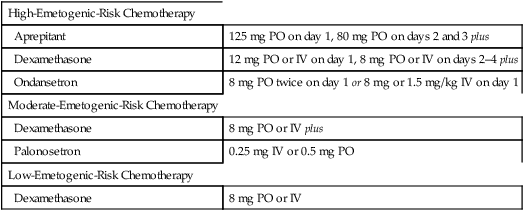
CHAPTER 80 Emesis is a complex reflex brought about by activating the vomiting center, a nucleus of neurons located in the medulla oblongata. Some stimuli activate the vomiting center directly; others act indirectly (Fig. 80–1). Direct-acting stimuli include signals from the cerebral cortex (anticipation or fear), signals from sensory organs (upsetting sights, noxious odors, or pain), and signals from the vestibular apparatus of the inner ear. Indirect-acting stimuli first activate the chemoreceptor trigger zone (CTZ), which in turn activates the vomiting center. Activation of the CTZ occurs in two ways: (1) by signals from the stomach and small intestine (traveling along vagal afferents); and (2) by the direct action of emetogenic compounds (eg, anticancer drugs, opioids, ipecac) that are carried to the CTZ in the blood. Once activated, the vomiting center signals the stomach, diaphragm, and abdominal muscles; the resulting coordinated response expels gastric contents. Several types of antiemetics are available. Their classes, trade names, and dosages are summarized in Table 80–1. Uses and mechanisms are summarized in Table 80–2. Properties of the principal classes are discussed below. TABLE 80–1 Antiemetic Drugs: Classes, Trade Names, and Dosages *Promethazine is contraindicated for children under 2 years of age owing to a risk of fatal respiratory depression. TABLE 80–2 Antiemetic Drugs: Uses and Mechanism of Action Ondansetron [Zofran, Zofran ODT, Zuplenz] was the first serotonin receptor antagonist approved for CINV. The drug is also used to prevent nausea and vomiting associated with radiotherapy and anesthesia. In addition, the drug is used off-label to treat nausea and vomiting from other causes, including childhood viral gastritis and morning sickness of pregnancy. In all cases, benefits derive from blocking type 3 serotonin receptors (5-HT3 receptors*) located in the CTZ and on afferent vagal neurons in the upper GI tract. The drug is very effective by itself, and even more effective when combined with dexamethasone. Administration may be oral or parenteral. The most common side effects are headache, diarrhea, and dizziness. Of much greater concern, ondansetron prolongs the QT interval and hence poses a risk of Torsades de Pointes, a potentially life-threatening dysrhythmia. Accordingly, the drug should not be given to patients with long QT syndrome, and should be used with caution in patients with electrolyte abnormalities, heart failure, or bradydysrhythmias, and in those taking other QT drugs. Since ondansetron does not block dopamine receptors, it does not cause the extrapyramidal effects (eg, akathisia, acute dystonia) seen with antiemetic phenothiazines. As discussed in Chapter 38, ondansetron is under investigation for treating early-onset alcoholism. Two glucocorticoids—methylprednisolone [Solu-Medrol] and dexamethasone—are commonly used to suppress CINV, even though they are not approved by the Food and Drug Administration (FDA) for this application. Glucocorticoids are effective alone and in combination with other antiemetics. The mechanism by which glucocorticoids suppress emesis is unknown. Both dexamethasone and methylprednisolone are administered IV. Because antiemetic use is intermittent and short term, serious side effects are absent. The pharmacology of the glucocorticoids is discussed in Chapter 72. Lorazepam [Ativan] is used in combination regimens to suppress CINV. The drug has three principal benefits: sedation, suppression of anticipatory emesis, and production of anterograde amnesia. In addition, lorazepam may help control extrapyramidal reactions caused by phenothiazine antiemetics. The basic pharmacology of lorazepam and other benzodiazepines is discussed in Chapter 34. The phenothiazines (eg, prochlorperazine) suppress emesis by blocking dopamine2 receptors in the CTZ. These drugs can reduce emesis associated with surgery, cancer chemotherapy, and toxins. Side effects include extrapyramidal reactions, anticholinergic effects, hypotension, and sedation. The basic pharmacology of the phenothiazines is discussed in Chapter 31 (Antipsychotic Agents and Their Use in Schizophrenia). Two butyrophenones—haloperidol [Haldol] and droperidol (formerly available as Inapsine)—are used as antiemetics. Like the phenothiazines, the butyrophenones suppress emesis by blocking dopamine2 receptors in the CTZ. Butyrophenones are effective against postoperative nausea and vomiting, and emesis caused by cancer chemotherapy, radiation therapy, and toxins. Potential side effects are similar to those of the phenothiazines: extrapyramidal reactions, sedation, and hypotension. In addition, droperidol may pose a risk of fatal dysrhythmias owing to prolongation of the QT interval. Accordingly, patients receiving the drug should undergo electrocardiographic monitoring. The pharmacology of the butyrophenones is discussed in Chapter 31. Two cannabinoids—dronabinol [Marinol] and nabilone [Cesamet]*—are approved for medical use in the United States. Both drugs are related to marijuana (Cannabis sativa). Dronabinol (delta-9-tetrahydrocannabinol; THC) is the principal psychoactive agent in C. sativa. Nabilone is a synthetic derivative of dronabinol. A third cannabinoid preparation, sold as Sativex (a combination of THC and cannabidiol), is available in Canada (for treating neuropathic pain) but is illegal in the United States. The basic pharmacology of THC and other cannabinoids is discussed in Chapter 40 (Drug Abuse: Major Drugs of Abuse Other Than Alcohol and Nicotine). The antiemetic regimen for a particular patient is based on the emetogenic potential of the chemotherapy drugs being used. For drugs with a low risk of causing emesis, a single antiemetic (dexamethasone) may be adequate. For drugs with a moderate or high risk of causing emesis, a combination of antiemetics is needed. The current regimen of choice for patients taking highly emetogenic drugs consists of three agents: aprepitant plus dexamethasone plus a 5-HT3 antagonist (eg, ondansetron, palonosetron). Lorazepam may be added to reduce anxiety and anticipatory emesis, and to provide amnesia as well. The superior efficacy of combination therapy suggests that anticancer drugs may induce emesis by multiple mechanisms. Table 80–3 shows representative regimens for preventing CINV in patients receiving anticancer drugs with low, moderate, and high emetogenic risk. TABLE 80–3 Representative Regimens for Preventing Chemotherapy-Induced Nausea and VomitingData from Basch E, Prestrud AA, et al. Antiemetics: American Society of Clinical Oncology. Clinical Practice Guideline Update J. Clin Oncol 29:4189-4198, 2011. Scopolamine, a muscarinic antagonist, is our most effective drug for prevention and treatment of motion sickness. Benefits derive from suppressing nerve traffic in the neuronal pathway that connects the vestibular apparatus of the inner ear to the vomiting center (see Fig. 80–1). The most common side effects are dry mouth, blurred vision, and drowsiness. More severe but less common effects are urinary retention, constipation, and disorientation. The antihistamines used most often for motion sickness are dimenhydrinate, meclizine [Antivert, others], and cyclizine [Marezine]. Because these drugs block receptors for acetylcholine in addition to receptors for histamine, they appear in Table 80–1 as a subclass under Anticholinergics. Suppression of motion sickness appears to result from blocking histaminergic (H1) and muscarinic cholinergic receptors in the neuronal pathway that connects the inner ear to the vomiting center (see Fig. 80–1). The most prominent side effect—sedation—results from blocking H1 receptors. Other side effects—dry mouth, blurred vision, urinary retention, and constipation—result from blocking muscarinic receptors. Antihistamines are less effective than scopolamine for treating motion sickness, and sedation further limits their utility.
Other gastrointestinal drugs
Antiemetics
The emetic response
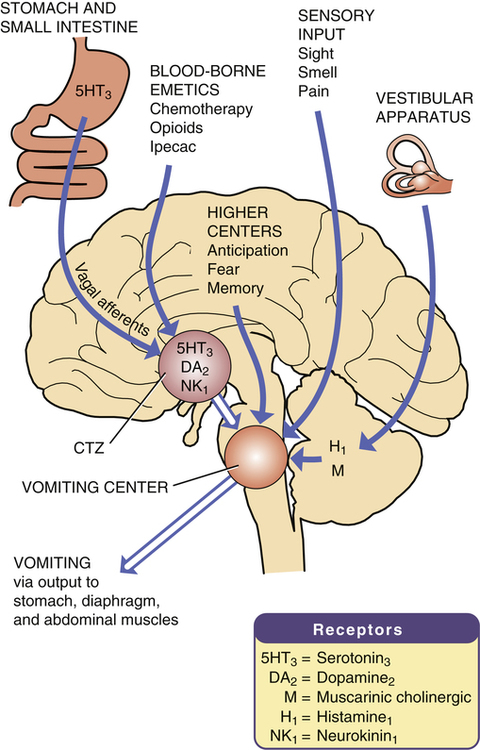
 The emetic response: stimuli, pathways, and receptors.
The emetic response: stimuli, pathways, and receptors.
(CTZ = chemoreceptor trigger zone.)
Antiemetic drugs

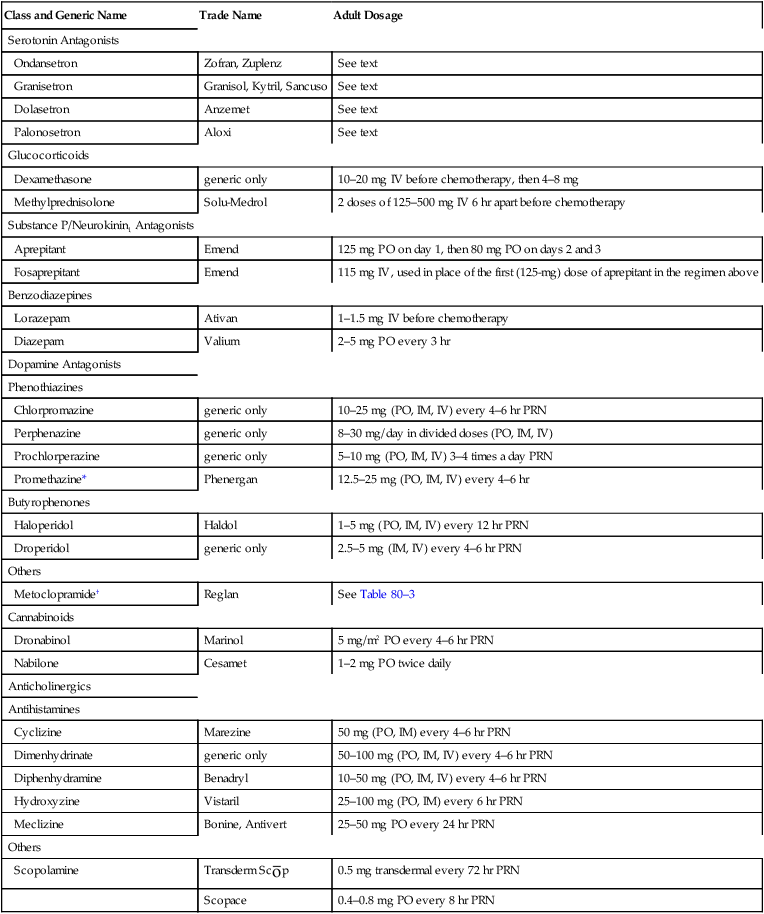
Class and Generic Name
Trade Name
Adult Dosage
Serotonin Antagonists
Ondansetron
Zofran, Zuplenz
See text
Granisetron
Granisol, Kytril, Sancuso
See text
Dolasetron
Anzemet
See text
Palonosetron
Aloxi
See text
Glucocorticoids
Dexamethasone
generic only
10–20 mg IV before chemotherapy, then 4–8 mg
Methylprednisolone
Solu-Medrol
2 doses of 125–500 mg IV 6 hr apart before chemotherapy
Substance P/Neurokinin1 Antagonists
Aprepitant
Emend
125 mg PO on day 1, then 80 mg PO on days 2 and 3
Fosaprepitant
Emend
115 mg IV, used in place of the first (125-mg) dose of aprepitant in the regimen above
Benzodiazepines
Lorazepam
Ativan
1–1.5 mg IV before chemotherapy
Diazepam
Valium
2–5 mg PO every 3 hr
Dopamine Antagonists
Phenothiazines
Chlorpromazine
generic only
10–25 mg (PO, IM, IV) every 4–6 hr PRN
Perphenazine
generic only
8–30 mg/day in divided doses (PO, IM, IV)
Prochlorperazine
generic only
5–10 mg (PO, IM, IV) 3–4 times a day PRN
Promethazine*
Phenergan
12.5–25 mg (PO, IM, IV) every 4–6 hr
Butyrophenones
Haloperidol
Haldol
1–5 mg (PO, IM, IV) every 12 hr PRN
Droperidol
generic only
2.5–5 mg (IM, IV) every 4–6 hr PRN
Others
Metoclopramide†
Reglan
See Table 80–3
Cannabinoids
Dronabinol
Marinol
5 mg/m2 PO every 4–6 hr PRN
Nabilone
Cesamet
1–2 mg PO twice daily
Anticholinergics
Antihistamines
Cyclizine
Marezine
50 mg (PO, IM) every 4–6 hr PRN
Dimenhydrinate
generic only
50–100 mg (PO, IM, IV) every 4–6 hr PRN
Diphenhydramine
Benadryl
10–50 mg (PO, IM, IV) every 4–6 hr PRN
Hydroxyzine
Vistaril
25–100 mg (PO, IM) every 6 hr PRN
Meclizine
Bonine, Antivert
25–50 mg PO every 24 hr PRN
Others
Scopolamine
Transderm Sc ![]() p
p
0.5 mg transdermal every 72 hr PRN
Scopace
0.4–0.8 mg PO every 8 hr PRN

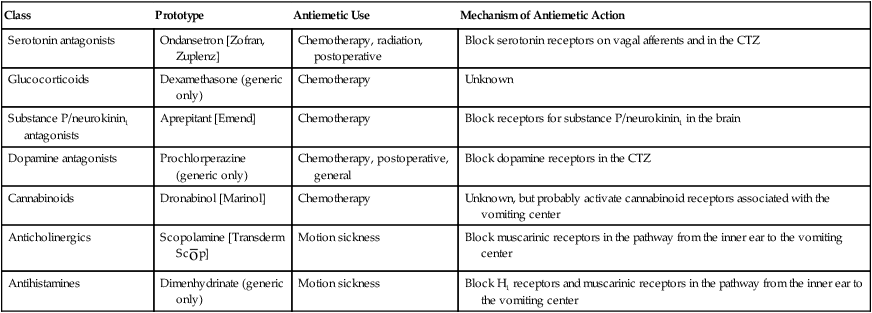
Class
Prototype
Antiemetic Use
Mechanism of Antiemetic Action
Serotonin antagonists
Ondansetron [Zofran, Zuplenz]
Chemotherapy, radiation, postoperative
Block serotonin receptors on vagal afferents and in the CTZ
Glucocorticoids
Dexamethasone (generic only)
Chemotherapy
Unknown
Substance P/neurokinin1 antagonists
Aprepitant [Emend]
Chemotherapy
Block receptors for substance P/neurokinin1 in the brain
Dopamine antagonists
Prochlorperazine (generic only)
Chemotherapy, postoperative, general
Block dopamine receptors in the CTZ
Cannabinoids
Dronabinol [Marinol]
Chemotherapy
Unknown, but probably activate cannabinoid receptors associated with the vomiting center
Anticholinergics
Scopolamine [Transderm Sc ![]() p]
p]
Motion sickness
Block muscarinic receptors in the pathway from the inner ear to the vomiting center
Antihistamines
Dimenhydrinate (generic only)
Motion sickness
Block H1 receptors and muscarinic receptors in the pathway from the inner ear to the vomiting center
Serotonin receptor antagonists
Ondansetron.
Glucocorticoids
Benzodiazepines
Dopamine antagonists
Phenothiazines.
Butyrophenones.
Cannabinoids
Chemotherapy-induced nausea and vomiting

High-Emetogenic-Risk Chemotherapy
Aprepitant
125 mg PO on day 1, 80 mg PO on days 2 and 3 plus
Dexamethasone
12 mg PO or IV on day 1, 8 mg PO or IV on days 2–4 plus
Ondansetron
8 mg PO twice on day 1 or 8 mg or 1.5 mg/kg IV on day 1
Moderate-Emetogenic-Risk Chemotherapy
Dexamethasone
8 mg PO or IV plus
Palonosetron
0.25 mg IV or 0.5 mg PO
Low-Emetogenic-Risk Chemotherapy
Dexamethasone
8 mg PO or IV
Drugs for motion sickness
Scopolamine
Antihistamines
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Other gastrointestinal drugs
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access
