CHAPTER 27 Nursing the patient who experiences trauma
Introduction
Trauma may be defined as ‘blunt or penetrating external force exerted on the body resulting in injury’ (Eckes-Roper 2003: 1). Trauma is not a new disease; however, it continues to be a leading cause of death and disability in all age groups, especially in the first four decades of life (Cole 2008).
Historically people have suffered traumatic injuries caused by modes of transport (the horse and cart for example), assaults, falls and work-related incidents. Conflict also causes death and disability due to traumatic injury. Contemporary trauma care was born out of wartime experience, and lessons learned from the two world wars and the Vietnam War have helped to shape current trauma practice, especially in relation to intravenous fluid therapy and surgical interventions (Cole & McGinley 2005).
Trauma patients are cared for by a variety of practitioners in many clinical settings – from the paramedic at the roadside, to the nurse in a rehabilitation unit; however, trauma is a relatively new specialty in its own right. In the late 1980s The Royal College of Surgeons of England carried out a retrospective review of 1000 trauma deaths in England and Wales (Anderson et al 1988). The report that followed identified that approximately one third of the deaths were preventable and were often due to treatable causes such as hypoxia and haemorrhage, and organisational issues. Following this, the Advanced Trauma Life Support (ATLS) protocols (American College of Surgeons [ACS] 2004) were adopted by many Emergency Departments to guide trauma care and standardise patient management. However, in November 2007 the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) launched Trauma: Who Cares? (Findlay et al 2007). This study has reported that nearly 50% of severely injured patients in the UK did not receive good-quality care. Deficiencies in organisational and clinical aspects of trauma care were identified and NCEPOD has called for significant improvements in pre-hospital and in-hospital trauma care.
Trauma: epidemiology and the need for injury prevention
Traumatic injury can be unintentional or intentional and continues to be a significant health problem. Trauma does not capture the public attention in the same way as other diseases such as cancer, cardiac disease or meningitis; however, traumatic injury is a disease. It has a host (the patient) and a mode of transmission (a vehicle, fire, knife) (ACS 2004) and the statistics are shocking. Trauma affects all age groups and it is the main cause of death in young people, under the age of 40. Annually in the UK, 14 500–18 000 deaths occur as a result of trauma, with 60 000 patients being admitted to hospital each year as a result of a road traffic collision (RTC) (Bonnett et al 2003). In the UK the incidence of severe traumatic injury is estimated at 4 people in every million per week. With approximately 60 million people in the UK, this means 240 severely injured patients per week (Findlay et al 2007).
The irony is that trauma in civilian settings is preventable. There is often a fatalistic ‘accidents will always happen’ attitude towards the cause of injuries; a death following a traumatic event, such as a car accident or a fall at work, is often publicly perceived as an unavoidable fatality (Chiara et al 2006). However, this is incorrect. Traumatic injury should not be thought of as an accident – this word implies a random circumstance, whereas injuries occur in specific, usually preventable patterns. Individuals in high-risk situations or environments, such as children playing near a busy road, adults driving a car at speed or following alcohol consumption, working without protective equipment or carrying a knife provide a chain of events that results in traumatic injury. Legislation such as seat belt laws, environment modifications such as road-calming measures and health promotion campaigns by organisations such as the Royal Society for the Protection of Accidents (RoSPA) have all helped to reduce death and disability, however more needs to be done. Trauma nurses who care for the injured are ideally placed to practise health promotion and injury prevention strategies, either during interactions with patients or by supporting injury prevention strategies such as the Safety and Risk Education Programme (RoSPA 2008).
Mechanism of injury
Following a traumatic event, information about the mechanism of injury may help identify up to 90% of a patient’s injuries (ACS 2004). Mechanism of injury can be classified into four main groups (Greaves et al 2001a):
Blunt trauma causes injury as a result of energy transfer leading to tissue compression and disruption (Eaton 2005). Common injuries include crushing, rupturing or shearing of organs or tissues, fractures (open and closed) and traumatic amputations (Middlehurst 2008). Blast injuries can cause a combination of blunt and penetrating injuries, due to the patient being thrown by the force of the blast, and surrounding objects or people being thrown at the patient.
Penetrating trauma causes injury when an object or missile with a small frontal area and high kinetic energy penetrates the skin and underlying tissues of the body (Eaton 2005). In general, penetrating forces are considered high and medium energy – firearms and fragments from blasts – and low energy such as knives, broken glass and other sharp objects (Middlehurst 2008).
The nurse assessing a trauma patient should consider the mechanism of injury, especially when it is suggestive of a serious, high-energy force. Patients may not appear to have sustained obvious injuries following a traumatic event, especially if the injury is internal. However, a high index of suspicion and careful assessment and reassessment of the patient is essential in every clinical setting to detect deterioration or the onset of complications (Middlehurst 2008).
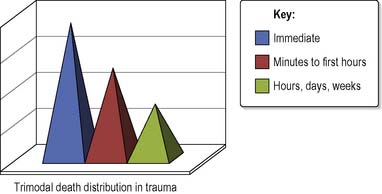
Death following trauma
Death due to traumatic injury occurs in one of three time periods, described as the trimodal death distribution (ACS 2004) (Figure 27.1). This has significance for trauma nurses working throughout all the areas of trauma care.
Disability
It must be remembered that death is not the only outcome following traumatic injury. Worldwide, large numbers of people are left permanently disabled following intentional or unintentional injury, causing a huge financial and social burden on society (WHO 2008). Disabilities following injury include:
Pre-hospital care
Pre-hospital care is defined as the provision of skilled medical help at the scene of an accident, medical or other clinical emergency, and during transport of the patient to hospital (Noble-Mathews 2005). In most UK settings this will involve staff from an ambulance service, using road vehicles or possibly helicopters to assess, resuscitate and then transport trauma patients to hospital. Currently in the UK there are only a few pre-hospital care nurses working in the field of trauma, in comparison to the USA and other European countries.
Advanced notification
Pre-hospital care staff can provide essential information from the scene to the hospital teams waiting to receive the patient in the emergency department (ED). This advanced notification allows the receiving hospital to prepare the necessary equipment and personnel to ensure the best clinical care and outcome (Cole & McGinley 2005). Advanced notification may differ between ambulance services; however, it will generally include the following:
Emergency department
Many Emergency Departments use a system of assessing (or triaging) the patients on arrival to determine the severity of their injury, and then streaming (or directing) them to the appropriate clinical area (Bickerton et al 2005). The ED is usually divided into sections where patients with minor injuries can be seen and treated in a designated area away from those who are more seriously ill or injured. The minor injuries section is where single system traumatic injuries such as ankle or wrist fractures, soft tissue injuries or uncomplicated wounds can be seen and treated.
Once the major trauma patient has arrived at the hospital they should be cared for in a resuscitation area. This is a clinical area which is designed to have the necessary equipment and space readily available to enable a trauma team to care for the patient efficiently and effectively. In the ED it is vital that there is a predetermined system, such as the Advanced Trauma Life Support (ATLS) protocols (ACS 2004), to guide personnel through the initial assessment of the patient. Using a systematic approach (A, B, C, D, E) helps the trauma team to identify life-threatening conditions quickly and to treat them appropriately (Box 27.1).
The trauma team
The trauma team is made up of clinicians (nurses, doctors, radiographers) who carry out pre-assigned roles so that several interventions can occur simultaneously (Cole & Crichton 2006). The aim of the trauma team is to promptly stabilise the patient, identify injuries and initiate a definitive management plan. It has been shown that the most efficient resuscitation will occur if a ‘horizontal organisation’ approach is adopted (Bonnett et al 2003). This is when each member of the team carries out individual tasks simultaneously rather than sequentially (vertical organisation). This reduces the time taken to resuscitate a patient and initiate life-saving procedures, which will improve the patient’s chances of survival. All members of the team should have received training in trauma care to ensure that they have the appropriate level of clinical knowledge and skills.
Trauma teams are usually alerted following the advanced notification information from the pre-hospital care staff. If the mechanism of injury and the status of the patient are suggestive of serious traumatic injury the Royal College of Surgeons/British Orthopaedic Association (2000) suggest that a trauma team should be called for:
Initial assessment and management of the patient: the primary and secondary surveys
Initial assessment and management of the trauma patient is usually performed in two stages: the primary survey and later the secondary survey (ACS 2004, Cole 2008).
The primary survey
The initial assessment (primary survey) has five components – ‘A, B, C, D, E’:
Airway with cervical spine control
The first step of assessment is to find out if the patient has a patent airway (Box 27.2). Following a traumatic event the airway can become obstructed by bleeding in the mouth, swelling of the face, mouth or oropharynx, a reduced level of consciousness or vomiting and aspiration. Expert anaesthetic help should be sought immediately if there is any doubt about the patient’s ability to maintain their own airway.
For any trauma patient it is vital that the cervical spine is protected with in-line immobilisation until a senior clinician can rule out a cervical spine injury. This requires a correctly sized semi-rigid collar to be applied to the neck and manual immobilisation. Alternatively head blocks and tape (attached to an immovable part of the trolley) can be applied to immobilise the head and neck (Figure 27.3).
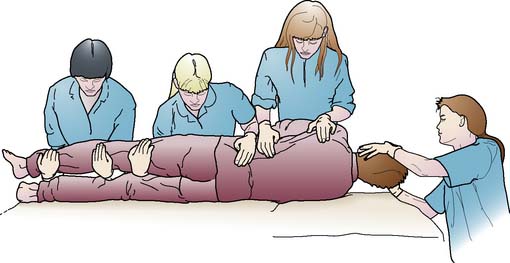
The nurse assisting with maintenance of the patient’s airway must be vigilant in observing the patient for any signs of nausea or vomiting. With the cervical spine immobilised, the patient is unable to move. If vomiting is likely, the team will have to log roll the patient to protect the spine (Figure 27.4) and assist the patient with suction apparatus. In this case, an antiemetic should be prescribed and administered urgently.
Breathing and ventilation
The patient’s respiratory rate must be measured and recorded to observe for the efficacy of ventilation, i.e. effective gaseous exchange taking place at the alveolar capillary membrane. Assessment should include the rate, depth and use of any accessory muscles (see Ch. 3). All patients who have a faster than expected respiratory rate (tachypnoea) should be considered to have had chest injury until proven otherwise. All patients who have sustained traumatic injuries are at risk of hypoxia and should receive a high flow of oxygen. This can be delivered via a mask with a reservoir bag (non-rebreathe mask) with a flow rate of 15 L/min (ACS 2004). By the addition of a reservoir bag the patient will receive up to 90% oxygen concentration compared to only 50% oxygen concentration with an ordinary oxygen mask (Resuscitation Council [UK] 2004). Pulse oximetry assists with monitoring of the patient’s oxygenation saturation of arterial blood. An arterial blood gas sample may be taken if the patient is hypoxic or hypoventilating so that the clinician can gain an accurate picture of the patient’s ventilatory status (Cole 2008).
Major chest injuries can be divided into those that are immediately life threatening and those that are life threatening but are less obvious and often difficult to diagnose. The two groups of injuries have been described as the Lethal six and the Hidden six (Cole 2008) (see Table 27.1). In most cases the life-threatening chest injuries will need a chest drain inserted as part of the initial treatment. The nurse should be familiar with the equipment and assistance needed for chest drain insertion (see Ch. 3).
Table 27.1 Classification of major thoracic injury
| The lethal six | The hidden six |
|---|---|
| Airway obstruction | Traumatic aortic disruption |
| Massive haemothorax | Tracheobronchial tree injury |
| Tension pneumothorax | Oesophageal perforation |
| Open pneumothorax | Cardiac contusion |
| Cardiac tamponade | Pulmonary contusion |
| Flail chest | Diaphragmatic tear or rupture |
Circulation and haemorrhage control
Haemorrhage is the main cause of early trauma deaths (ACS 2004) and can contribute to problems such as clotting disorders or organ failure once the patient has reached definitive care. In severely injured patients hypovolaemia is common and it is the nurse’s role to closely assess and monitor for signs of hypovolaemic shock (see Ch. 18). This includes regular measurement and recording of the patient’s heart rate, blood pressure, capillary refill time and, where possible, urine output (catheterisation may be necessary to monitor this). Table 27.2 summarises the changes to observations in response to haemorrhage.
Table 27.2 Changes in observations in response to haemorrhage
| Pulse rate | Tachycardia due to adrenaline and noradrenaline release (tachycardia is an early sign!) NB: Patients who are on beta blockers or patients who are very athletic will not appear to be tachycardic, although they may be hypovolaemic |
| Respiratory rate | Tachypnoea (increased respiratory rate) due to increased oxygen demand and compensatory mechanisms |
| Level of consciousness | Anxiety or confusion due to the reduction in oxygen delivery to the brain |
| Capillary refill time | Delayed >2 seconds due to systemic vasoconstriction |
| Blood pressure | Normal or raised due to compensation: systemic vasoconstriction (hypotension may be a late sign!) |
| Skin colour | Pale, cool peripheries due to systemic vasoconstriction |
| Urine output | Reduced urine output and increased urine concentration due to antidiuretic hormone and aldosterone production (part of the compensation process) |
It is important to remember that tachycardia is an early sign of haemorrhage, whereas alteration of blood pressure is sometimes a later sign. This is because healthy adults and children may compensate during the initial stages of bleeding, and natural production of adrenaline and noradrenaline help to maintain the blood pressure within normal limits until approximately 30% of blood volume has been lost (Matthews & Bentley 2005). Observing the patient’s skin colour can provide some indication of blood loss and talking to the patient will indicate their current mental status. The greater the blood loss, the paler the patient will look (in all skin colours, however pallor may be easier to detect in the oral mucosa of patients with very dark skin) and as oxygen availability decreases in the blood supply, the patient will become increasingly confused, agitated and eventually unconscious (Bonnett et al 2003).
Common sites of haemorrhage following traumatic injury include the chest, the abdominal contents, the pelvis, the shaft of femurs and external haemorrhage from deep wounds. Internal haemorrhage can be difficult to detect by clinical examination and plain X-ray alone. Increasingly, diagnostic imaging such as ultrasound scans (known as FAST: Focussed Assessment with Sonography in Trauma) and computerised tomography (CT) scans are performed in the ED (or as close as possible) so that the source of bleeding can be found quickly. Trauma patients who are bleeding will need to be seen urgently by a senior surgeon to decide whether surgical or conservative treatment is necessary (Cole 2008).
Fluid resuscitation in early trauma
The injured patient needs two wide-bore cannula inserted into large veins, such as those found in the crease of the elbow joint (antecubital fossa). At this point blood is taken for full blood count, clotting, urea and electrolytes and blood grouping (and if necessary cross matching for a transfusion). Intravenous fluid therapy may be necessary if the patient is hypovolaemic. Isotonic crystalloid fluids are recommended such as 0.9% saline or Hartmann’s solution (ACS 2004). Colloids are not used in the early stages of trauma resuscitation as they have been shown to have a detrimental effect on blood clotting (Brohi et al 2003).
The volume of intravenous fluids required will depend on the cardiovascular status of the patient and the injuries that they have sustained. Traditionally, if a patient is bleeding, intravenous fluids are given to keep their blood pressure at a normal level. However, modern trauma practice suggests that if the patient is given a lot of fluids to maintain the blood pressure then there is a risk of causing clotting problems, hypothermia and further bleeding (Cole 2008). Therefore fluids need to be prescribed and administered following careful consideration of the patient’s haemodynamic status and potential injuries. Once intravenous fluids have been commenced it is vital that cardiovascular observations are recorded every 5 minutes to determine whether the patient is responding. A patient who improves following intravenous fluids may not need urgent surgery, whereas a patient who only improves transiently or not at all is unstable and is likely to require an urgent blood transfusion. If the patient’s own blood group and rhesus match is not available, O Rh-negative blood (the universal donor) will be used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree