CHAPTER 8 Nursing patients with urinary disorders
Introduction
This chapter begins with a brief overview of the anatomy and physiology of the urinary system and of the male reproductive organs. With respect to the latter, this chapter complements the anatomy and physiology described in Chapter 7. Common disorders of the kidneys and the rest of the urinary tract and their treatment and nursing care are then described, including infections, significant renal disorders, obstructive disorders and disorders of the bladder. With regard to the male urinary system and reproductive organs, only prostatic disorders and conditions primarily affecting the urethra are considered here. Conditions more directly affecting reproductive and sexual function, such as erectile dysfunction (ED) and testicular cancer, are discussed in Chapter 7.
Anatomy and physiology
The urinary tract
The kidneys – structure
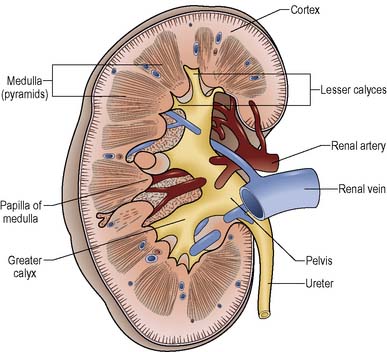
The kidneys are paired organs which lie on the posterior abdominal wall, extending from the twelfth thoracic vertebra to the third lumbar vertebra. Because of the position of the liver, the right kidney is normally slightly lower than the left. Three layers of supportive tissue surround each kidney: an inner fibrous capsule, a middle fatty layer and an outer fascia. This fatty encasement is necessary for maintaining the kidneys in their normal position. Beneath this, a dark outer cortex surrounds a paler medulla, which consists of pale conical striations called the renal pyramids (Figure 8.1).
The nephron
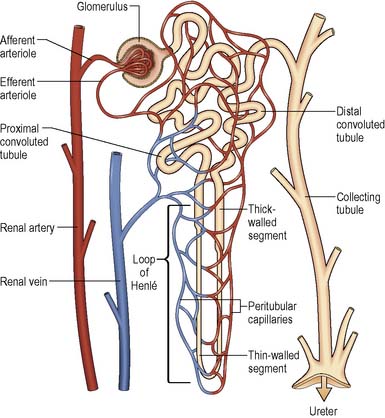
A nephron comprises a convoluted tubular system and a tuft of capillaries known as the glomerulus (Figure 8.2). The glomerulus is enclosed in the cup-shaped upper end of the tubule (glomerular or Bowman’s capsule). The tubule has three sections: the proximal convoluted tubule (PCT), the loop of Henlé, and the distal convoluted tubule (DCT). The DCTs merge to form straight collecting tubules; these ultimately terminate at the renal papillae.
Formation of urine
The first process in the production of urine is filtration. Arterial blood arriving in the wide-bore afferent arteriole enters the glomerulus within the Bowman’s capsule, where substances that are between 3 and 7 nanometres can pass through holes in the capsule endothelium called fenestrations. Note that in health, blood cells and large molecules such as proteins with a molecular weight of 69 000 or above do not pass through the glomerular filtration barrier into the tubule. Once inside the body of Bowman’s capsule, the material that has been filtered, which is called filtrate, enters the first section of the PCT, which is the main site of reabsorption in the nephron. To maintain a flow of blood into the glomerulus, and therefore to maintain filtration, blood must enter at a constant pressure and constant volume. This is achieved by two structures that line the afferent arteriole, the macula densa and the juxtaglomerular apparatus (JGA). When the blood volume and pressure falls, perhaps as a result of blood loss during surgery, the diameter of the arteriole is reduced, thereby maintaining perfusion pressure. This situation cannot last, i.e. the arteriole cannot continue to get smaller because this would limit the kidney’s ability to remove waste products and maintain fluid balance. The constriction of the arteriole is achieved by release of renin. Renin combines with angiotensinogen to form angiotensin I, which is converted by angiotensin-converting enzyme (ACE) into angiotensin II, which is a strong vasoconstrictor. In addition, it stimulates the release of aldosterone (a hormone from the adrenal cortex), which promotes sodium reabsorption, which therefore enhances water reabsorption (see Ch. 20). This, in conjunction with antidiuretic hormone (ADH; also known as arginine vasopressin [AVP] or vasopressin), helps to increase water reabsorption and water intake, and accounts for the fact that urine would normally be expected to be concentrated, i.e. have a specific gravity towards 1.035, in states where fluid loss and dehydration had occurred (see Ch. 20).
![]() See website for further content
See website for further content
See also Thibodeau and Patton (2007) in Further reading.
The functions occurring in the nephron have been summarised in Table 8.1.
Table 8.1 Summary of processes occurring in the nephron
| Location in the Nephron | Processes |
|---|---|
| Proximal convoluted tubule (PCT) | The PCT is the site of most selective reabsorption – the vast majority of filtrate is reabsorbed in the PCT. Specifically specialised cells that line the PCT reabsorb water (H2O), electrolytes including bicarbonate (HCO3–), glucose and other substances, returning them to the circulation via the vasa recta. Substances such as the waste products urea and creatinine are not reabsorbed as they need to be excreted. At the end of the PCT the filtrate contains water, waste and some electrolytes |
| Loop of Henlé | The cells change their structure in the loop of Henlé, allowing selective reabsorption of water and sodium (Na+) |
| Distal tubule (DCT) | Sodium and chloride (Cl–) can be reabsorbed here. The hormone aldosterone facilitates the reabsorption of sodium (and with it water) and chloride, but the hormone ADH is required for any reabsorption of water. The cells of the DCT are also concerned with the reabsorption and/or secretion of hydrogen (H+) and potassium (K+) ions into the filtrate. This last process, known as tubular secretion, is vital in the maintenance of acid–base balance |
| Collecting duct | Once the filtered fluid gets to the collecting ducts only in exceptional circumstances can water and sodium chloride (NaCl) be reabsorbed. ADH is required to make the collecting ducts more permeable to water in order to produce concentrated urine |
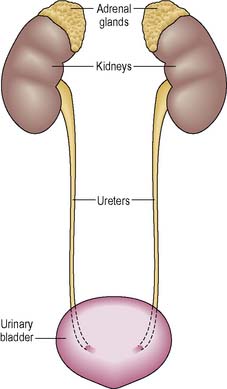
The ureters
Urine is conveyed from the pelvis of each kidney to the bladder via the ureters (Figure 8.3). The ureters are tubular structures approximately 25–30 cm long, ranging in diameter from 2 to 8 mm at various points along their length.
Each ureter is composed of three layers of tissue:
The bladder
The bladder is composed of four layers:
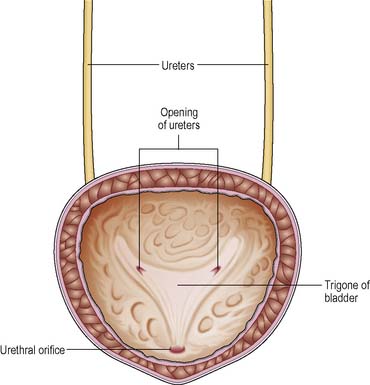
The muscle layer is called the detrusor and is an exceptionally strong muscle that contracts during micturition (passing urine). The interior of the bladder has three orifices, two for the ureters and one for the opening of the urethra. This forms a triangle called the trigone (Figure 8.4).
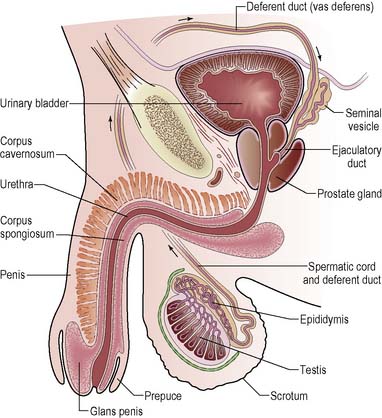
The male reproductive organs
The male reproductive organs are those structures responsible for the production, maturation and delivery into the female reproductive tract of spermatozoa necessary for the fertilisation of secondary oocytes (immature ova). The essential organs of this system are the two testes, in which spermatogenesis (spermatozoa production and maturation) occurs (Figure 8.5). The accessory organs which support the reproductive process include:
The testes
The accessory glands
Disorders of the urinary system
This section covers a range of investigations and disorders of the kidney and other parts of the urinary system. The nursing management is discussed along with an outline of the medical and surgical treatment. Readers who require more detail about treatment are directed to Further reading suggestions, e.g. Colledge et al 2010, Garden et al 2007, Levy et al 2009, and Reynard et al 2008, 2009.
General investigations of the renal and urinary tract
Disorders of the renal and urinary system can be detected using various tests and investigations. Some pathologies, for example, prostate enlargement and prostate cancer, have similar signs and symptoms, and therefore in practice, multiple tests and investigations can be used to aid diagnosis. The common tests and investigations have been divided into those testing urine (Table 8.2), those testing blood (Table 8.3) and those that examine the structure of the urinary tract (Table 8.4). Other investigations used include computed tomography (CT) scan, magnetic resonance imaging (MRI) scan and radionuclide studies.
| Type of Test/Investigation | Indication/Associated Pathology | Significance of Findings |
|---|---|---|
| Urinalysis | All | b. Glycosuria may indicate diabetes mellitus, use of corticosteroids. If positive result, need fasting blood glucose c. Haematuria indicates infection, calculi, renal damage, tumour. A positive result for blood warrants further (specific) investigation d. Proteinuria or albuminuria indicates infection or renal damage; further investigation, e.g. MSU, needed |
| Midstream urine (MSU) or catheter specimen of urine (CSU) | UTI – cystitis, acute pyelonephritis and chronic pyelonephritis (reflux nephropathy) Prostatic enlargement Renal failure | Detects presence of infection; ensure aseptic technique to avoid contaminants and false-positive results. Microbiological examination of the specimen will indicate the presence of and the types of infective organism |
| 24-hour urine analysis e.g. calcium, phosphate, oxalate | Urinary calculi | Measures the substances excreted in the urine in different types of urinary calculi |
| Urine cytology | Bladder cancer | Detects presence of tumour cells. Not diagnostic but used in combination with other tests |
| Urinary flow rate | Prostatic enlargement/cancer | Determines the speed of bladder emptying, volume voided and time taken to empty the bladder. Used to determine the extent of prostate/urethral compression |
| Post-void residual volume | Urinary retention/prostatic enlargement | Determines the volume of urine in the bladder |
| Type of Test/Investigation | Indication/Associated Pathology | Significance of Findings |
|---|---|---|
| Urea and electrolytes (U/Es) | All | Elevations in urea and creatinine indicate decreased renal function |
| Full blood count (FBC) | All | Low haemoglobin may indicate blood loss; anaemia. Increase in white cell count may indicate infection |
| Serum creatinine clearance (used to estimate GFR) | Renal failure and conditions affecting renal function, e.g. diabetic nephropathy | Estimate of renal function. Monitoring patients with reduced renal function |
| Erythrocyte sedimentation rate (ESR) | Nephritis | Non-specific test that detects inflammation/infection Erythrocytes sediment more quickly in individuals in whom disease is present |
| Prostate specific antigen (PSA) (a screening test, also used to monitor response to treatment of prostatic cancer) | Prostatic cancer | PSA result <4 ng/mL is within normal range; PSA result 4–10 ng/mL indicates an intermediate risk of prostate cancer; PSA >10 ng/mL indicates a high risk of prostate cancer |
Table 8.4 Tests of urinary tract structure/function
| Type of test/Investigation | Indication/Associated Pathology | Significance of Findings |
|---|---|---|
| Intravenous urogram/pyelogram (IVU/IVP) | Renal failure, calculi, recurrent UTI, trauma | Indication of structural abnormality or obstruction |
| Urethrogram; endoscopy: urethroscopy, cystoscopy, nephroscopy | Calculi, obstruction | Indication of presence of calculi or mass |
| X-ray or ultrasound (U/S, USS) of kidneys, ureter and bladder (KUB) | Prostate, calculi, UTI | Imaging of renal tract may indicate presence of calculi |
| Biopsy | Kidney, prostate, bladder | Diagnostic for pathology, e.g. cancers, causes of renal failure, types of glomerular disease, etc. Determines the stage of the disease |
Urinary tract infections (UTIs)
Urinary tract infections are defined as an inflammatory response of the urothelium (cells lining the urinary tract) to bacterial invasion that is usually associated with bacteriuria and pyuria (Steggall 2007).
Most bacteria enter the urinary tract through the urethra into the bladder. This is enhanced in individuals with significant soilage of the perineum with faeces and patients with intermittent or indwelling catheters. Depending on the location of the infection, there are further classifications of UTI (Table 8.5).
Table 8.5 Classification of common urinary tract infections by site
| Site | Type of Infection | Causes/Signs |
|---|---|---|
| Kidney | a. Acute pyelonephritis | a. Chills, fever, flank pain; accompanied by bacteriuria and pyuria |
| b. Chronic pyelonephritis (reflux nephropathy) | b. Chronic bacterial infection of the kidney associated with vesicoureteric reflux (VUR) (reflux of infected urine from the bladder into the ureters); causes scarring on the kidney | |
| Bladder | Cystitis | Dysuria (pain on passing urine), frequency, urgency, cloudy urine that may have a strong odour and sometimes haematuria, suprapubic or back pain. There is inflammation of the bladder which can be bacterial or non-bacterial |
| Urethra | Urethritis | As cystitis but it is inflammation of the urethra |
Pyelonephritis
Pyelonephritis, or inflammation of the renal pelvis and renal tissue, may occur in one or both kidneys. Bacteria may enter the urinary tract, especially the kidneys, via the bloodstream or, more commonly, the bladder. Most organisms causing urinary tract infection – E. coli, Klebsiella spp, Proteus, Pseudomonas, E. faecalis and S. epidermidis (S. albus) – are found in the bowel and the perineum. There are two types of pyelonephritis, acute and chronic (often called reflux nephropathy as it can result from vesicoureteric reflux [VUR]), but the presenting features are different (Table 8.5).
Investigations for acute and chronic pyelonephritis (reflux nephropathy)
Box 8.1 Information
Intravenous urogram or pyelogram (IVU/IVP)
The IVU radiograph may demonstrate a variety of pathologies:
Cystitis
Cystitis may be chronic or acute and is characterised by severe inflammation of the bladder walls. More commonly affecting women, cystitis may also result from predisposing factors such as the presence of foreign bodies or stones, obstruction, tuberculosis, carcinoma in situ, chronic urinary infection and schistosomiasis (disease caused by flukes). Features of cystitis include burning on micturition, urinary frequency and urgency, and possibly incontinence. The results of MSU may be needed to treat any infection, although there is no need to wait for the results before commencing antibiotic therapy. Persistent infections warrant further investigations, for example IVU, and may be treated with long-term antibiotic therapy. A key feature in treatment should be increased fluid intake to help flush the urinary system. In addition to increasing fluid intake there is a range of self-help measures available to women who suffer from recurrent cystitis, for example attention to personal hygiene, passing urine frequently during the day and not ‘holding on’, emptying their bladder just before going to bed, cranberry juice, etc. (Boxes 8.2, 8.3). Nurses providing information to patients should be aware that cranberry juice may possibly increase the action of coumarin anticoagulants, e.g. warfarin.
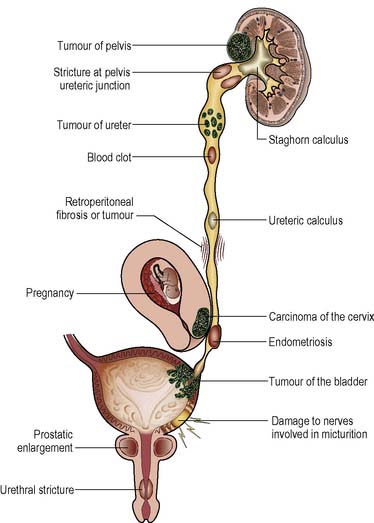
Obstructive disorders of the urinary tract
There are many disorders that cause obstruction to the flow of urine, for example prostate enlargement, calculi or tumours (Figure 8.6). Although the early stages may cause only mild symptoms which are easily ignored, the progressive damage caused by abnormal pressure, infection and stone formation can lead to renal failure. The importance of early detection and intervention cannot be overemphasised.
Urinary stones (renal calculi)
Pathophysiology
Urinary calculi are formed by the aggregation of mineral crystal deposits in the urine (Steggall & O’Mara 2008). The main types of stone are calcium oxalate, although other compositions of stone occur (Steggall & O’Mara 2008). The frequency of different types of stone varies between countries and is probably related to diet, environmental factors and possibly genetic factors (Goddard et al 2006). The risk factors for developing calculi are stasis of urine, chronic urinary infection and excess excretion of stone-forming substances. The most common presenting feature is pain and haematuria, caused by movement of the calculi, although this is not a universal symptom. Stones lodged in the renal pelvis (e.g. ‘staghorn’ calculus) tend to be immobile and so the presenting features are urinary tract infection and pyrexia.
Medical management and treatment
Stones less than 5 mm in diameter may pass unobstructed through the urinary tract and be excreted in the urine. In some cases an alpha-blocker (e.g. tamsulosin) can be used to aid the passing of a stone. Increasing fluid intake to increase fluid output is not recommended in the acute phase of management because it will result in further distension of the urinary system; a normal fluid intake should be encouraged. For further information see Further reading, e.g. Reynard et al 2008, 2009.
Management of acute renal colic
Information about investigations is provided in Tables 8.2, 8.3 and 8.4.
The patient with renal stones may be acutely ill, suffering from excruciating pain arising in the loin and radiating to the groin (and the testis or labium), which can last 5–6 h. Pain is caused by small calculi being moved along the ureter by peristaltic movements, by impaction and by obstruction of urine. Bed rest, warmth to the site of pain (Boon et al 2006) and analgesics are the first line of treatment.
Medications include the opioid morphine intramuscularly. Pethidine should be avoided as it is associated with a higher incidence of vomiting (Holdgate & Pollock 2004). Diclofenac sodium (per rectum, usually at night) is a prostaglandin synthetase inhibitor which reduces renal blood flow and urination. It has an antispasmodic and anti-inflammatory effect and is long acting. Nausea may be relieved by an antiemetic such as i.m. prochlorperazine.
Flush-back of calculi and stenting
(Box 8.4) This procedure affords temporary relief when a calculus causes obstruction and pain in the ureter. The stone is flushed back to the pelvis of the kidney. A small silicone tube called a stent is positioned in the ureter from the pelviureteric junction (PUJ) to the bladder. This stent is left in position to hold the stone in place. Further treatment to remove the stone can now be planned. The stent should not be left for more than 6 weeks. If the planned treatment cannot be carried out by the end of this period, the stent should be changed.
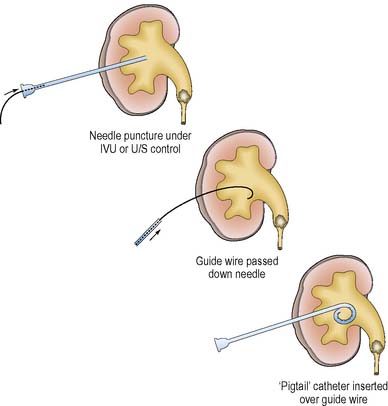
Insertion of a nephrostomy tube
is indicated when obstruction in the kidney or the ureter cannot be relieved by flush-back and stenting (Figure 8.7).This is carried out under X-ray control, usually with a local anaesthetic. A small silicone tube is placed percutaneously into the collecting system of the kidney. The tube is held in place by a suture and connected to a closed-system drainage bag.
Ureteroscopic removal of calculi
Rigid ureteroscopes are now available which can be inserted under direct vision. The surgeon is able to see the stone and can disintegrate it in situ (using mechanical means or laser) before removing the smaller fragments in a ‘basket’ (Underwood et al 2003).
Extracorporeal shock wave lithotripsy (ESWL)
This procedure is the treatment of choice for the majority of patients with calculi, both renal and ureteric (Downey 2000). It effectively treats 70–80% of cases. Large calculi are broken up by means of this technique before percutaneous removal.
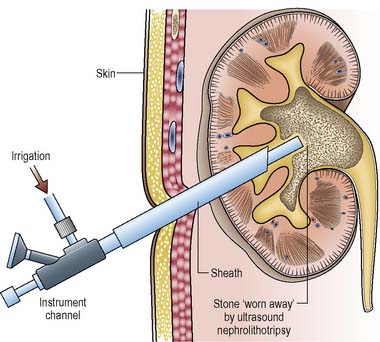
Percutaneous nephrolithotomy (PCNL)
This procedure is used to remove calculi lying within the kidney. Large staghorn calculi may need to be broken up first, using ESWL. PCNL is performed under X-ray and ultrasound control. The patient will normally have a general anaesthetic. The kidney is punctured and the tract into the kidney is dilated to allow the nephroscope and a variety of grasping instruments to be inserted (Figure 8.8). The stone can then be removed or broken down into fine powder by ultrasonic probes. This powder can be aspirated through the centre of the probe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree