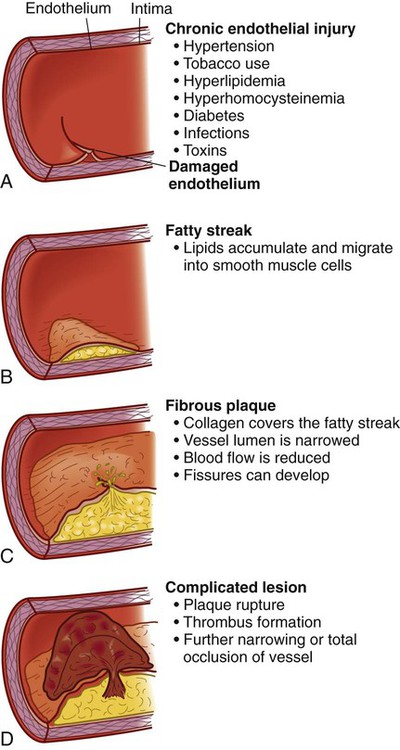
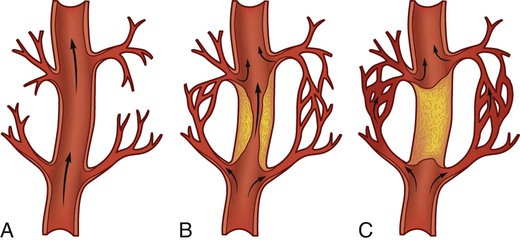
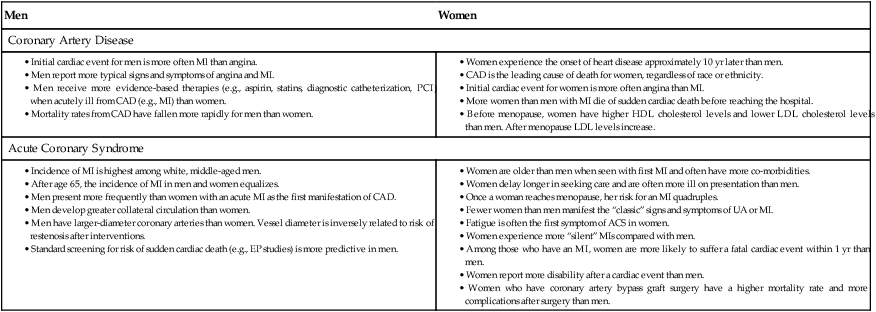
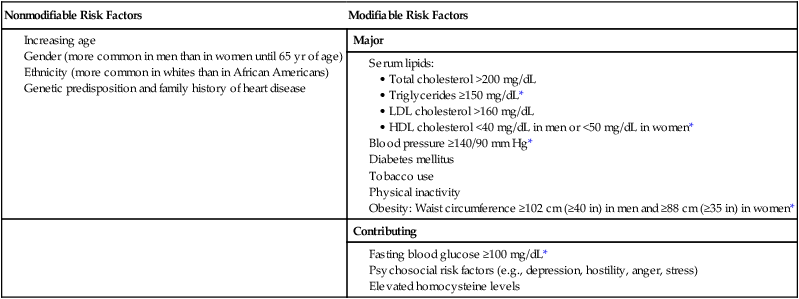
Linda Bucher and Sharmila Johnson 1. Relate the etiology and pathophysiology of coronary artery disease (CAD), angina, and acute coronary syndrome (ACS) to the clinical manifestations of each disorder. 2. Describe the nursing role in the promotion of therapeutic lifestyle changes in patients at risk for CAD. 3. Differentiate the precipitating factors, clinical manifestations, collaborative care, and nursing management of the patient with CAD and chronic stable angina. 4. Explain the clinical manifestations, complications, diagnostic study results, and collaborative care of the patient with ACS. 5. Evaluate commonly used drug therapy in treating patients with CAD and ACS. 6. Prioritize key components to include in the rehabilitation of patients recovering from ACS and coronary revascularization procedures. 7. Differentiate the precipitating factors, clinical presentation, and collaborative care of patients who are at risk for or have experienced sudden cardiac death. eTABLE 34-1 GENES KNOWN TO CONTRIBUTE TO CORONARY ARTERY DISEASE RISK From: Jorde LB, Carey JC, Bamshad MJ: Medical genetics, ed 4, Philadelphia, 2010, Mosby. Cardiovascular disease is the major cause of death in the United States. (The leading causes of death are shown in eFig. 34-1, available on the website for this chapter.) Coronary artery disease (CAD) is the most common type of cardiovascular disease and accounts for the majority of these deaths.1 Patients with CAD can be asymptomatic or develop chronic stable angina (or chest pain). Unstable angina (UA) and myocardial infarction (MI) are more serious manifestations of CAD and are termed acute coronary syndrome (ACS). The American Heart Association (AHA) estimates that 1.1 million Americans have an MI each year. About one fourth of these persons die in an emergency department (ED) or before reaching a hospital. Although the mortality rate from MI has decreased because of advances in treatment, it remains the leading cause of death from all cardiovascular diseases and other conditions in general.1 The endothelium (the inner lining of the vessel wall) is normally nonreactive to platelets and leukocytes, as well as coagulation, fibrinolytic, and complement factors. However, the endothelial lining can be injured as a result of tobacco use, hyperlipidemia, hypertension, toxins, diabetes, hyperhomocysteinemia, and infection causing a local inflammatory response2 (Fig. 34-1, A). C-reactive protein (CRP), a protein produced by the liver, is a nonspecific marker of inflammation. It is increased in many patients with CAD3 (see Table 32-6). The level of CRP rises when there is systemic inflammation. Chronic elevations of CRP are associated with unstable plaques and the oxidation of low-density lipoprotein (LDL) cholesterol. Fatty streaks, the earliest lesions of atherosclerosis, are characterized by lipid-filled smooth muscle cells. As streaks of fat develop within the smooth muscle cells, a yellow tinge appears.2 Fatty streaks can be seen in the coronary arteries by age 15 and involve an increasing amount of surface area as one ages. Treatment that lowers LDL cholesterol may reverse this process (Fig. 34-1, B). Normally the endothelium repairs itself immediately. This does not happen in the individual with CAD. LDLs and growth factors from platelets stimulate smooth muscle proliferation and thickening of the arterial wall. Once endothelial injury has taken place, lipoproteins (carrier proteins within the bloodstream) transport cholesterol and other lipids into the arterial intima. Collagen covers the fatty streak and forms a fibrous plaque with a grayish or whitish appearance. These plaques can form on one portion of the artery or in a circular fashion involving the entire lumen. The borders can be smooth or irregular with rough, jagged edges. The result is a narrowing of the vessel lumen and a reduction in blood flow to the distal tissues (Fig. 34-1, C). The final stage in the development of the atherosclerotic lesion is the most dangerous. As the fibrous plaque grows, continued inflammation can result in plaque instability, ulceration, and rupture. Once the integrity of the artery’s inner wall is compromised, platelets accumulate in large numbers, leading to a thrombus. The thrombus may adhere to the wall of the artery, leading to further narrowing or total occlusion of the artery. Activation of the exposed platelets causes expression of glycoprotein Ilb/IIIa receptors that bind fibrinogen. This, in turn, leads to further platelet aggregation and adhesion, further enlarging the thrombus. At this stage the plaque is referred to as a complicated lesion (Fig. 34-1, D). Normally some arterial anastomoses or connections, termed collateral circulation, exist within the coronary circulation. Two factors contribute to the growth and extent of collateral circulation: (1) the inherited predisposition to develop new blood vessels (angiogenesis) and (2) the presence of chronic ischemia. When a plaque occludes the normal flow of blood through a coronary artery and the resulting ischemia is chronic, increased collateral circulation develops (Fig. 34-2). When occlusion of the coronary arteries occurs slowly over a long period, there is a greater chance of adequate collateral circulation developing, and the myocardium may still receive an adequate amount of blood and oxygen. Risk factors are characteristics or conditions that are associated with a high incidence of a disease. Many risk factors have been associated with CAD. They are categorized as nonmodifiable and modifiable (Table 34-1). Nonmodifiable risk factors are age, gender, ethnicity, family history, and genetics. Modifiable risk factors include elevated serum lipids, elevated blood pressure, tobacco use, physical inactivity, obesity, diabetes, metabolic syndrome, psychologic states, and elevated homocysteine level. TABLE 34-1 RISK FACTORS FOR CORONARY ARTERY DISEASE *Three or more of these risk factors meet the criteria for metabolic syndrome (as defined by the National Cholesterol Education Program Adult Treatment Panel III). Metabolic syndrome is discussed in Chapter 49. Data on risk factors for CAD come from several major studies. In the Framingham study (one of the most widely known), men and women were observed for 20 years. Over time, it was noted that elevated serum cholesterol (greater than 240 mg/dL), elevated systolic blood pressure (BP) (greater than 160 mm Hg), and tobacco use (one or more packs a day) were positively correlated with an increased incidence of CAD.1 The incidence of CAD and MI is highest among white, middle-aged men. After age 65, the incidence in men and women equalizes, although cardiovascular disease causes more deaths in women than men. Additionally, CAD is present in African American women at rates higher than those of their white counterparts.1 (See Cultural & Ethnic Health Disparities box for additional differences in CAD among ethnic groups.) Heart disease kills almost 10 times more women than breast cancer and is the leading cause of death in women. Yet most women do not consider CAD their greatest health risk.4 (Cardiovascular disease mortality trends for both men and women are shown in eFig. 34-2, available on the website for this chapter.) On average, women with CAD are older than men who have CAD, and women are more likely to have co-morbidities (e.g., hypertension, diabetes). Most women have atypical symptoms of angina rather than MI when they experience their first cardiac event4 (see Gender Differences box). The genetic basis of CAD/MI is complex and, to date, poorly understood. It is estimated that the genetic contribution to CAD/MI is as high as 40% to 60%. This proportion relates mainly to genes that control known risk factors (e.g., lipid metabolism).5 (Genes known to contribute to CAD risk are listed in eTable 34-1, available on the website for this chapter.) See the Genetics in Clinical Practice box at right. An elevated serum lipid level is one of the four most firmly established risk factors for CAD.6 The risk of CAD is associated with a serum cholesterol level greater than 200 mg/dL (5.2 mmol/L) or a fasting triglyceride level greater than 150 mg/dL (3.7 mmol/L). (See Table 32-6 for normal serum lipid values.) LDLs contain more cholesterol than any of the lipoproteins and have an attraction for arterial walls. VLDLs contain both cholesterol and triglycerides, and may deposit cholesterol directly on the walls of arteries. Elevated LDL levels correlate closely with an increased incidence of atherosclerosis and CAD. Therefore low serum LDL levels are desirable.6,7 Guidelines for treating elevated LDL cholesterol are based on a person’s 10-year risk for having a nonfatal MI or dying from a coronary event and his or her LDL levels. The following information generates a risk score: (1) age, (2) gender, (3) use of tobacco, (4) systolic BP, (5) use of BP medications, (6) total cholesterol, and (7) HDL cholesterol level.7 A 10-year risk calculator is available at http://hin.nhlbi.nih.gov/atpiii/calculator.asp?usertype=prof. In general, individuals with no or only one risk factor are considered at low risk for the development of CAD, and the LDL goal is less than 160 mg/dL (4.14 mmol/L). Those at very high risk have CAD and multiple risk factors. The LDL goal for this group is less than 70 mg/dL (1.8 mmol/L).7 The second major risk factor in CAD is hypertension, which is defined as a BP greater than 140/90 mm Hg or greater than 130/80 mm Hg if the patient has diabetes or chronic kidney disease.8 Hypertension increases the risk of death from CAD 10-fold in all people. In postmenopausal women, hypertension is associated with a higher incidence of CAD than in men and premenopausal women. Blood pressure is classified as (1) normal (BP less than 120/80 mm Hg), (2) prehypertension (BP of 120 to 139/80 to 89 mm Hg), (3) stage 1 hypertension (140 to 159/90 to 99 mm Hg), and (4) stage 2 hypertension (BP greater than 160/100 mm Hg).8 The cause of hypertension in 90% of those affected is unknown, but it is usually controllable with diet and/or drugs. Therapeutic lifestyle changes should begin in people with prehypertension. Those with stage 1 or 2 hypertension often require more than one drug to reach therapeutic goals8 (see Table 33-7). Teach all people with elevated systolic or diastolic BP the importance of achieving and maintaining target BP goals. The stress of an elevated BP increases the rate of atherosclerotic development. This relates to the shearing stress that causes endothelial injury. Atherosclerosis, in turn, causes narrowed, thickened arterial walls and decreases the distensibility and elasticity of vessels. More force is required to pump blood through diseased arteries, and this increased force is reflected in a higher BP. This increased workload results in left ventricular hypertrophy and decreased stroke volume with each contraction. Salt intake positively correlates with elevated BP, adding volume and increasing systemic vascular resistance (SVR) to the cardiac workload. (See Chapter 33 for a complete discussion of hypertension.) Nicotine in tobacco smoke causes catecholamine (i.e., epinephrine, norepinephrine) release. These neurohormones cause an increased heart rate (HR), peripheral vasoconstriction, and increased BP. These changes increase the cardiac workload. Tobacco smoke is also related to an increase in LDL level, a decrease in HDL level, and release of toxic oxygen radicals. All of these add to vessel inflammation and thrombosis.2 The benefits of smoking cessation are dramatic and almost immediate. CAD mortality rates drop to those of nonsmokers within 12 months. However, nicotine is highly addictive, and often intensive intervention is required to assist people to quit. Individual and group counseling sessions, nicotine replacement therapy, smoking cessation medications (e.g., bupropion [Zyban], varenicline [Chantix]), and hypnosis are examples of smoking cessation strategies. (See Chapter 11, Tables 11-4 through 11-6 for information on smoking cessation.) Chronic exposure to environmental tobacco (secondhand) smoke also increases the risk of CAD.6 People who live in the same household as the patient should be encouraged to stop smoking. This reinforces the individual’s effort and decreases the risk of ongoing exposure to environmental smoke. Pipe and cigar smokers, who often do not inhale, have an increased risk of CAD similar to those exposed to environmental tobacco smoke. Physical inactivity is the fourth major modifiable risk factor. Physical inactivity implies a lack of adequate physical exercise on a regular basis. An example of health-promoting regular physical activity is brisk walking (3 to 4 miles per hour) for at least 30 minutes five or more times a week.9 The mortality rate from CAD is statistically higher in obese persons. Obesity is defined as a body mass index (BMI) of greater than 30 kg/m2 and a waist circumference more than 40 inches for men and more than 35 inches for women. BMI is a measure of body fat based on height and weight. It can be calculated online (http://nhlbisupport.com/bmi/bmicalc.htm). The increased risk for CAD is proportional to the degree of obesity. Obese persons may produce increased levels of LDLs and triglycerides, which are strongly related to atherosclerosis. Obesity is often associated with hypertension. There is also evidence that people who tend to store fat in the abdomen (an “apple” figure) rather than in the hips and buttocks (a “pear” figure) have a higher incidence of CAD (see Table 41-2). As obesity increases, the heart grows and uses more oxygen. In addition, there is an increase in insulin resistance in obese individuals.2 The incidence of CAD is two to four times greater among persons who have diabetes, even those with well-controlled blood glucose levels, than the general population. The patient with diabetes manifests CAD not only more frequently but also at an earlier age.2 There is no age difference between male or female patients with diabetes in the onset of symptoms of CAD. Diabetes virtually eliminates the lower incidence of CAD in premenopausal women. Undiagnosed diabetes is frequently discovered at the time a person has an MI. The person with diabetes has an increased tendency toward endothelial dysfunction. This may account for the development of fatty streaks in these patients. Diabetic patients also have alterations in lipid metabolism and tend to have high cholesterol and triglyceride levels. Management of diabetes should include lifestyle changes and drug therapy to achieve a glycosylated hemoglobin (A1C or Hb A1C) level of less than 7%.6 Metabolic syndrome refers to a cluster of risk factors for CAD whose underlying pathophysiology may be related to insulin resistance. These risk factors include obesity as defined by increased waist circumference, hypertension, abnormal serum lipids, and an elevated fasting blood glucose2 (see Table 41-10). These interrelated risk factors of metabolic origin appear to promote the development of CAD. (Chapter 41 discusses metabolic syndrome.) Studies now are focusing on specific psychologic risk factors thought to increase risk of CAD. These include depression, acute and chronic stress (e.g., poverty, serving as a caregiver), anxiety, hostility and anger, and lack of social support.10,11 In particular, depression is a risk factor for both the development and worsening of CAD. Depressed patients have elevated levels of circulating catecholamines that may contribute to endothelial injury and inflammation and platelet activation. Higher levels of depression are also associated with an increased number of adverse cardiac events.10 More research on the treatment of depression and other negative psychologic states (e.g., anger) in patients with or at risk for CAD is needed to improve these patients’ emotional and physical health. Stressful states correlate with the development of CAD.12 Sympathetic nervous system (SNS) stimulation and its effect on the heart are the physiologic mechanism by which stress predisposes one to the development of CAD. SNS stimulation causes an increased release of catecholamines (i.e., epinephrine, norepinephrine). This stimulation increases HR and intensifies the force of myocardial contraction, resulting in increased myocardial oxygen demand. Also, stress-induced mechanisms can cause elevated lipid and glucose levels and changes in blood coagulation, which can lead to increased atherogenesis.
Nursing Management
Coronary Artery Disease and Acute Coronary Syndrome
Gene
Chromosome Location
Function of Protein Product
Apolipoprotein A-I
11q
HDL component. LCAT cofactor
Apolipoprotein A-IV
11q
Component of chylomicrons and HDL. May influence HDL metabolism
Apolipoprotein C-III
11q
Allelic variation associated with hypertriglyceridemia
Apolipoprotein B
2p
Ligand for LDL receptor. Involved in formation of VLDL, LDL, IDL, and chylomicrons
Apolipoprotein D
2p
HDL component
Apolipoprotein C-I
19q
LCAT activation
Apolipoprotein C-II
19q
Lipoprotein lipase activation
Apolipoprotein E
19q
Ligand for LDL receptor
Apolipoprotein A-II
1p
HDL component
LDL receptor
19p
Uptake of circulating LDL particles
Lipoprotein(a)
6q
Cholesterol transport
Lipoprotein lipase
8p
Hydrolysis of lipoprotein lipids
Hepatic triglyceride lipase
15q
Hydrolysis of lipoprotein lipids
LCAT
16q
Cholesterol esterification
Cholesterol ester transfer protein
16q
Facilitates transfer of cholesterol esters and phospholipids between lipoproteins
Coronary Artery Disease
Etiology and Pathophysiology
Developmental Stages.
Fatty Streak.
Fibrous Plaque.
Complicated Lesion.
Collateral Circulation.
Risk Factors for Coronary Artery Disease
Nonmodifiable Risk Factors
Modifiable Risk Factors
Major
Contributing
Nonmodifiable Risk Factors
Age, Gender, and Ethnicity.
![]() Genetic Link
Genetic Link
Major Modifiable Risk Factors
Elevated Serum Lipids.
Hypertension.
Tobacco Use.
Physical Inactivity.
Obesity.
Contributing Modifiable Risk Factors
Diabetes Mellitus.
Metabolic Syndrome.
Psychologic States.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree