Pain Resource Nurse Program and Monthly Chart Audits Improve Pediatric Pain Assessment
Sonja Jones MSN, RN, CPN1
Renee Green BSN, RN2
Elizabeth Carroll BSN, RN3
Denise Zubczynski BSN, RN, CPN4
Colleen Foster BSN, RN5
Susan M. Kolb MSN, CRNP6
Beth Ely PhD, RN7
1Nurse Manager, 4East/4South
joness@email.chop.edu
2Clinical Level III Staff Nurse, 4East/4South
3Clinical Level III Staff Nurse, 4East/4South
4Clinical Level III Staff Nurse, 7West
5Clinical Level IV Staff Nurse, 7West
6Director, Advanced Practice Nursing
7Nurse Researcher
Children’s Hospital of Philadelphia Philadelphia, Pennsylvania
www.chop.edu
Case Study Highlights
A combination of hospital-wide efforts and unique unit-based strategies led to improved pain assessment practices. Hospital-wide efforts included the development of a pain resource nurse (PRN) program with unit-based champions. Modification of the Patient Care Flowsheet was instrumental in improving pain assessment documentation. Unit-specific efforts included chart audits with direct individual coaching of nurses at the point of care.
Identification of the Problem
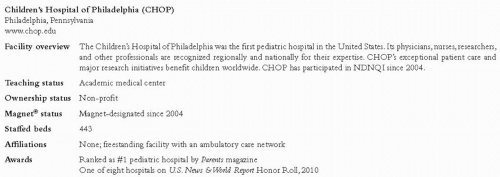
The Quality Practice and Patient Safety (QPPS) Council at Children’s Hospital of Philadelphia (CHOP; see Figure 1) determined that its pain assessment-intervention-reassessment (AIR) cycle documentation was falling below the national median reported by NDNQI®. The need for improved pain management practices was reinforced when feedback from a Joint Commission visit in early 2007 indicated documentation of pain reassessment was inconsistent. Hospital-wide and unit-specific efforts from 2007 to 2009 have brought improvements in both frequency of pain assessments and the completion of AIR cycles.
Pain Resource Nurse Program
In the fall of 2006, CHOP hired several doctorally prepared nurses to form a center for nursing research and evidence-based practice. One of these nurses started a pain resource nurse program, bringing together nurses with an interest and expertise in pain management from all areas of practice represented in the hospital’s QPPS Council. The group began meeting in December 2006 to identify areas of pain management that needed improvement and to promote a rapid turnaround time when planning and implementing any proposed changes. When the Joint Commission visit in early 2007 brought pain reassessment documentation to the forefront, nursing leadership identified the QPPS Council and the PRN subcommittee as the logical place to formulate and carry out an improvement plan. Nurses on the PRN subcommittee polled staff on their units and reviewed NDNQI data from the previous four quarters to better understand where and how to focus the improvement strategies.
Development of Hospital-Wide Initiatives
Three hospital-wide initiatives have improved pain management practices: revisions to the daily nursing documentation form, selection of a new assessment tool for children with cognitive impairment, and expansion of the PRN group’s activities.
As of early 2007, charting pain management required access to three separate areas of the Patient Care Flowsheet as well as electronic charting of medication administration. On the front of the Patient Care Flowsheet, a pain intensity score was documented along with vital signs and daily weights. However, the interventions
provided and subsequent pain reassessments were charted in a different section of the flowsheet. Finally, nursing notes related to pain were located at the back of the document. Nurses polled by the PRN group indicated that paper documentation was a major barrier to actually recording assessment scores since disjointed and duplicate documentation was required and they were often too busy.
provided and subsequent pain reassessments were charted in a different section of the flowsheet. Finally, nursing notes related to pain were located at the back of the document. Nurses polled by the PRN group indicated that paper documentation was a major barrier to actually recording assessment scores since disjointed and duplicate documentation was required and they were often too busy.
Revisions to the daily nursing documentation form were made to co-locate all pain assessment data for a more logical flow of information. In addition, coded lists of common pain management interventions were provided, rather than having to repeatedly write out common interventions. The form was revised with input from QPPS, shared governance council members, and unit staff. In August 2007, the new flowsheet (see Figure 2) was rolled out with education at the hospital’s QPPS Council meeting and through unitlevel QPPS meetings.
The PRN subcommittee recognized the need to review evidence related to pain assessment in children with cognitive or neurologic impairment, a population cared for frequently at this hospital. A small workgroup (staff nurses, clinical nurse specialists [CNSs], nurse researcher) was charged with this task. From an extensive literature review, the workgroup identified two promising pain assessment tools for children with cognitive impairment: the Pediatric Pain Profile (PPP) and the revised Face-Legs-Activity-Cry-Consolability (rFLACC) Scale (Hunt et al., 2004; Hunt et al., 2007; Malviya, Voepel-Lewis, Burke, Merkel, & Tait, 2006; Voepel-Lewis, Malviya, & Tait, 2005; Voepel-Lewis, Merkel, Tait, Trzcinka, & Malviya, 2002). The choice of these tools was based on their published psychometric properties as well as judgments about clinical utility by group members. Each tool was designed to include parentS’ input by identifying common pain behaviors of the child. To obtain feedback on applicability, clinical utility, preference for use, and time to complete for each tool, the tools were introduced to parents at the hospital’s Family Advisory Council and to staff nurses through a formal quality improvement (QI) project.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree