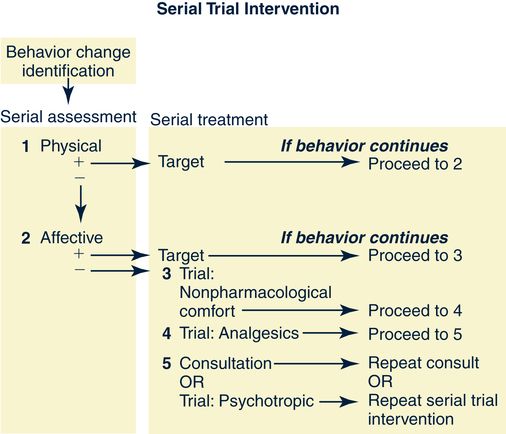
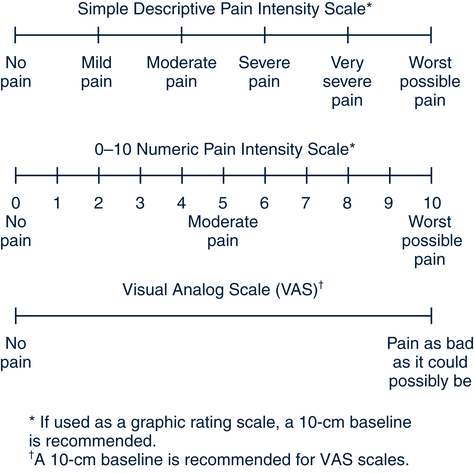
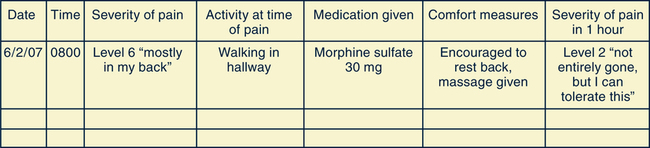
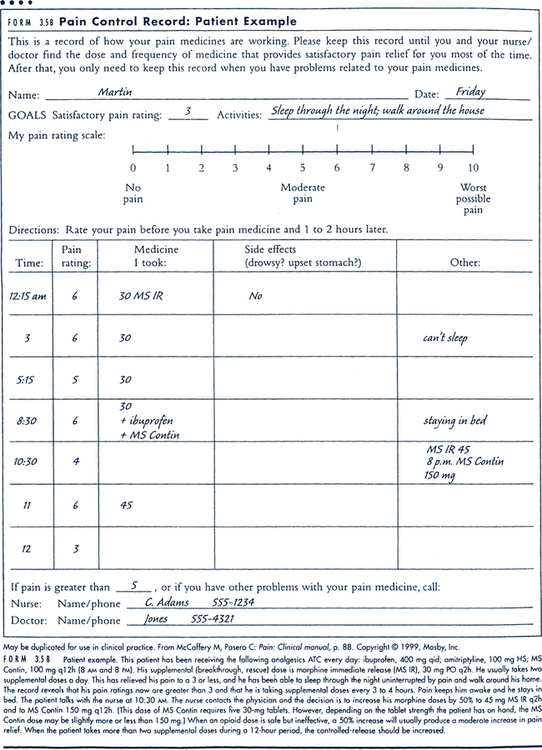
Sue E. Meiner, EdD, APRN, BC, GNP On completion of this chapter, the reader will be able to: 1. Define the concept of pain, including types and sources. 2. Identify the potential effects of pain on an older adult. 3. Discuss the goals of pain management in older adults. 4. Identify barriers that affect the assessment of pain or its management in older adult clients. 5. Describe the effect of pain on the quality of life of older adult clients. 6. Identify factors that may affect older adults’ pain experiences. 7. Use a pain assessment tool to rate clients’ pain intensity. 8. Describe the use of pharmacologic and nonpharmacologic therapies for older adults with pain. Pain has long been recognized as a symptom of something else in the body. Pain has often been referred to as the fifth vital sign. When all of the body systems are working together well, pain should not be felt. These are facts, whereas pain as an expectation of aging is a myth. There are many misconceptions about pain and age; predominant among the ones held by health care professionals is the myth that pain is a normal aspect of growing old (Pasero, Reed, & McCaffery, 1999). Pain is underrecognized, highly prevalent, and undertreated among older adults, especially when cognition is impaired. Hanks-Bell et al (2004) found that the incidence of pain more than doubles after the age of 60. Many health care practitioners have only encountered older adults in an emergency room or in hospitals, where they are in need of unusually intense medical or nursing treatment; this is not a good way to understand that these patients are not representative of normal aging. However, older adults are at high risk for pain-inducing situations during their life span. Degenerative changes and pathologic and comorbid conditions from disease or injury lead to pain in the elderly (Hanks-Bell et al, 2004; Herr & Decker, 2004). Understanding pain and how to efficaciously treat it calls for a look at how pain is defined. There are multiple definitions of pain; most include the mind–body relationship. According to some, pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage (McCaffery, Frock, & Garguilo, 2003). McCaffery (2000) further states that pain is “whatever the experiencing person says it is, existing whenever he or she says it does.” Aronoff’s (2002) definition is more specific: “a subjective, personal, unpleasant experience involving sensations and perceptions that may or may not relate to bodily or tissue damage.” Pain is also defined as an unpleasant sensory and emotional experience (Merskey & Bogduk, 1994). The literature on pain is in agreement that pain is (1) a complex phenomenon derived from sensory stimuli or neurologic injury and modified by individual memory, expectations, and emotions (Sternbach, 1978) and (2) usually associated with injury or a pathophysiologic process that causes an uncomfortable experience. These authors clearly note that pain is individual and can be very different for different persons with the same disease or injury. Pain can be defined as acute or chronic. Acute pain is defined by rapid onset and relatively short duration and a sign of a new health problem requiring diagnosis and analgesia. Treatment usually involves treating the underlying disease or injury and short-term use of analgesics. In contrast, chronic or persistent pain continues after healing or is not amenable to a cure. This pain usually has no autonomic signs and is associated with long-standing functional and psychologic impairment. It is likely to require a multidimensional approach for relief (Kedziera, 2001). The American Geriatrics Society (AGS) (2002) advocates the use of the term persistent rather than chronic pain, which may be associated with negative images and stereotypes. The AGS Panel on Persistent Pain identified four categories of pain that encompass most syndromes (Box 15–1) (AGS, 2002): 1. Nociceptive pain may be visceral or somatic and is usually a result of stimulation of pain receptors. It may arise from tissue inflammation, mechanical deformation, ongoing injury, or destruction of tissue. This type of pain usually responds well to common analgesic medication and nonpharmacologic strategies. 2. Neuropathic pain results from a pathophysiologic process involving the peripheral or central nervous system. These types of pain do not respond as predictably to analgesic therapy as do nociceptive types of pain. They do, however, respond to unconventional analgesic drugs, such as tricyclic antidepressants, anticonvulsants, or antiarrhythmic drugs. 3. Mixed or unspecified pain has mixed or unknown mechanisms. Treatment is unpredictable and may require more trials of different or combined approaches. 4. Other types of pain may be rare conditions such as conversion reaction or psychologic disorders. Persons with these disorders may benefit from specific psychiatric treatments, but traditional medical interventions for analgesia are not indicated. Age-associated changes in pain perception have been observed in some older persons with unusual manifestations of common illnesses. Neuroanatomic and neurochemical findings have shown that the perception of pain and its treatment in the central nervous system are elaborate and complex (Gibson & Helme, 2001). Alteration of transmission along A-delta and C-nerve fibers may be associated with aging, but it is not clear how it affects the individual experience of pain (Chakour et al, 1996). An AGS panel concluded age-related changes in pain perception are probably not clinically significant (AGS, 2002). Even though pain is not part of normal, healthy aging, pain is a common problem among older adults, and persistent physical pain is widespread in the older population (AGS, 2002). It is estimated that 50% of community-dwelling older adults experience significant pain problems (Herr, 2002; Mosby et al, 1994). A Louis Harris telephone survey found that nearly 20% of older Americans are taking analgesic medications regularly (several times a week or more), and 63% had taken prescription pain medications for more than 6 months (Cooner & Amorosi, 1997). Pain is even greater in nursing homes, where it has been shown that 70% to 80% of residents have substantial pain that is undertreated (AGS, 2002; Ferrell, 1995; Weiner, Peterson, & Keefe, 1999; Werner et al, 1998). Stereotyping older persons as having less pain because of their age contributes to less frequent pain assessment and consequently less appropriate and effective treatment for the pain. Older adults commonly report less pain because they do not want to be complainers, fear more tests and medicines, and fear losing their independence (AGS, 2002). In addition, older adults have been told that they will have pain at sometime in their later years. Thus they become resigned to the expectation of pain. The fear that pain will be seen as a reason for losing independent living is associated with a reluctance to express pain freely to nonfamily members. Older adults may be ambivalent about the benefit of any action for their pain. Some of these responses by older persons may be due to health practitioners saying, “What do you expect at your age?” which supports the belief that nothing can be done to control or stop the pain. Consequences of persistent pain are numerous. Depression, anxiety, decreased socialization, sleep disturbance, decreased or impaired ambulation, prolonged recovery periods, increased use of health care resources, premature death, and increased health care use and costs have all been documented with the presence of pain in older patients (Agency for Health Care Policy and Research [AHCPR], 1994; Carson & Mitchell, 1998). Unrelieved pain has been shown to result in decreased ambulation, impaired posture, sleep disturbance, anxiety, and impaired appetite in nursing home residents. Pain can make getting to the bathroom so difficult that incontinence occurs. Constipation can also be related to unrelieved pain when the person changes diet plans, decreases activity, and has difficulty getting to a toilet before the urge passes (Ferrell, Ferrell, & Osterweil, 1990). Weiner and Rudy (2002) found that nursing home residents who were functionally disabled believed that the staff labeled them as less deserving of pain treatment than more independent residents. Pain research and literature on pain management have increased dramatically over the past four decades. Despite these advances, pain remains underrecognized and undertreated in older adults, especially those 75 or older. This situation has developed because the study of pain has generally been limited to the young and to those with cancer-related pain in acute care settings. More recently, though, studies have focused on the special needs of older adults in other care settings such as the nursing facility (Loeb, 1999; Morley et al, 1995; Stein & Ferrell, 1996; Wagner et al, 1997), the home, and the community (Cooner & Amorosi, 1997; Huber & Spirig, 2004; Keefe et al, 2004; Mosby et al, 1994). Pain in cognitively impaired older adults is a relatively new field of inquiry (Farrell, Katz, & Helme, 1996; Ferrell, Ferrell, & Rivera, 1995; Kovach et al, 2001) along with gender differences in pain response (Bradbury, 2003; Giles & Walker, 2000; Vallerand, 1995). Accountability for undertreatment of pain is also gaining attention, given the results of court cases against professionals who undertreat pain in older adults (Pasero & McCaffery, 2001). • Control of chronic disease conditions causing pain • Maintenance of mobility and functional status • Promotion of self-care and maximum independence The causes of pain in older adults are both chronic and acute. Chronic diseases that cause pain are especially prevalent in this age group. Some of the major chronic illnesses causing pain in older adults are arthritis, polymyalgia rheumatica, temporal arteritis, peripheral vascular disease, diabetic neuropathy, postherpetic neuralgia, and cancer. It is suggested that sex hormones influence the neural circuitry that detects and controls pain, although their role has not been clearly identified (Giles & Walker, 2000). The three major components of the nervous system that cause the sensation and perception of pain are the afferent pathways (reception), central nervous system (perception), and efferent pathways (reaction). Afferent pathways have nociceptors and are found on the skin. Pacinian corpuscles that mediate sensation, including pain, pressure, and itching, are the nerve endings that are distributed in the skin. Stimulation of these nerve endings by vibrations from massage or sound waves can reduce the perception of pain in conditions such as chronic rheumatoid arthritis. The free nerve endings of nociceptors are sensitive to mechanical, thermal, electrical, or chemical stimuli and are responsible for transmitting sensory pain information. This stimulation flows through peripheral sensory nerves (afferent pathways) to the spinal cord. A painful stimulus (e.g., a pinprick) sends an impulse to a nociceptor (a receptor for painful stimuli) along a peripheral nerve fiber, which enters the gray matter of the spinal cord. Nociceptors terminate in the spinal cord (McCaffery & Pasero, 1999). Here the nociceptor stimulation flows to the brain through a series of relay neurons. When the pain stimulus or signal reaches the central nervous system, it is evaluated and interpreted in the limbic system, reticular formation, thalamus, hypothalamus, medulla, and cerebral cortex. The brain’s interpretation is based on both physical and psychologic factors. Modulation of the pain stimulus can occur in the gray matter, the dorsal horn of the cord. Here, transmission occurs from the nociceptor to the spinothalamic tract neuron. Substance P, a neurotransmitter, facilitates transmission of the stimulus from the afferent (peripheral) neuron across the synapse to the spinothalamic tract neuron. Uninhibited by medications or other modalities, the pain impulse travels to the cerebral cortex of the brain, where the brain interprets the quality of pain, processing past experiences with pain, knowledge of pain, and cultural associations related to pain perception. The interpretation is relayed back through the peripheral nervous system (efferent) pathways that are made up of fibers connecting the reticular formation, midbrain, and substantia gelantinosa. Pain modulation takes place in the efferent neural pathways and may involve chemical factors of neuropeptides, which can increase the sensitivity of the afferent pain receptors to noxious stimuli. These pathways result in the sensation and perception of pain (McCance & Huether, 2002.) The mind–body connection of pain can be affected by mind–body therapies that are useful in reducing symptoms of pain, especially persistent (chronic) pain. Some mind–body therapies are meditation, relaxation, guided imagery, and cognitive behavioral counseling. Study findings also reveal that factors such as emotion, attitudes, and stress can directly influence physiologic functions and health outcomes (Astin et al, 2003). A more detailed explanation may be obtained in any extensive book or chapter on pain physiology. Atypical silent myocardial infarction occurs more commonly in older adults. The acute pain of appendicitis in young adults is often not experienced by older adults (McCaffery & Pasero, 1999). The reason for this difference is unknown. Nevertheless, studies demonstrate that older adults have the same intensity of pain as younger adults and are as sensitive to it (Harkins & Scott, 1996). Older persons may have decreased pain tolerance (Leo & Huether, 1998). Laboratory study findings that suggest an age-related decline in pain sensitivity and perception are questionable (Ferrell, Rhiner, & Ferrell, 1993; Harkins & Scott, 1996). One review concluded that age has no significant effect on the perception of acute pain (Harkins & Scott, 1996). Furthermore, both the intensity and frequency of pain increase with increasing age. Pain sensitivity and perception should be examined in relation to analgesic use, coexisting disease, and comorbid conditions. Nurses working with pain in the elderly need to develop the knowledge and skill to aggressively treat pain. However, regulatory scrutiny requiring pain assessment documentation, medication determination according to a physician’s orders, the signing out of narcotics, dispensing of the medication, and follow-up documentation causes some nurses to fear the process of providing controlled substances to patients with pain (Hanks-Bell, 2004). Inadequate access to diagnostic services is another barrier to appropriate pain assessment for older residents of nursing facilities and frail older adults in the community. Often it is difficult to schedule appointments and arrange transportation so that a family member or health care professional can accompany the client to a diagnostic testing facility. Furthermore, many older adults do not have children who live near them and have lost their social networks (Luggen & Rini, 1995). Pain assessment tools such as visual analog scales, word descriptor scales, and numeric scales have not been validated in the older adult population. Cognitive, visual, hearing, and motor impairments may prevent accurate use of these pain assessment methods. When using any pain assessment tool, the nurse must evaluate each client’s ability to give accurate responses with that tool. The use of a second tool may help confirm the value obtained with the first tool. The AGS (2002) found that the most accurate and reliable indicator of pain intensity and experience is the patient’s self-report. An additional barrier to effective pain management may be the nurse’s extensive use of pain-related behavior assessment to identify and validate the presence of pain in older adults with dementia. Confused older adult clients have difficulty interpreting painful stimuli. They may be unable to identify its location or communicate the nature of their distress to caregivers (Wold, 1999). They do not respond to pain typically. They may demonstrate changes in body language, vital signs, and level of confusion as indicators of pain. Pain may result in agitation, as well as increased pulse, respiration, blood pressure, and confusion (Wold, 1999). Researchers have tried to verify pain behaviors such as facial grimacing, agitation, restlessness, groaning, and attempting to leave or escape as valid signs indicating pain. However, the assessment of pain through behavior indicators should be done with caution because clients in pain may not portray any visible signs of pain or distress or may be unable to communicate their pain. The compromised ability of people with moderate to severe dementia to clearly or consistently report on their internal states provides both challenges and opportunities to nurses who want to improve care and comfort. The Serial Trial Care Protocol (STCP), developed to assess and treat physical pain and affective discomfort in people with dementia who are no longer able to clearly and consistently verbalize needs, addresses critical steps in the breakdown and disconnection between nurses’ understanding of the person’s need and the provision of care for that unmet need (Fig. 15–1). The STCP is an innovative approach that has concrete specifications but allows discretion in individualizing assessments of and interventions for the situation. The STCP is based on the assumption that behaviors associated with dementia (e.g., fidgeting, exiting, pacing, decreased appetite, and combative behavior) signal an unmet need. When the sources of these behaviors are not easily identified, the nurse begins the STCP protocol by doing a physical assessment. If the physical assessment reveals a problem, the nurse institutes an intervention to target the problem. If the physical assessment is negative or the intervention provided is ineffective in returning behaviors to baseline, the nurse assesses for common psychosocial and environmental needs. Intervention trials are pharmacologic or nonpharmacologic treatments provided when specific domains of assessment or intervention have failed to uncover the source of the problem or failed to ameliorate behaviors. The STCP is a systematic process for using intervention trials that proceeds from nonpharmacologic comfort interventions, to a trial of analgesics, and then perhaps to a trial of psychotropics (Kovach, 2004). Studies have documented that physicians and nurses tend to underestimate their clients’ pain. This seems to be based on limited education and on the belief that older adults have less sensitivity to pain, which has not been demonstrated. Older adult clients actually underreport pain and are therefore at risk for undertreatment of pain, which may cause unnecessary suffering, exacerbation of the underlying disease, and reduction in ADLs and quality of life. Nurses must always be aware of the negative influence ageism has on pain management for older adults (Keefe et al, 2004). For health care professionals, clients, and their families, fear of addiction is a barrier to effective pain management. However, the risk of addiction is not an issue for those older adults who require opioids for pain relief. In fact, because of side effects, especially constipation, older adults have a high rate of discontinuation of opiates (Reuben, Yoshikawa, & Besdine, 1996). The treatment for constipation, especially that which is opioid induced, is readily available and should be provided before starting narcotic pain medication as a preventive measure. Nonetheless, clinicians are reluctant to provide opioids to those with chronic painful conditions in a community setting (American Academy of Pain Medicine [AAPM] and American Pain Society [APS], 1997). Unwarranted fear of addiction should not inhibit the appropriate use of pain-relieving medications. Tolerance to opioids may occur a few days after treatment (McCaffery & Pasero, 1999), which supports the need for monitoring for a period. Tolerance is defined as the diminished effect of a drug while maintaining the same dosage over time. With opiates, some individuals might need higher and higher doses of a drug to maintain effectiveness. This should not be confused with addiction; it is a characteristic of these drugs when given over time. The drug dosage must be increased to avoid causing needless pain to patients. There are few ceiling effects (level for effectiveness of the drug) for the amount of drug that can be given, in contrast to drugs that have a level at which additional drug does not offer increased relief. Tolerance to the nonanalgesic effects (i.e., the side effects) of opioids can also develop (McCaffery & Pasero, 1999). Tolerance to nausea and mental clouding, which commonly occur when the drug is first given, will develop. These symptoms diminish in days or weeks. However, tolerance to constipation does not occur, so no program of pain relief with opiates should be started without an accompanying bowel regimen, including diet, fluids, activity, and stool softeners. Inadequacy of the pain education provided to medical and nursing students is also a barrier to effective pain management (Gloth, 2000). Changes in demographics and health care delivery, as well as increasing research, have increased the awareness of the prevalence of pain (Davis, 1998). As Gloth (2000) notes, “It is difficult to find space for additional instruction in a busy medical school curriculum but here remains a disproportionate allotment to subjects such as obstetrics (which many physicians use very little), compared with pain management and care of the dying (which most physicians will encounter, regardless of specialty).” Lack of education does not fully account for undertreatment of pain. It is a multifaceted problem (McCaffery & Pasero, 1999). Institutional rituals of practice and care are persistent barriers to effective pain management. An interdisciplinary team approach can provide the impetus for blending continuous quality improvement with other strategies for changing systems and practices, such as those described in the Client/Family Teaching box. The pharmacodynamics and the pharmacokinetics of commonly prescribed medications are different in older adults than in individuals in other age groups (see Chapter 22). Older adults are especially vulnerable to the effects of drugs because of age-related physiologic changes and altered pharmacodynamics. The limited research in this area supports the importance of starting with low doses and slowly titrating upward until the desired effect is achieved (Nagle & Erwin, 1996). Inadequate treatment of pain in older people may ultimately lead to legal action. In 2001 a California court found a doctor guilty of recklessness and abuse under California’s Elder Abuse and Dependent Adult Care Protection Act (Pasero & McCaffery, 2001). The charge was one of not providing adequate pain medication for an 85-year-old man with cancer pain. An increased number of cases of this type are expected in the future. To reduce the risk of such legal action, institutional guidelines and education for individual nurses and physicians are suggested (Pasero & McCaffery, 2001). Guidelines for pain treatment, as suggested by Yonan and Wegener (2003), include using a baseline report of activity or pain level of the individual to set the initial goals for pain treatment outcomes; these outcomes should be at about 75% of the established baseline for the individual. This is believed to be a reasonable initial goal for pain control. Pain assessment begins when the nurse accepts the person’s report of pain and takes that report seriously. Assessment is essential in differentiating acute life-threatening pain from long-standing chronic pain. Otherwise, disease progression and acute injury may go unrecognized and be attributed to preexisting disease or illness. Table 15–1 identifies components of the clinical assessment of pain in older adults. TABLE 15–1 ASSESSMENT OF PAIN IN OLDER ADULTS From American Geriatrics Society Panel on Chronic Pain in Older Persons: Clinical practice guidelines, J Am Geriatr Soc 46:635, 1998. Pain assessment should include a thorough history and a physical examination. These assessments are especially important for older persons because effective pain management often depends on the appropriate treatment of underlying disease or illness. When the underlying disease is unknown, multidisciplinary consultation is indicated (AGS, 2002; Linton & Lach, 2007). • There are no biologic markers for the presence of pain. • The client’s report is the most accurate and reliable evidence of pain and its intensity. • Clients with mild to moderate cognitive impairment can be assessed with simple questions and screening tools. • Older clients may be reluctant to report pain despite substantial impairments. • Older persons expect pain with aging. • Older adults may use words like discomfort, aching, and hurting rather than pain. • They may see pain as a metaphor for serious disease or death. • Pain may represent “God’s will” or atonement for “bad” deeds. • Assess clients for evidence of chronic pain. • Recognize pain that significantly affects functional ability or quality of life as a significant problem. • For clients with cognitive or language impairments, observe nonverbal pain behaviors, recent functional changes, and vocalizations (e.g., groans and cries). • For clients with cognitive or language impairments, seek caregiver reports and input. • Seek specialist consultation for clients with debilitating psychiatric problems, substance abuse problems, or intractable pain. • Monitor clients with chronic pain by recording pain intensity, medication use, response, and associated activities in a pain log or diary. • Reassess all clients with chronic pain regularly for improvement, deterioration, positive or negative effects of medications, and complications of treatment. Use the same pain instruments at each client visit. Little research has been conducted on pain in clients of any age from different cultures. Because of increasing racial and ethnic diversity in the United States, nurses must work closely with culturally diverse clients to identify mutual goals, including clients’ preferences about specific remedies and practices from their culture (McCaffery & Pasero, 1999; Sakauye, 2005) (see Cultural Awareness box). In a notable study of hospital nurses caring for Arabic clients, nurses who spoke Arabic rated their clients’ pain similarly to the way clients’ rated their own pain. This was not true of non-Arabic-speaking nurses, whose pain ratings were notably dissimilar to the ratings of their Arabic clients (Harrison, Busebar, & Al-Kaabi, 1996). Pain assessment tools assist health care professionals in objectively and accurately measuring a client’s report of pain and any relief or change in that pain. Pain assessment tools include numeric pain rating scales, such as a 0 to 10 scale where 0 means no pain and 10 means the worst pain; visual analog scales; descriptive pain intensity scales, using descriptions such as “no pain,” “a little pain,” “a lot of pain,” and “too much pain”; pain diaries; and pain logs. Examples of pain assessment tools are illustrated in Fig. 15–2. and is measured by a numeric pain rating scale, such as the 0 to 10 scale. The numeric pain rating scale translates the client’s report of pain into a number that provides the health care professional with an objective description of the client’s pain. This measure of pain can then be used to gauge relief, given the assumption that the number is lower after treatment of the pain. These measures should be recorded in the client’s pain log or chart. A self-care pain management log (Fig. 15–3) is a useful tool. Older adult patients and family members can record pain intensity, pain distress, actions (pharmacologic or nonpharmacologic) taken to relieve the pain, and the outcome of the actions (McCaffery & Pasero, 1999). The self-care pain management log furnishes clients, family members, and clinicians with the information needed to provide effective pain assessment and management. (For another method of recording, see the daily pain diary in Fig. 15–4.) However, researchers have found that the use of self-care pain management logs and diaries may involve an excessive focus on pain, resulting in a negative client response (Kerns & Habib, 2004). Gloth (2000) suggests the following three-pronged assessment guide: 1. Pain history: Focus on concurrent medications, prior adverse drug reactions, concomitant illnesses, and the duration, type, onset, and relieving factors of pain. 2. Physical examination: Recognize that pain in the older patient may present differently than in younger patients (e.g., less pain may indicate more serious problems). 3. Prescribing: Resist prescribing analgesics without a diagnosis; begin with low doses (often less than the minimum recommended dose, especially for the oldest old) and increase while frequently monitoring pain status; continually review medications (including over-the-counter drugs) and decrease or remove medications when indicated; monitor for adverse effects and changes in mental status. When it is used in the posttreatment period, a pain scale that relies on the level of activity rather than a subjective rating of pain alone can provide more specific data that are helpful in assessing the level of pain and the effectiveness of pain interventions (Table 15–2). Using other terms in addition to the word pain has been shown to more accurately reflect how many older persons view their discomfort or pain. TABLE 15–2 From Gloth FM, et al: The Functional Pain Scale (FPS): reliability, validity, and responsiveness in a senior population, J Am Med Dir Assoc 2(3):110–114, 2001.
Pain
Understanding Pain
Definition
Pain Classification
Scope of the Problem of Pain
Consequences of Unrelieved Pain
Epidemiology of Pain
Pathophysiology of Pain in Older Adults
Atypical Acute Pain in Older Adults
Barriers to Effective Pain Management in Older Adults
Undertreating Pain: Abuse
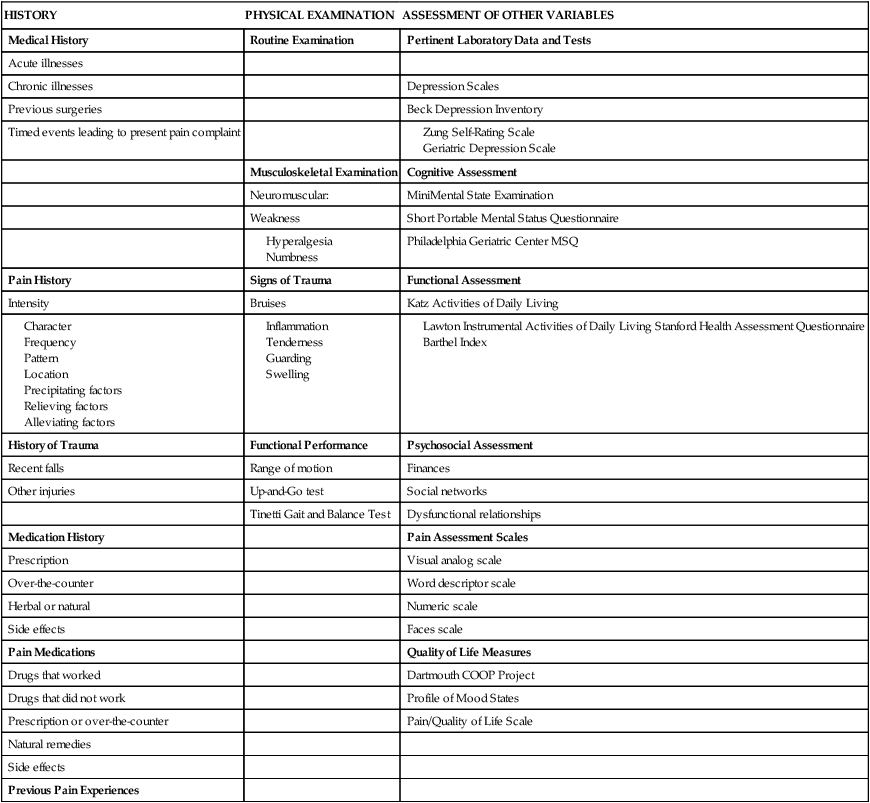
Pain Assessment
HISTORY
PHYSICAL EXAMINATION
ASSESSMENT OF OTHER VARIABLES
Medical History
Routine Examination
Pertinent Laboratory Data and Tests
Acute illnesses
Chronic illnesses
Depression Scales
Previous surgeries
Beck Depression Inventory
Timed events leading to present pain complaint
Musculoskeletal Examination
Cognitive Assessment
Neuromuscular:
MiniMental State Examination
Weakness
Short Portable Mental Status Questionnaire
Philadelphia Geriatric Center MSQ
Pain History
Signs of Trauma
Functional Assessment
Intensity
Bruises
Katz Activities of Daily Living
History of Trauma
Functional Performance
Psychosocial Assessment
Recent falls
Range of motion
Finances
Other injuries
Up-and-Go test
Social networks
Tinetti Gait and Balance Test
Dysfunctional relationships
Medication History
Pain Assessment Scales
Prescription
Visual analog scale
Over-the-counter
Word descriptor scale
Herbal or natural
Numeric scale
Side effects
Faces scale
Pain Medications
Quality of Life Measures
Drugs that worked
Dartmouth COOP Project
Drugs that did not work
Profile of Mood States
Prescription or over-the-counter
Pain/Quality of Life Scale
Natural remedies
Side effects
Previous Pain Experiences
Cultural Pain Assessment
Pain Assessment Tools
SCORE
DESCRIPTION OF PAIN BY PATIENT FUNCTION
0
No pain
1
Tolerable (and does not prevent any activities)
2
Tolerable (but does prevent some activities)
3
Intolerable (but can use telephone, watch TV, or read)
4
Intolerable (cannot use telephone, watch TV, or read)
5
Intolerable (and unable to verbally communicate because of pain)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pain
Get Clinical Tree app for offline access