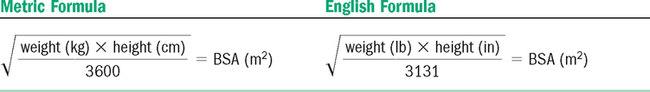
Body Surface Area (BSA)
![]() The nurse is expected to be able to define BSA, identify square meters, and, most important, distinguish among m2 and mg and mcg metric measurements when reading orders, medication records, and current drug references and when calculating SDR. The nurse rarely calculates the BSA. Pharmacy usually supplies it.
The nurse is expected to be able to define BSA, identify square meters, and, most important, distinguish among m2 and mg and mcg metric measurements when reading orders, medication records, and current drug references and when calculating SDR. The nurse rarely calculates the BSA. Pharmacy usually supplies it.
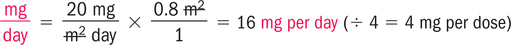
Calculating milligrams per square meter (mg per m2)
![]() The calculation of milligrams per square meter is performed using a DA-style equation or simple multiplication, just as it is for calculating milligrams per kilogram (e.g., 2 mg per m2 means “2 milligrams of medicine for each square meter of body surface area”).
The calculation of milligrams per square meter is performed using a DA-style equation or simple multiplication, just as it is for calculating milligrams per kilogram (e.g., 2 mg per m2 means “2 milligrams of medicine for each square meter of body surface area”).
![]() Pay close attention to the placement of decimal points. Square meters of BSA are very small amounts. A missing decimal point would result in a tenfold dose error.
Pay close attention to the placement of decimal points. Square meters of BSA are very small amounts. A missing decimal point would result in a tenfold dose error.
![]() Pediatric doses are calculated to the nearest hundredth of a mL. Check agency policies.
Pediatric doses are calculated to the nearest hundredth of a mL. Check agency policies.