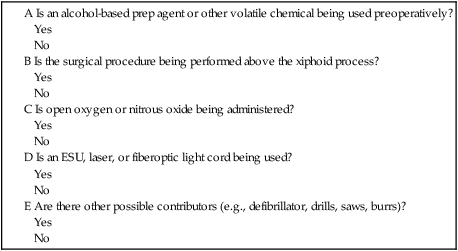
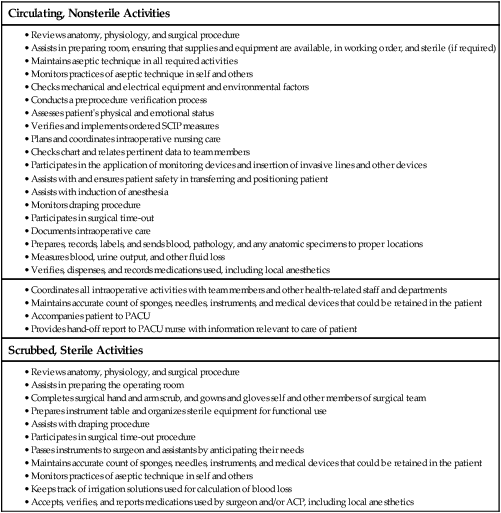
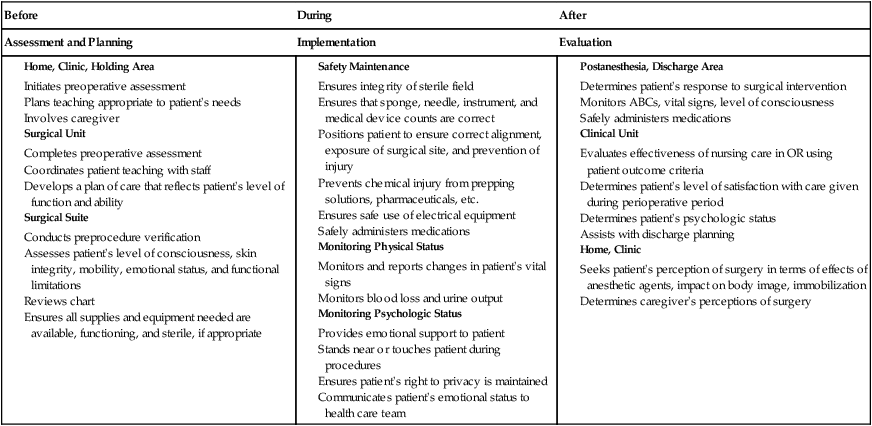
Chapter 19 Anita Jo Shoup and David M. Horner* 1. Differentiate the purposes of the various areas of the perioperative/surgery department and the proper attire for each area. 2. Differentiate the roles and responsibilities of the interdisciplinary surgical team members. 3. Prioritize needs of patients undergoing surgery. 4. Analyze the role of the perioperative nurse in the management of the patient undergoing surgery. 5. Apply basic principles of aseptic technique used in the operating room. 6. Evaluate the importance of safety in the operating room relative to patients, equipment, and anesthesia. 7. Differentiate the common types of and delivery systems for anesthesia. The surgical suite is a controlled environment designed to minimize the spread of pathogens and allow a smooth flow of patients, staff, and equipment needed to provide safe patient care. The suite is divided into three distinct areas: unrestricted, semirestricted, and restricted areas. The unrestricted area is where people in street clothes can interact with those in surgical attire. These areas typically include the points of entry for patients (e.g., holding area), staff (e.g., locker rooms), and information (e.g., nursing station or control desk). The semirestricted area includes the surrounding support areas and corridors. Only authorized staff are allowed access to the semirestricted areas. All staff in the semirestricted area must wear surgical attire and cover all head and facial hair. In the restricted area masks are required to supplement surgical attire.1 The restricted area can include the OR, scrub sink area, and clean core. eTABLE 19-1 In addition, the physical layout is designed to reduce cross-contamination. The flow of clean and sterile supplies and equipment should be separated from contaminated supplies, equipment, and waste by space, time, and traffic patterns. Staff move supplies from clean areas, such as the clean core, through the OR for surgery, and on to the surrounding areas, such as the instrument decontamination area.2 The Surgical Care Improvement Project (SCIP) is a national quality partnership of organizations focused on improving surgical care by significantly reducing the number of complications from surgery3 (refer to www.jointcommission.org/assets/1/6/Surgical%20Care%20Improvement%20Project.pdf). Several SCIP measures may be implemented in the holding area, such as drug administration, patient warming, and application of sequential compression devices (SCDs). Many minor procedures (e.g., inserting IV catheters and arterial lines) can also be performed here. The National Patient Safety Goals (NPSGs) require a preprocedure process, including the verification of relevant documentation (e.g., history and physical examination, signed consent form, nursing and preanesthesia assessment). In addition, any required blood products, implants, devices, and special equipment need to be available. Further, any diagnostic and radiology test results (e.g., x-rays, biopsy reports) need to be properly labeled and displayed.4 In addition, the NPSGs require that the surgeon mark the procedure site. If possible, the marking should be done with the patient’s involvement.4 The traditional surgical environment, or OR, is a unique setting removed from other hospital clinical units. It is controlled geographically, environmentally, and bacteriologically, and it is restricted in terms of the inflow and outflow of staff (Fig. 19-1). It is preferable to have the OR located next to the postanesthesia care unit (PACU) and the surgical intensive care unit. This allows for quick transport of the postoperative patient and close proximity to anesthesia staff if complications arise. Overall safety and comfort are aided by the use of OR furniture that is adjustable, easy to clean, and easy to move. All equipment is checked frequently to ensure proper functioning and electrical safety. The lighting is designed to provide a low- to high-intensity range for a precise view of the surgical site (see Fig. 19-2). A communication system provides a means for the delivery of routine and emergency messages.5,6 In the perioperative role, you assume functions that involve either sterile or unsterile activities (Table 19-1). When you serve in the role of scrub nurse, you follow the designated scrub procedure, are gowned and gloved in sterile attire, and remain in the sterile field (Fig. 19-2). When you serve in the role of circulating nurse, you remain in the unsterile field and so you are not gowned and gloved in sterile attire. TABLE 19-1 INTRAOPERATIVE ACTIVITIES OF PERIOPERATIVE NURSE Ongoing assessment of the patient is essential because the patient’s condition may change quickly. You respond to these changes and revise the plan of care as needed. Examples of nursing activities that characterize each phase surrounding the surgical experience are presented in Table 19-2. TABLE 19-2 NURSING ACTIVITIES DURING SURGICAL EXPERIENCE* ABCs, Airway, breathing, circulation. As patients move through the surgical experience, they are cared for by many team members. Opportunities for error are created whenever clinical information is shared among these members.7 The Joint Commission requires that all health care providers implement a standardized approach to hand-off communication. The perioperative RN ensures that a complete and accurate hand-off using a consistent format, such as SBAR (see Table 1-7), occurs every time the responsibility for patient care is transferred to another professional. Examples of such transfers include change of shift, surgeon to nurse, and OR nurse to postanesthesia nurse. You also have the opportunity to become a certified operating room nurse (CNOR). Certification reflects expertise in surgical nursing. The credential is a personal commitment to higher standards that inspires credibility and confidence with patients and peers in the workplace.8 Depending on your state nurse practice act, the role of the circulating or scrub nurse may be filled by a licensed practical/vocational nurse or a surgical technologist. Surgical technologists may attend an associate degree program, a vocational training program, or a hospital or military training program. The Association of Surgical Technologists is an organization that sets standards for education, provides continuing education opportunities, and offers certification for surgical technologists.9 If the circulating nurse is not an RN, the licensed practical/vocational nurse or surgical technologist must have access to an RN at all times. You are responsible for supervising the licensed practical/vocational nurse or surgical technologist in the performance of all delegated nursing tasks.10 • Preoperative medical history and physical assessment, including need for surgical intervention, choice of surgical procedure, management of preoperative testing, and discussion of the risks of and alternatives to surgical intervention • Patient safety and management in the OR The registered nurse first assistant (RNFA) works in collaboration with the surgeon to produce an optimal surgical outcome for the patient. The Association of periOperative Registered Nurses (AORN) position statement on RNFAs states that the perioperative nurse must have formal education for this role and works collaboratively with the surgeon, patient, and surgical team by handling tissue, using instruments, providing exposure to the surgical site, assisting with hemostasis, and suturing.6,11 RNFA education programs are designed to provide RNs with the education necessary to assume this expanded role.12 The RNFA can also obtain certification. • Medically managing patients who are unconscious or insensible to pain and emotional stress during surgical and other medical procedures • Protecting functions and vital organs under the stress of anesthetic, surgical, or other medical procedures • Managing cardiopulmonary resuscitation • Managing problems in pulmonary care ACPs who are anesthesiologists are responsible for administering anesthetic agents to relieve pain and manage vital life functions (e.g., breathing, blood pressure [BP]) during surgery. After surgery they provide care during recovery.13 A nurse anesthetist is an RN who has graduated from an accredited nurse anesthesia program (minimally a master’s degree program) and successfully completed a national certification examination to become a certified registered nurse anesthetist (CRNA). The CRNA scope of practice includes the following:14 • Performing and documenting a preanesthetic assessment and evaluation • Developing and implementing a plan for delivering anesthesia • Selecting and initiating the planned anesthetic technique • Selecting, obtaining, and administering the anesthesia, adjuvant drugs, and fluids • Selecting, applying, and inserting appropriate noninvasive and invasive monitoring devices • Managing a patient’s airway and pulmonary status • Managing emergence and recovery from anesthesia • Releasing or discharging patients from a PACU • Ordering, initiating, or modifying pain relief therapy • Responding to emergency situations by providing airway management, and administering emergency fluids and drugs • Assuming additional responsibilities within the expertise of the individual The preoperative assessment of the surgical patient establishes baseline data for intraoperative and postoperative care. Preoperative care of the patient is discussed in Chapter 18. Some additional information is discussed in this chapter. Performing a cultural and spiritual assessment can help you understand the patient’s response to the surgical experience (see Tables 2-7 and Table 10-5 for additional information). For example, members of the Jehovah’s Witness community may refuse blood transfusions.15 For Muslims, the left hand is considered unclean, so you should use the right hand to give forms, drugs, and treatments.16 Some Native American patients may request that surgically removed body tissue be preserved so that it may be buried. Some tattoos and body piercings may also have cultural meaning.17 Some patients may have a prayer cloth or other traditional or sacred item with them. Consider spiritual needs and beliefs in the individualized plan of care. For patients who do not speak English, a qualified interpreter must be used (see Table 2-10). Required chart data vary with agency policy, patient condition, and specific surgical procedures. Because ambulatory surgery facilities tend to have a healthier population, fewer tests may be required. Examples of data that are obtained during the preoperative assessment can be found in Tables 18-2 and 18-4. This information contributes to an understanding of past and present history, cardiopulmonary status, and potential for infection and other complications. Complementary and alternative therapies such as therapeutic touch, aromatherapy, music therapy, guided imagery, and even movies may be used for surgical patients. (See the Complementary & Alternative Therapies box above on music and Chapter 6.) These therapies may decrease anxiety, promote relaxation, reduce pain, and accelerate the healing process.6,18 In some facilities these therapies are initiated before the patient’s admission to the OR. In others, such as ambulatory settings, they may be started after the patient’s arrival in the holding area. Before transferring the patient into the OR, prepare the room to ensure privacy, prevention of infection, and safety. Individualization of this preparation is essential to achieve the expected patient outcomes. For example, when an obese patient is admitted to the OR, there are several special considerations (see Chapter 41). Ask such questions as, What equipment is needed to safely transfer the patient to and from the OR table? Will extra staff be required for safe transfer and positioning? Is special equipment needed (e.g., extra-long instrumentation)? What special precautions, if any, must be taken to ensure maintenance of the patient’s airway? The unique needs of each patient must be addressed for a safe surgical experience. Surgical attire (pants and shirts, masks, protective eyewear, and caps or hoods) is worn by all people entering the OR (Fig. 19-3). All electrical and mechanical equipment is checked for proper functioning. Aseptic technique is practiced as each surgical item is opened and placed on the instrument table.19 Sponges, needles, instruments, and small medical devices (e.g., surgical clip cartridges, universal adapters) are counted according to strict processes to ensure accurate retrieval at the end of the procedure. Any retained surgical supplies, devices, or instruments are sentinel events that can result in negative outcomes for the patient.20,21 Surgical hand antisepsis is required of all sterile members of the surgical team (scrub nurse, surgeon, and assistant). When the procedure of scrubbing is the chosen method for surgical hand antisepsis (often for the first case of the day), your fingers and hands should be scrubbed first with progression to the forearms and elbows. The hands should be held away from surgical attire and higher than the elbows at all times to prevent contamination from clothing or detergent suds and water from draining from the unclean area above the elbows to the clean and previously scrubbed areas of the hands and fingers.6,22 Waterless, alcohol-based agents are replacing traditional soap and water in many facilities. When using an alcohol-based surgical hand-scrub product, prewash hands and forearms with soap and dry completely before applying the alcohol-based product. After application of the alcohol-based product, allow hands and forearms to dry thoroughly before donning sterile gloves.22,23 Once surgical hand antisepsis is completed, the team members enter the OR to put on surgical gowns and two pairs of gloves to protect patients and themselves from the transmission of microorganisms.24,25 Because the gowns and gloves are sterile, those who have scrubbed can manipulate and organize all sterile items for use during the procedure.
Nursing Management
Intraoperative Care
Physical Environment of Operating Room
Department Layout
Holding Area
Operating Room

Surgical Team
Registered Nurse
Licensed Practical/Vocational Nurse and Surgical Technologist
Surgeon and Assistant
Registered Nurse First Assistant
Anesthesia Care Provider
Nursing Management Patient before Surgery
Psychosocial Assessment
Chart Review
Admitting the Patient
Nursing Management Patient During Surgery
Room Preparation
Scrubbing, Gowning, and Gloving
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access


