Two-Tier Fall Precautions Combined with Improved Staffing and New Equipment Reduce Injury Fall Rates
Scott Madaris MSHSA, BSN, RN
Director of Clinical Education/Nursing Quality/Magnet Program Director
Scott_Madaris@memorial.org
Memorial Hospital Chattanooga, Tennessee
www.memorial.org
Case Study Highlights
A two-tier approach to fall prevention led to zero injury falls on six medical and surgical units. New bed alarms, an algorithm for sitter usage, and a lower nurse—patient ratio were key structural changes that helped sustain the improvement. Lessons learned from post-fall huddles will be used to continue injury fall prevention efforts.
Quality Measurement and Organizational Structure
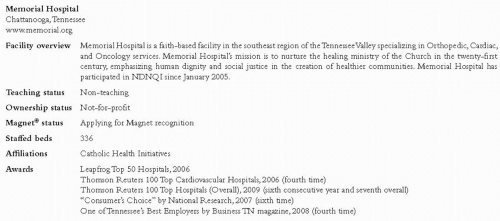
In January 2005, Memorial Hospital (see Figure 1) chose to participate in NDNQI® as an opportunity to seek out national nursing quality benchmarks. As Memorial moved forward in utilizing nursing-sensitive data, a shared governance design was formulated to involve bedside nurses in practice decisions and nursing-related policies. Memorial’s Nurse Practice Council membership has evolved over time and is now composed of an elected staff nurse chair and co-chair, voting members from all inpatient and outpatient nursing areas, and non-voting representatives from the Pharmacy, Advanced Practice Nursing, Quality, and Risk Management departments.
Over the last two years, the Nursing Quality Council was redesigned and incorporated with the Nurse Practice Council. This merger brought quality decisions that affect clinical practice to the forefront, empowering nursing staff to provide insight and be involved with quality improvement. With this change in governance structure there have been several initiatives, including fall reduction, that have brought more evidence-based practices to the bedside.
Problem Identification
The Restraint and Fall Committee examined monthly fall data and used NDNQI benchmarks to evaluate total and injury fall rates. In November 2007, discussion about revising the existing fall prevention program began. Staff and nursing leadership determined that the previous fall program was no longer effective. Multiple acute care nursing units had injury fall rates above the NDNQI mean in 3Q07 and there had been several falls with major injuries.
The Restraint and Fall Committee noted several factors contributing to injury falls. At this time, patients were assessed for fall risk using clinical judgment, not a risk assessment tool. Fall signage was either being ignored by staff or not placed appropriately based on clinical assessment. Falls were often associated with patients getting up to use the bathroom. The Committee began working to design a prevention program, with the goal of achieving a zero injury fall rate.
Development of a Two-Tier Fall Reduction Program
To improve fall risk assessment and fall signage, the Committee gathered information about current practice, policy, and clinical tools. Fall identification bracelets with a “falling star” were already being used to distinguish at-risk patients, but assessment of risk needed to be standardized. The literature spoke of signage that not only alerted staff to potential fall risk, but also involved the patients, family, and visitors. Thus, new risk assessment tools and “traffic light” signs were trialed on two units with high-risk populations and increased fall rates. After the trial, nursing staff said that the new fall signage was helpful and prompted triggers related to fall criteria, room clutter, and the use of fall risk identification bracelets. However, they stated the assessment tools were cumbersome and that “most patients became fall risks” based on the criteria used. After further discussion and analysis, it was concluded that most patients in the healthcare setting are at risk for falls, which generated discussion of a two-tier fall prevention process.
The first tier utilizes the concept of “standard” fall precautions for all acute care patients and includes basic fall reduction techniques, such as patient and family education, reduction of room clutter, placing the patient call light in reach, use of slipper socks, and utilization of assistive devices such as gait belts with transfer and ambulation. The second tier applies to patients with advanced age, equipment (such as IV pumps or other attached equipment), history of falls within the past year, or physical or cognitive impairments. At the second tier, patients would be placed on “strict” fall precautions which initially included fall signage (alert bracelets, yellow socks, “traffic light” signs, and
so forth), and hourly rounding. Bed alarms were later added for second-tier patients. These fall precautions were designed to catch falls before they happened, thereby reducing the risk of injury.
so forth), and hourly rounding. Bed alarms were later added for second-tier patients. These fall precautions were designed to catch falls before they happened, thereby reducing the risk of injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree