CHAPTER 13 Nursing patients with disorders of the eye and vision
Introduction
The aims of this chapter are to present the knowledge and specialised care required for the ophthalmic patient, to raise awareness pertaining to visual impairment (VI) and how VI impacts upon all aspects of daily living, and to consider the implications for practice relating to the Disability Discrimination Act (DDA) in 2005 (http://www.direct.gov.uk). It is estimated that 100 people a day lose their vision, and sight loss is feared more than AIDS, stroke, cancer, heart disease and diabetes (http://www.vision2020uk.org.uk). As life expectancy increases in the UK, there is a higher incidence of cataract, age-related maculopathy and diabetic eye disease and, therefore, it is increasingly important for health care professionals to recognise adverse ocular signs and symptoms and ensure prompt referral for specialised care.
It is predicted that by 2020 many specialised nurses will be retiring (http://www.rcn.org.uk) at a time when a large percentage of the population will be over 60 years of age and by association there will be a higher incidence of VI/eye disease. The need for service modernisation which would improve efficiency and delivery of care (Cuber-Dochan et al 2006) and the reduction in junior doctors’ hours (Calpin-Davies 2001) have served as catalysts for developing the role of the health care professional in this dynamic field of health care. As the professional need and desire to develop ophthalmic knowledge (Marsden & Shaw 2007) continues, the nursing roles are evolving in response to the influence of technological, statutory and organisational change. These roles, which have increased both nursing autonomy and responsibility, include performing minor lid surgery, emergency eye care, glaucoma monitoring and cataract care among a variety of other nurse-led initiatives. The health care professional in all environments has a duty of care to be up-to-date in practice, to facilitate health promotion, screening, primary and secondary care (Nursing and Midwifery Council [NMC] 2008). The ocular conditions and diseases presented in this chapter will provide the reader with a sound knowledge base related to causes, diagnoses, management and related nursing care. Not all ocular conditions cause VI; many clinical conditions are successfully treated with medical and surgical interventions. The main causes of VI in the UK are cataract (p. 431) and glaucoma (p. 432), age-related macular degeneration (p. 443) and diabetic eye disease (p. 444).
The term ‘visually impaired’ will be used throughout this chapter as an alternative term for people who do not wish to be labelled as ‘blind’ or ‘partially sighted’, as they can feel that these terms are negative and misleading (http://www.afbp.org/). It is estimated, globally, that 135 million people are visually impaired (VI) with 80% having eye disease that is believed to be treatable or preventable (http://www.who.int). The risk of blindness in developing countries is 10–14 times higher than in developed countries and it is predicted that the incidence of VI will double by 2020, due to an increase in the population and longer life expectancy (Bunce & Wormald 2006).
The World Health Organization is at the forefront of Vision 2020 – The Right to Sight: A Global Initiative for the Elimination of Avoidable Blindness (http://www.vision2020uk.org.uk). The aim is to eliminate avoidable blindness as a public health problem by the year 2020 (http://www.who.int). The Royal College of Ophthalmologists (http://www.rcopht.ac.uk) estimates that 4.3 million people over 65 years of age in the UK have a VI in one or both eyes (http://www.guidedogs.org.uk).
Anatomy and physiology
The eye
The eyeball
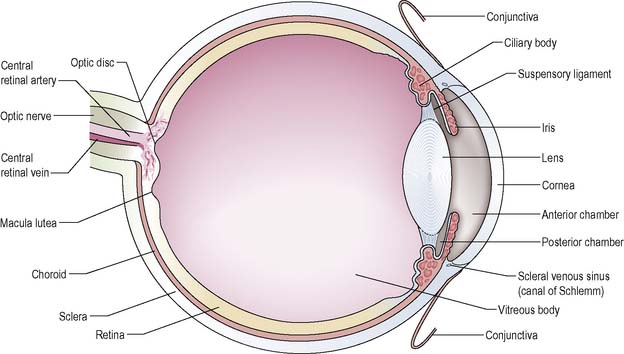
The eyeball or globe is a structure composed of three main layers of tissue (Figure 13.1):
The retina consists of two layers: the pigmented outer layer, which lines the choroid, and the innermost neural layer, which is in contact with the vitreous humor. Rod cells predominate in the periphery and function best in dim light. Cone cells predominate near the centre of the retina and are adapted for bright light and colour vision. These photoreceptor cells are linked through a series of synapses to ganglion cells whose axons run together to form the optic nerve. For further anatomy and physiology see Waugh & Grant (2006) or Field & Tillotson (2008).
The two segments of the eye
Inside the globe, the lens acts to divide the eye into two main segments:
Internal environment and intraocular pressure (IOP)
The anterior compartment is bathed in a clear aqueous fluid (humor) that is produced by the ciliary body and provides nutrients to the lens and cornea. Aqueous flows from the posterior chamber through the pupil to the anterior chamber and drains away through the sieve-like fibrous trabecular meshwork located in the angle between the iris and cornea around the circumference of the eye. This then drains into the vascular canal of Schlemm and into the systemic venous circulation. The production and drainage of aqueous must be constant in order to maintain a normal IOP within the range of 10–20 mmHg (Waugh & Grant 2006).
The depth of the anterior chamber and thus the angle between the cornea and iris, affects the functioning of the drainage system. The larger, elongated eye of the myope (short-sighted person) has a naturally occurring deep anterior chamber with an open angle, whilst the small eye of the hypermetrope (long-sighted person) has a shallow anterior chamber with a narrow angle (Box 13.1). Any interference with normal drainage of the aqueous humor raises the IOP, leading to the decreased blood supply, pain and impaired vision associated with conditions such as glaucoma.
The visual pathways and interpretative centres
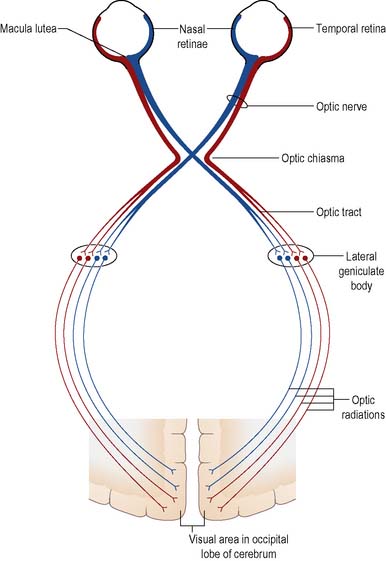
The optic nerve runs from the posterior aspect of the globe and enters the cranial cavity via the optic foramen. The medial nerve fibres cross over to the opposite side at the optic chiasma (Figure 13.2) to join with the lateral fibres and form the optic tract before synapsing in the lateral geniculate body of the thalamus. The fibres then run in the optic radiations to the occipital cerebral cortex of the brain. The main blood supply to the eye is via the ophthalmic artery, a branch of the internal carotid artery.
Accessory structures
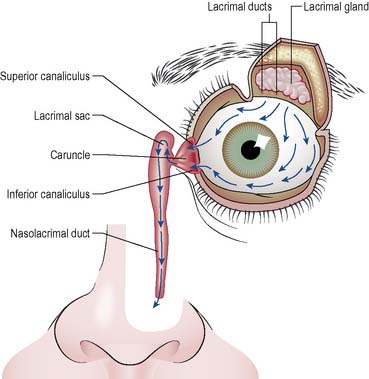
The exposed surface of the eye is covered by a three-layered film of tear fluid. Mucous secretion from conjunctival goblet cells forms the first layer of the tear film and ensures an even spread of tears over the cornea. The middle layer is the watery fluid secreted by the lacrimal glands (situated under the upper orbital rim) and by the accessory glands in the conjunctiva. The outer lipid layer of tear film is secreted by the meibomian glands of the lids. This is thought to reduce the evaporation rate of tears and to prevent the lids sticking together during sleep. The main functions of tear fluid are to lubricate the eye, to facilitate O2 and CO2 exchange, to provide an optically smooth corneal surface and to cleanse the eye with a bacteriostatic enzyme called lysozyme. Excess tears are drained from the eye via the lacrimal punctum and apparatus at the inner canthus (nasal end of the lid margins) into the lacrimal sac and thence into the nose through the nasolacrimal duct (Figure 13.3). Posteriorly and laterally the globe is protected by the bony orbit, the extraocular recti and oblique muscles (responsible for tracking movements) and by orbital fat.
The physiology of vision
Failure to focus may be described as ametropia, or refractive error (see Box 13.1).
Once the rays of light are focused on the retina, their energy is converted into neuroelectrical energy by the photoreceptor cells. These nerve impulses are transmitted via the visual pathway to the visual cortex. Here, they are interpreted as sensations of light, form and colour and are processed into images of objects that are given meaning by other cerebral areas (see Ch. 9).
Assessing the eye and visual function
Examination of structure
It is necessary to know what a normal eye looks like and the normal expectations for an eye recovering from surgery or disease. It is vital for nurses working with ophthalmic patients to examine the eye in a systematic way and to be able to recognise significant abnormalities. It is recommended the nurse works in good light using a well-charged pen torch and examines all ocular structures from outermost to innermost. The possible implications of clinical features that may be found in the course of an eye examination are listed in Table 13.1. For further information on initial visual assessment see Field & Tillotson (2008).
Table 13.1 Significance of clinical features found on eye examination
| Structure | Clinical Features | Possible Significance |
|---|---|---|
| Lids | Bruising (ecchymosis) | Surgical handling |
| Swelling | Trauma | |
| Drooping | Infection | |
| Increased lacrimation | ||
| Discharge | ||
| Conjunctiva | Redness (injection) | Surgical handling |
| Swelling (chemosis) | Trauma | |
| Allergy | ||
| Infection | ||
| Cornea | Cloudy | Increased IOP |
| Crinkled | Infection | |
| Fluorescein staining | Loss of AC | |
| Suture line not intact | Ulceration | |
| Penetrating injury | ||
| Anterior chamber (AC) | Hyphaema (blood in AC) | Hyphaema due to surgery should gradually resolve |
| Increasing IOP = bleeding/inflammation | ||
| Hypopyon (pus in AC) | Hypopyon = infection | |
| Shallow AC | Shallow = ? aqueous loss | |
| Iris | Muddy | Inflammation |
| Pupil | Irregular shape | Iris prolapse |
| Adhesions | ||
| Trauma |
Testing visual function
Visual acuity
Distance vision
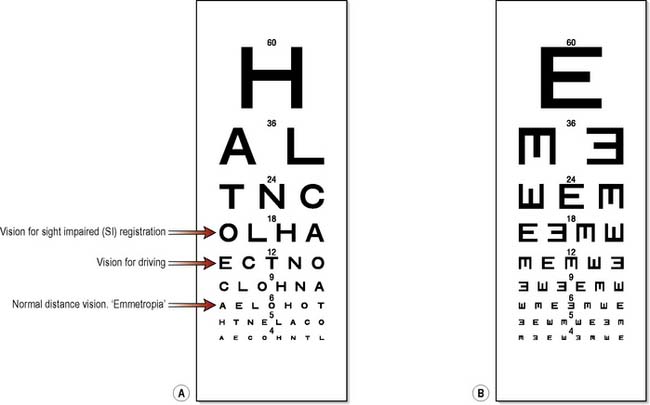
This is tested using Snellen test-type charts, which display letters or pictures arranged in rows of precise and diminishing size (Figure 13.4A). Each eye should be tested separately, with the benefit, if worn, of any spectacles or contact lenses, to ensure that ‘best corrected vision’ is being checked. The eye not being tested must be completely occluded. In normal testing, patients are positioned 6 m away from the chart and asked to read each line aloud until they can no longer make out the letters. The result is recorded as a fraction of the distance from the chart in metres over the normal reading distance of the last complete line read, plus the number of extra letters read from the line below or minus the number of letters read incorrectly, e.g. 6/9 − 2 (Figure 13.4). If glasses or contact lenses are worn this is also recorded.
If the patient cannot read the top letter (6/60) then ability to count fingers (CF) at 1 metre, detect hand movements (HM) or perceive light (PL) is tested. Testing when the patient does not read or understand English can be facilitated by using a Snellen ‘E’ chart (Figure 13.4B). If the patient has learning difficulties, poor concentration or expressive dysphasia then VA testing can be done by using a Sheridan-Gardiner singles booklet in which single letters or pictures of varying size are presented one at a time and the patient is asked match them on a card with a limited choice of symbols. When increased sensitivity of testing is required the LogMAR system may be used at a distance of 4 m. It is conducted in a similar fashion to the Snellen test, but the scoring system for every letter missed is more rigorous (Marsden 2008).
Binocular vision
involves simultaneous perception of an image by both eyes and fusion of the two images in the visual cortex to form a single image. Binocular vision is thought to play a role in depth perception. Having two eyes also widens the field of vision and counters gaps in the visual field caused by natural blind spots (Box 13.2).
The visual field refers to what the eye can see with respect to angle of view (rather than distance). Normally this is about 60 degrees nasally, 90 degrees temporally, 50 degrees superiorly and 70 degrees inferiorly. Assessment of the integrity of the visual field is essential in the management of glaucoma and an important aid to diagnosis of neurological disease and retinal detachment. In the primary care environment and in the absence of automated equipment visual field testing can be carried out by means of a simple confrontation test, whereby the examiner sits directly in front and approximately one metre from the patient and compares the patient’s field of vision with their own (Douglas et al 2005). In the ophthalmic setting it is performed by means of perimetry using field analyser systems to gain accurate measurements of visual field defects known as scotomas (Khaw et al 2004).
Colour-blindness
Colour vision depends on the normal functioning of the retinal cones. A colour-blind person is unable to distinguish between some colours – usually red and green. While approximately 8% of the male population is born with defective colour vision, this problem is estimated at only 1% in females. Colour-blindness can be congenital or acquired through certain conditions such as optic neuritis or drug dependency. For further information on colour vision deficiency see http://www.healthinfoplus.scot.nhs.uk.
Eye changes with ageing
By age 70, most people will need some form of visual aid because the elasticity of the lens decreases with age. Focusing is affected as the cornea flattens, causing astigmatism (see Box 13.1). Retinal cells become less efficient due to deposits laid down by ageing pigment epithelial cells. Tear film is reduced in volume and altered in structure, with the result that tears evaporate more quickly, leading to dryness and irritation of the eye. Conversely, some elderly patients complain of watering eyes due to muscle laxity and malposition of eyelids (see Entropion and Ectropion, p. 444).
Nursing management and health promotion: preservation of vision
Health care professionals can do a great deal through health education and active intervention to help people preserve their vision by observing individual behaviour and general appearance; missed appointments, unkempt clothes and a reluctance to go out may suggest ocular problems (http://www.rnib.org.uk) (Box 13.3). Should any changes be noted, prompt action and referral to an optician to ensure early screening and accurate diagnosis are vital.
The following will contribute to health education and promotion.
Box 13.4 Reflection
Concordance and compliance
If we accept that concordance is not necessarily the same concept as compliance or adherence (consult the Phamaceutical Journal Online – http://www.pharmj.com/ – and type in ‘concordance’ in the search box), how do you as a nurse see your role with a patient who is prescribed topical anti-glaucoma treatment?
The visually impaired person (VIP)
Certification of vision impairment (CVI)
Most visually impaired people have some residual sight and there are few VIPs with a visual acuity of no perception of light (NPL). An ophthalmologist is required to certify the degree of impairment (Table 13.2) and certify that the patient is either Severely Sight Impaired (SSI, previously known as blind) or Sight Impaired (SI, previously known as partially sighted). In England a ‘certificate of vision impairment’ form (http://www.dh.gov.uk) is used and in Scotland it is a ‘blind person’ form. For information regarding registration in Wales and Northern Ireland see http:www.rnib.org.uk.
Table 13.2 Defining visual impairment (adapted from the Royal National Institute of Blind People)
| Type of VI | Definition/ Standards for CVI |
|---|---|
| SSI | VA less than 3/60 with full visual field (VF) VA between 3/60 and 6/60 with reduced VF VA 6/60 or above with reduced VF |
| SI | VA 3/60 to 6/60 with full VF VA up to 6/24 with altered VF VA up to 6/18 with large VF defect |
People with impaired vision may be referred to a low-vision clinic and assessed by an optometrist or specialist nurse to determine the need for low visual aids (LVAs) in the form of a monocular telescope, for reading bus numbers at a distance, or a magnifying glass for near vision tasks such as reading newspapers. Closed circuit television (CCTV) allows the VIP to comfortably view a magnified image of material such as photographs or objects such as pill boxes with added clarity and so can help individuals to make best use of their residual sight. These professionals may also provide information and advice on adaptation or retraining for employment. Employers can also be advised by various agencies, including the Royal National Institute of Blind People (http://www.rnib.org.uk) and Action for Blind People (http://www.afbp.org) about the sophisticated electronic equipment now available for VI employees. The introduction of the Disability Discrimination Act (DDA) in 1995 made it unlawful to treat disabled individuals in a discriminatory way, stating that employers and service providers, including the NHS and Primary Care Trusts (PCTs), must make reasonable adjustments to their services, ensuring for example equal access for disabled persons (http://www.direct.gov.uk).
Considering the needs of the visually impaired person
All client care should be planned using a structured approach to assessment and implemented with an ongoing recognition of the degree of assistance the VIP actually wants. The principles for care listed below echo the tenets of the Roper, Logan and Tierney (1990) model for nursing which is based on activities of living; it is a nursing model in which care is orientated to the patient and provided in a way that enables or supports the patient.
![]() See website Critical thinking question 13.1
See website Critical thinking question 13.1
Some general principles of care for the visually impaired person are outlined below:
Nursing management and health promotion: ophthalmic care
General principles for ophthalmic care
Alleviating stress and giving information
If a local anaesthetic is to be used, the person may be concerned about their level of awareness during the procedure and about whether they will be able to cooperate. Depending on the patient’s visual acuity, it is often helpful to discuss the operation using a model of the eye. Some patients will want only the minimum details and so the nurse should provide the appropriate amount and depth of information for each individual in order that the patient’s wishes are respected. See Chapter 26 for further discussion of the principles of peri-operative nursing, anxiety, informed consent and information giving.
Asepsis and infection control issues
Each eye should be treated separately. Drops and ointments should only be used in the eye for which they are prescribed. In hospital, topical medication should be dated upon opening and discarded after one week (after 4 weeks in the community). These precautions and simple handwashing measures (see Ch. 16) will reduce the risk of eye infection, which can pose a threat to vision.
Instilling eye drops and ointments
If the patient is able to carry out self-medication, instruction in the instillation of drops can provide a good opportunity to begin a teaching programme for postoperative self-care. Eye drops are inserted into the middle to outer third of the lower conjunctival sac. To facilitate this, the patient is asked to tilt the head back and look up while the lower lid is gently pulled down (Figure 13.6). Dropping the solution onto the sensitive cornea will cause discomfort and trigger a reflexive squeezing shut of the eye. After drop instillation the patient is asked to close their eyes gently for 30 s to maximise absorption.
Eye ointment is instilled into the lower conjunctival sac with the patient’s head tilted back as described above. Contact of the tube with the eye should be avoided. For information about topical and systemic drugs and other ophthalmic preparations see http://www.bnf.org/bnf/.
Irrigation
This is a procedure that is generally confined to the emergency or occupation health setting. When irrigating the eye, the warmed solution of sodium chloride 0.9% should be directed across the skin of the lateral cheek so as to prepare the patient for the solution coming into contact with the eye. After this the irrigating motion should be directed away from the nasal side of the sclera. This will wash harmful foreign material away from the lacrimal duct to the side of the cheek, where it can be received in a kidney dish (Box 13.5).
Box 13.5 Information
Irrigation of an eye
Copiously irrigate the affected eye(s), preferably with 1 litre of sodium chloride 0.9% via an i.v. giving set or ideally a Morgan lens (http://www.morganlens.com). Ensure the patient is comfortable, reclining with their head and neck supported. Clothing should be protected by waterproof cape and towels. Ask the patient to hold the receiver dish and to turn their head slightly to the affected side. Instill topical anaesthetic drops, e.g. proxymetacaine 1 to 2 drops. Pull down the lower eyelid and irrigate with a steady flow of fluid, while asking the patient to move their eye around and to evert the upper lid to ensure thorough irrigation. Continue irrigation for at least 15 minutes, re-instilling local anaesthetic drops as required. Remove particles or foreign bodies with moistened cotton bud or forceps. Wait 5 minutes prior to checking pH levels of the tear film, which should be 7.5 or below. Continue irrigation until this neutral pH is indicated when reading the colour reaction of a strip of universal pH paper when it touches the tear film in the lower fornix of the eye (Marsden 2008).