CHAPTER 14 Nursing patients with disorders of the ear, nose and throat
The ear
Anatomy and physiology of the ear
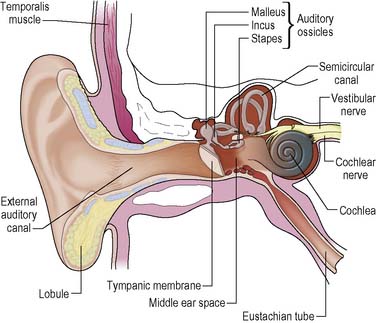
The ear can be divided into three sections: the external ear, the middle ear and the inner ear. The external and middle ears are primarily involved with the transmission of sound. The inner ear contains the organ of hearing as well as structures concerned with body balance (Figure 14.1).
The posterior part of the inner ear is formed by three semicircular canals and by the vestibular apparatus. These assist in the perception of body position against gravity and in the maintenance of balance. The vestibular apparatus consists of the utricle and saccule and is sensitive to linear acceleration. The semicircular canals are sensitive to rotatory acceleration. Balance is maintained by the adjustment of muscles, joints, tendons and ligaments in response to information gathered by the vestibular apparatus and the canals as well as that received by the eyes. For further information, see Tortora (2009).
Disorders of the external ear
Otitis externa
The most common causes of otitis externa, inflammation of the external ear, are infection and allergy. Infection may be caused by excess wax trapping water in the EAM or scratching the ear with contaminated fingernails, cotton buds or other sharp objects. Itching is an early symptom of allergy and is more common in dry skin and dermatological conditions. In otitis externa, multiple bacteriological flora are usually present. The condition most commonly occurs in hot, humid climates, where it tends to be recurrent and may be severe. Patients usually present with a sensation of a blocked ear and a history of localised pain and itching and a burning sensation followed by a discharge, which initially may be watery and then becomes thicker. If there is gross oedema of the meatus and a large amount of debris is present, the patient may suffer from conductive deafness (see p. 452).
Nursing management and health promotion: otitis externa
The first priority of the nursing staff is to clean the EAM so that an examination can be carried out and any prescribed treatment administered effectively. This procedure is called aural toilet and should only be carried out by an appropriately qualified ENT nurse. Cotton wool can be tightly applied to an instrument specifically designed for aural toilet (Figure 14.2). This looks similar to a cotton bud, however the area of cotton is designed to be narrower to ensure the ear canal is not occluded once the cotton-tipped instrument is inserted into the canal. Care must be taken not to damage the skin. Gentle pulling of the pinna will straighten the canal and allow easier access (as demonstrated in Figure 14.3). A good light source should be used or an operating microscope. Gentle irrigation with water can clean the EAM but large amounts of discharge and debris are best removed by an appropriately qualified nurse or doctor using microsuction via a fine-bore tube under an operating microscope in the outpatient department.
It may be necessary to administer an oral analgesic before the external auditory canal can be properly examined, as often any movement of the pinna is painful, see Box 14.1.
Box 14.1 Reflection
Cerumen excess
Cerumen is the normal waxy secretion of special glands in the external auditory canal. Along with shed skin scales and hair, the cerumen normally migrates naturally out of the EAM but can be hindered by coarse hair, narrow canals or by the person impacting the material by attempting to clean the ears with cotton wool buds or other instruments. Nurses should provide patients with health education information regarding the normal cleansing mechanism and avoiding the use of cotton buds and other foreign bodies (Reynolds 2004). The patient usually presents with a blocked feeling in the ear. Tinnitus may develop, causing the patient distress (see p. 458), and disturbance of balance may result from pressure of the hard material on the tympanic membrane.
Medical management
If there is an excessive amount of wax, or the patient needs to have a hearing test or hearing aid review, the doctor, community nurse or outpatient nurse will need to clear the EAM. The wax can be removed manually with instruments, by irrigation with water using an electronic irrigator or by microscope and suction. If the wax is too hard and compacted for this to be carried out, water can be inserted into the EAM for 15 minutes to soften the wax (Roland et al 2008). To improve patient comfort, written information can be given at the time of booking recommending they use olive oil for a few days before the procedure. An advice sheet regarding ear care and how to insert ear drops is available on the website.
![]() See website for further content
See website for further content
Nursing management and health promotion: cerumen excess
![]() See website for further content
See website for further content
Foreign bodies in the ear
Small objects may become lodged in the ear by some mishap or, as frequently occurs among children, by accident during play (Reynolds 2004). Such objects may lie undetected for years unless they have damaged the tympanic membrane. Sometimes gentle irrigation with water or microsuction will remove the foreign body, but if it has become impacted it may be necessary for the patient to be admitted to hospital as a day case and for the object to be removed under general anaesthetic. Only objects that will not expand when in contact with water should be irrigated. Hydroscopic matter such as peas and lentils will absorb the water and become enlarged and often impacted in the canal; as a result removal from the EAM will be through microsuction and/or instrumentation.
Deafness and hearing loss
Although total deafness is comparatively rare, many people suffer hearing loss to varying degrees. Deafness can affect both adults and children. There are 840 babies born each year in the UK with significant deafness. Many children who are deaf continue to be so for all of their lives, but some can be helped to maximise auditory function. This section will concentrate on hearing problems among adults. There are estimated to be 9 million deaf and hard of hearing adults in the UK. This figure is rising as the number of those over 60 increases, with 698 000 of this age group being severely or profoundly deaf (RNID 2008a). A high proportion of severely or profoundly deaf people have other disabilities as well. Among those under 60, 45% have additional disabilities, which are more likely to be physical disabilities. Among severely or profoundly deaf people over 60 years of age, 77% have some additional disability. For 45%, this means significant dexterity or sight difficulties, or both.
Pathophysiology and medical management
Audiometry
Audiometric tests measure hearing acuity. These tests, which include delivering tones of variable frequency and intensity, the spoken word and measuring middle ear pressures, are amongst the methods used to determine the type and source of any hearing loss. Electric response audiometry measures the patient’s response to an acoustic stimulus by way of an electroencephalogram and can provide reliable and exact information on the site of a disorder, e.g. the cochlea, auditory nerve tract or brain stem. Detailed descriptions of these tests can be found in Maltby (2002).
Sensorineural deafness
Presbycusis
the most common type of sensorineural deafness, develops as a consequence of ageing and is becoming increasingly prevalent in Western society. In the UK, 71.1% of people over 70 and 41.7% of people over the age of 50 years will have some kind of hearing loss (RNID 2008a). Audiometry initially shows loss of ability to hear high tones, but there is gradual deterioration of lower tone hearing as well. Degeneration of the nervous tissue leads to loss of intelligibility in the sounds that are heard. Hearing loss in this disorder is symmetrical, i.e. it affects both ears. A hearing aid may be of slight advantage, but distortion and poor discrimination may cancel out any benefit from amplification. When communicating with these patients, it is important to speak a little slower and more distinctly and to try to eliminate any background noise. Because the high tones are affected first, the individual may have trouble hearing consonants, as these are usually of higher tone than vowels. Durga et al (2007) has found that taking a daily folic acid supplement (800 μg) may be helpful in slowing down the progression of presbycusis.
Trauma
Noise-induced hearing loss is well documented and has become recognised as an industrial disease. Socioacusis, the term used to describe the hearing loss caused by sources of noise outside work (loud music, traffic), can be as great a risk as loud noise in the workplace (RNID 2008b). A single exposure to a loud noise such as an explosion or gunshot can cause permanent deafness, or the injury may be temporary. Tinnitus usually accompanies this injury and often takes longer to resolve than any deafness (see p. 458). Exposure to loud noise over a period of time leads to destruction of the hair cells in the organ of Corti. The Noise at Work Regulations (HMSO 1989) laid down strict standards of noise control and protection for employers in the UK, who are liable to be prosecuted if they do not comply (see Useful websites for more information). Occupational health nurses have a role to play in monitoring noise levels and encouraging auditory health through education. On audiometry, early changes in hearing caused by exposure to noise are seen as a dip that gradually deepens and involves adjacent frequencies.
Head injuries
or other trauma resulting in deafness usually involve fractures or penetrating injuries of the temporal bone. Occasionally, concussion (see Ch. 9) can cause deafness due to haemorrhage into the middle ear or cochlea. These injuries are often accompanied by severe vertigo, nausea and vomiting.
Ménière’s disease
Nursing management and health promotion: deafness and hearing loss
![]() See website for further content
See website for further content
Communicating effectively with a hearing-impaired patient is a very important nursing priority (Box 14.2). In the assessment, the nurse should obtain and record information about the patient’s preferred method of communicating, e.g. lip-reading, finger-spelling or sign language. A study by the RNID (2008a) suggested that deaf adults who used sign language were dissatisfied with and disadvantaged in their communication with health care staff, including nurses. According to Ratna (1994), the problems deaf clients bring to counselling include isolation, frustration, discrimination and physical and sexual abuse.
It is now recognised that deafness can have a profound psychological impact and that hearing-impaired individuals may require support to help resolve problems. Many deaf people would prefer to have counselling from a counsellor who is deaf, and attempts should be made to find such a professional if preferred (via the British Association for Counselling and Psychotherapy [BACP] if necessary, see Useful websites). Older adults and their carers have complained of symptoms such as depression, anxiety, decreased social activity and emotional turmoil (Berry et al 2004).
Community nurses can provide tremendous help and support for patients and their relatives when sensorineural deafness is a problem. They should be able to assist their patients to obtain many of the aids available, including a hearing dog for the deaf, which can help to overcome communication difficulties in everyday life. There are many associations, both voluntary and professional, which can provide support and help. The nurse working in the community should be a resource person for patients and guide them to the support that is available (see Useful websites and Box 14.3).
Box 14.3 Evidence-based practice
Are we being heard?
Disorders of the middle ear
Secretory otitis media (glue ear)
Glue ear is the most common cause of hearing impairment and the most common reason for elective surgery in children. Approximately 80% of children will suffer from glue ear before they are 4 years old (Scottish Intercollegiate Guidelines Network [SIGN] 2003). This disorder is known as glue ear because it is characterised by a thick, tenacious fluid that collects in the middle ear. Normally, the mucosal secretions of the middle ear drain down the eustachian tube into the nasopharynx (see Figure 14.1). It is not certain whether the abnormal accumulation of this fluid is caused by the viscosity of the fluid, congestion of the eustachian tubes or obstruction caused by enlarged adenoids or a tumour.
Medical management
Conservative treatment
is to prescribe a decongestant, or antihistamines, to reduce oedema of the nasal mucosa. Mucolytics, which liquefy the mucus, have been shown to have no effect on the condition (SIGN 2003).
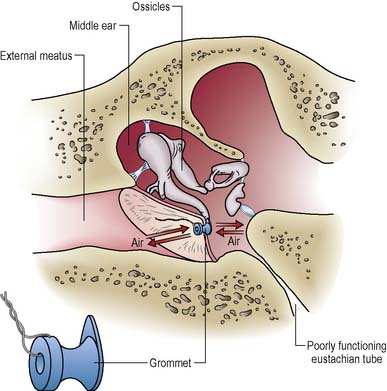
Surgical intervention
involves performing a myringotomy (incising the tympanic membrane) and suctioning of the glue. If a grommet is not inserted, the delicate tympanic membrane heals within a few days. The fluid may, of course, accumulate again. The insertion of a grommet (Figure 14.4) is sometimes considered appropriate, although some specialists think this can lead to scar formation in later years which will impair hearing. If a grommet is inserted, it usually is extruded from the tympanic membrane at 9–12 months; patients sometimes find it on their pillow when they waken one morning. A grommet allows aeration of the middle ear, thus restoring middle ear air pressure. There is usually a marked improvement in hearing after this procedure which is maintained in about 75% of patients.
Nursing management and health promotion: secretory otitis media (glue ear)
Only care specific to ENT patients is outlined in this chapter. The reader is referred to Chapter 26 for details of routine peri-operative care.
Pre-operative care
Most of this surgery is carried out on a day case basis, and the nurse must ensure that the patient and family are adequately informed about what the surgical procedure will entail. This may involve the use of diagrams and it may be helpful to show them a grommet if one is to be inserted. When communicating with the patient pre-operatively, the nurse should make allowances for hearing loss (see Box 14.2).
Otosclerosis
Otosclerosis is a condition in which the ossicles in the middle ear, along with the temporal bone (see Figure 14.1), begin to soften. This spongy bone gradually becomes a dense sclerotic mass; the ossicles may become fixed and less effective in passing on auditory vibrations. The individual with this condition will complain of increasing hearing loss. While this loss is conductive in origin, if the damage extends to the cochlea, sensorineural loss of hearing will also occur. Mild tinnitus (see p. 458) may also be experienced, in which case some people find that they can actually hear better in a noisy environment where their tinnitus is masked.
Acute suppurative otitis media (ASOM)
This is an acute bacterial infection of the middle ear which is especially common in childhood. The most common causative organisms are Streptococcus pneumoniae, Haemophilus influenzae, Streptococcus pyogenes and Staphylococcus aureus. Onset usually follows acute tonsillitis, the common cold or influenza, when infection travels up the eustachian tube to the middle ear. The whole middle ear may be affected, including the mastoid air cells, small air spaces in the posterior portion of the temporal bone, behind the middle ear (see Figure 14.1).
Medical management and treatment
Early stage
The eardrum may appear red with no light being reflected. Analgesics such as paracetamol alternated with ibuprofen will be necessary to relieve pain and reduce fever. Vasoconstricting nasal sprays may also be helpful in keeping the eustachian tubes patent, thereby allowing escape of fluid from the middle ear. In severe cases, admission for intravenous antibiotics and pain control may be necessary (SIGN 2003).
Chronic suppurative otitis media (CSOM)
Medical management
Tympanoplasty
Following removal of diseased tissue, an attempt may be made to re-establish the sound transmission mechanism in the middle ear by reconstructing the tympanic membrane (myringoplasty) using a connective tissue graft taken from the fascia covering the temporal bone and reconstructing the ossicular chain (ossiculoplasty). This combined reconstruction is known as a tympanoplasty. For further information on middle ear surgery see Ludman (2007).
Pre-operative care
The patient is usually admitted on the day of surgery. In view of their obvious hearing deficit, the establishment of good communication is very important. To help avoid complications, the ear must be dry and free from infection. Hearing tests will be carried out to confirm the degree of hearing loss. To help alleviate anxiety, the nurse should give the patient information about the procedure and warn about sensations that may be experienced afterwards, such as dizziness and tinnitus (see p. 458). It is also important to describe the very bulky bandage that will be present around the head and affected ear so that this does not alarm the patient and family. Hearing aids should be worn to the operating theatre. The theatre nurse should remove the hearing aid as the patient is anaesthetised and place it in the patient’s notes. If the hearing aid was worn in the ear that was not operated on, it should be reinserted by the recovery nurse before the patient is extubated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree