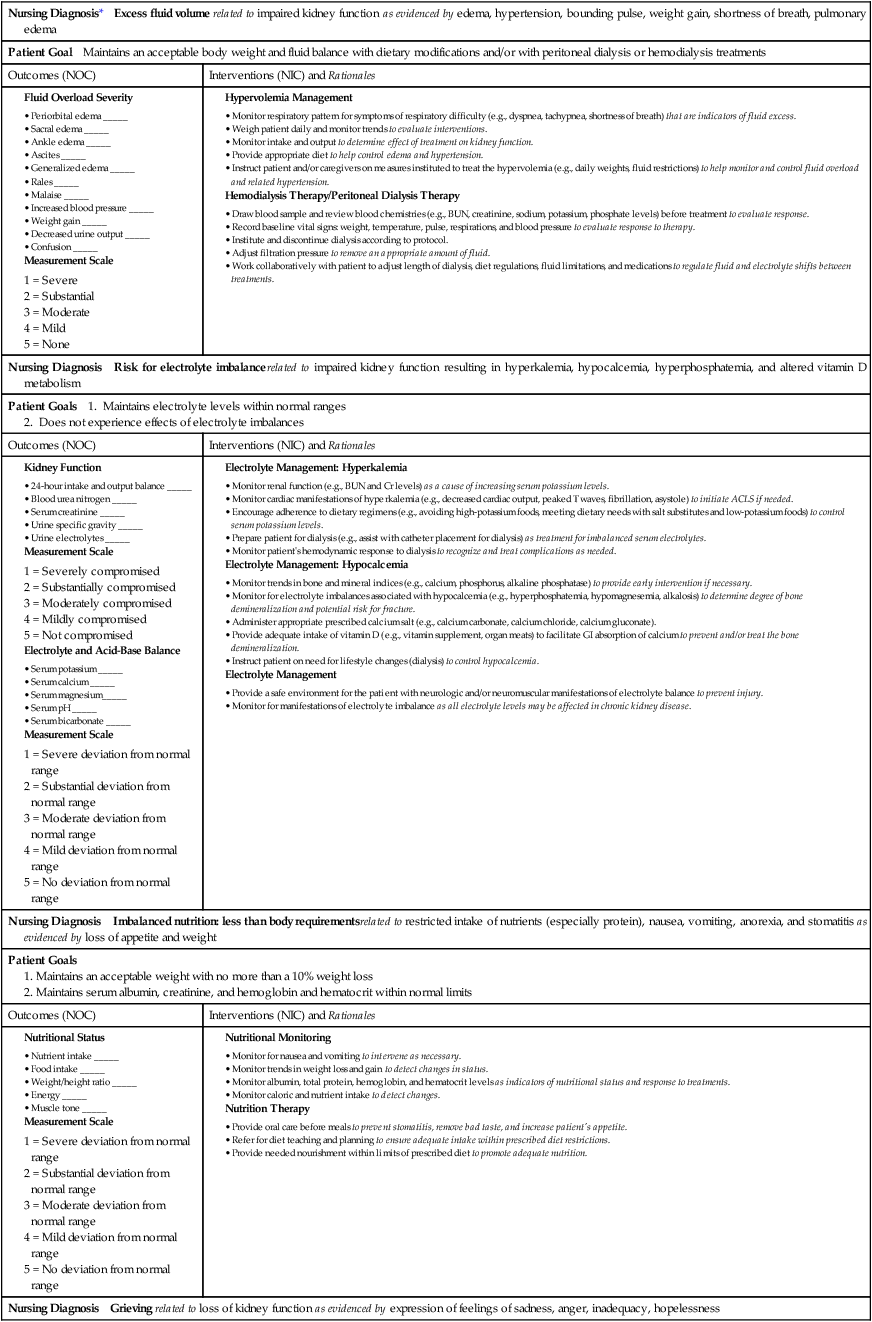
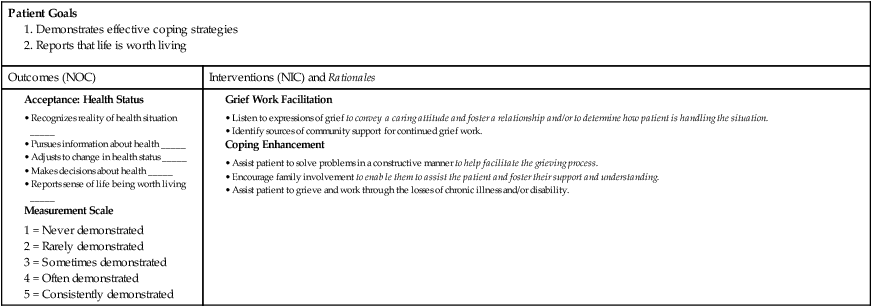
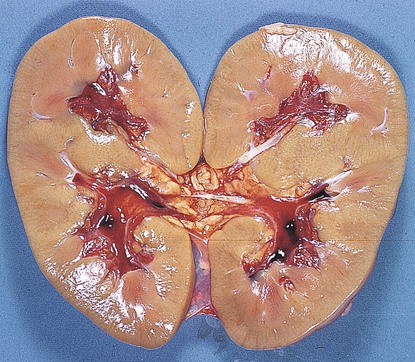
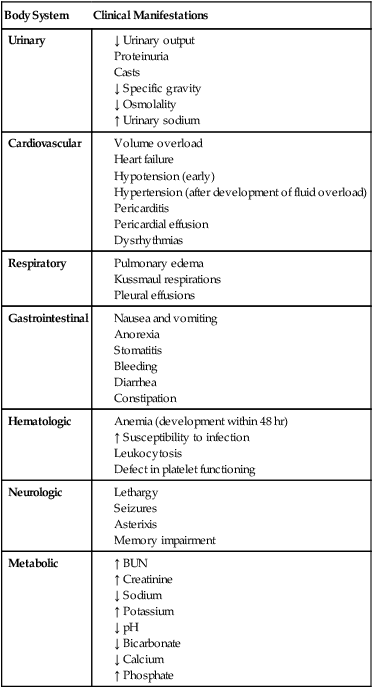
Chapter 47 1. Differentiate between acute kidney injury and chronic kidney disease. 2. Identify criteria used in the classification of acute kidney injury using the acronym RIFLE (Risk, Injury, Failure, Loss, End-stage kidney disease). 3. Describe the clinical course of acute kidney injury. 4. Explain the collaborative care and nursing management of a patient with acute kidney injury. 5. Define chronic kidney disease and delineate its five stages based on the glomerular filtration rate. 6. Select risk factors that contribute to the development of chronic kidney disease. 7. Summarize the significance of cardiovascular disease in individuals with chronic kidney disease. 8. Explain the conservative collaborative care for and the related nursing management of the patient with chronic kidney disease. 9. Differentiate among renal replacement therapy options for individuals with end-stage kidney disease. 10. Compare and contrast nursing interventions for individuals on peritoneal dialysis and hemodialysis. 11. Discuss the role of nurses in the management of individuals who receive a kidney transplant. Reviewed by Kay Helzer, RN, MSN, Former Renal/Pancreas Transplant Coordinator, Banner Good Samaritan Medical Center, Phoenix, Arizona; and Marci Langenkamp, RN, MS, Assistant Professor of Nursing, Edison Community College, Piqua, Ohio. Kidney failure (also called renal failure) is the partial or complete impairment of kidney function. It results in an inability to excrete metabolic waste products and water, and it contributes to disturbances of all body systems. Kidney disease can be classified as acute or chronic (Table 47-1). Acute kidney injury (AKI) has a rapid onset. Chronic kidney disease (CKD) is linked with the development of cardiovascular (CV) disease. TABLE 47-1 COMPARISON OF ACUTE KIDNEY INJURY AND CHRONIC KIDNEY DISEASE eTABLE 47-1 MANIFESTATIONS OF ACUTE KIDNEY INJURY eTABLE 47-2 CASE STUDY Although AKI is potentially reversible, it has a high mortality rate.1 AKI usually affects people with other life-threatening conditions2 (Table 47-2). Most commonly, AKI follows severe, prolonged hypotension or hypovolemia or exposure to a nephrotoxic agent. TABLE 47-2 COMMON CAUSES OF ACUTE KIDNEY INJURY AKI can develop over hours or days with progressive elevations of blood urea nitrogen (BUN), creatinine, and potassium with or without a reduction in urine output. Hospitalized patients develop AKI at a high rate (1 in 5) and have a high mortality rate. When AKI develops in patients in intensive care units (ICUs), the mortality rate can be as high as 70% to 80%.3–5 The causes of AKI, which are multiple and complex, are categorized as prerenal, intrarenal (or intrinsic), and postrenal causes (see Table 47-2). Intrarenal causes of AKI (see Table 47-2) include conditions that cause direct damage to the kidney tissue, resulting in impaired nephron function. The damage from intrarenal causes usually results from prolonged ischemia, nephrotoxins (e.g., aminoglycoside antibiotics, contrast media), hemoglobin released from hemolyzed red blood cells (RBCs), or myoglobin released from necrotic muscle cells. Acute tubular necrosis (ATN) is the most common intrarenal cause of AKI and is primarily the result of ischemia, nephrotoxins, or sepsis (Fig. 47-1). Ischemic and nephrotoxic ATN is responsible for 90% of intrarenal AKI cases.6,7 Severe kidney ischemia causes a disruption in the basement membrane and patchy destruction of the tubular epithelium. Nephrotoxic agents cause necrosis of tubular epithelial cells, which slough off and plug the tubules. ATN is potentially reversible if the basement membrane is not destroyed and the tubular epithelium regenerates. ATN is the most common cause of AKI for hospitalized patients. Risks associated with development of ATN while in the hospital include major surgery, shock, sepsis, blood transfusion reaction, muscle injury from trauma, prolonged hypotension, and nephrotoxic agents (see Table 47-2). Postrenal causes of AKI involve mechanical obstruction in the outflow of urine. As the flow of urine is obstructed, urine refluxes into the renal pelvis, impairing kidney function. The most common causes are benign prostatic hyperplasia, prostate cancer, calculi, trauma, and extrarenal tumors. Bilateral ureteral obstruction leads to hydronephrosis (kidney dilation), increase in hydrostatic pressure, and tubular blockage, resulting in a progressive decline in kidney function. If bilateral obstruction is relieved within 48 hours of onset, complete recovery is likely. After 12 weeks, recovery is unlikely. Prolonged obstruction can lead to tubular atrophy and irreversible kidney fibrosis. Postrenal causes of AKI account for less than 10% of AKI cases.7,8 The RIFLE classification is used to describe the stages of AKI (Table 47-3). Risk, the first stage of AKI, is followed by Injury, which is the second stage. Then AKI increases in severity to the final or third stage, Failure. The two outcome variables are Loss and End-stage kidney disease. (See eTable 47-2 for a case study showing how RIFLE classification is used.) TABLE 47-3 RIFLE CLASSIFICATION FOR STAGING ACUTE KIDNEY INJURY The most common initial manifestation of AKI is oliguria, a reduction in urine output to less than 400 mL/day. Nonoliguria AKI indicates a urine output greater than 400 mL/day. Oliguria usually occurs within 1 to 7 days of the injury to the kidneys. If the cause is ischemia, oliguria often occurs within 24 hours. In contrast, when nephrotoxic drugs are involved, the onset may be delayed for as long as 1 week. The oliguric phase lasts on average about 10 to 14 days but can last months in some cases. The longer the oliguric phase lasts, the poorer the prognosis for complete recovery of kidney function.1 About 50% of patients will not be oliguric, making the initial diagnosis more difficult.5 Changes in urine output generally do not correspond to changes in glomerular filtration rate (GFR). However, changes in urine output are often helpful in differentiating the etiology of AKI. For example, anuria is usually seen with urinary tract obstruction, oliguria is commonly seen with prerenal etiologies, and nonoliguric AKI is seen with acute interstitial nephritis and ATN.8 Even though patients with hyperkalemia are usually asymptomatic, some patients may complain of weakness with severe hyperkalemia. Acute or rapid development of hyperkalemia may result in clinical signs that are apparent on electrocardiogram (ECG). These changes include peaked T waves, widening of the QRS complex, and ST segment depression. Progressive changes in the ECG that are related to increasing potassium levels are depicted in Fig. 17-14. Because cardiac muscle is intolerant of acute increases in potassium, treatment is essential whenever hyperkalemia develops.9
Nursing Management
Acute Kidney Injury and Chronic Kidney Disease
Acute Kidney Injury
Chronic Kidney Disease
Onset
Sudden
Gradual, often over many years
Most common cause
Acute tubular necrosis
Diabetic nephropathy
Diagnostic criteria
Acute reduction in urine output
and/or
Elevation in serum creatinine
GFR <60 mL/min/1.73m2 for >3 mo
and/or
Kidney damage >3 mo
Reversibility
Potentially
Progressive and irreversible
Primary cause of death
Infection
Cardiovascular disease
Body System
Clinical Manifestations
Urinary
Cardiovascular
Respiratory
Gastrointestinal
Hematologic
Neurologic
Metabolic
Intrarenal Cause of Acute Kidney Injury Following Surgery
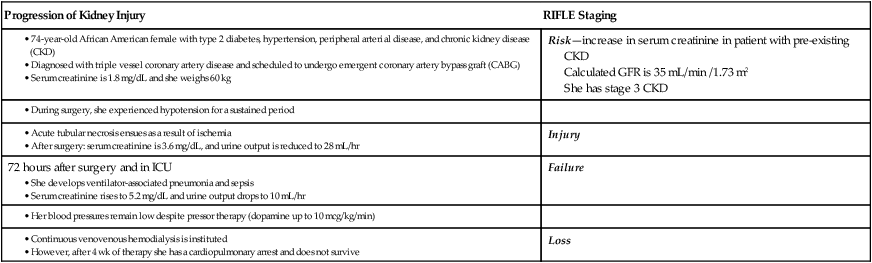
Progression of Kidney Injury
RIFLE Staging
Risk—increase in serum creatinine in patient with pre-existing CKD
Calculated GFR is 35 mL/min /1.73 m2
She has stage 3 CKD
Injury
72 hours after surgery and in ICU
Failure
Loss
Acute Kidney Injury
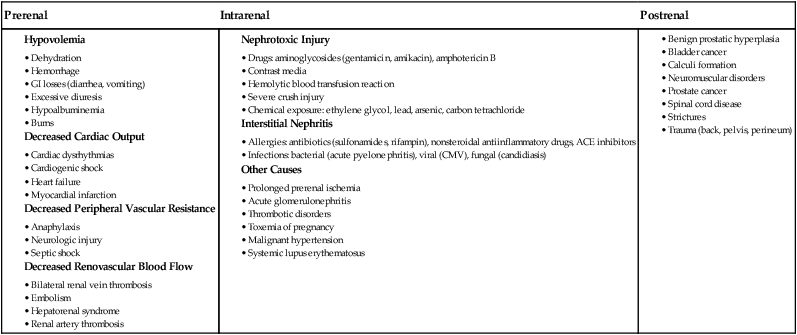
Etiology and Pathophysiology
Intrarenal.
Postrenal.
Clinical Manifestations
Stage
GFR Criteria
Urine Output Criteria
Risk
Serum creatinine increased × 1.5
OR
GFR decreased by 25%
Urine output <0.5 mL/kg/hr for 6 hr
Injury
Serum creatinine increased × 2
OR
GFR decreased by 50%
Urine output <0.5 mL/kg/hr for 12 hr
Failure
Serum creatinine increased × 3
OR
GFR decreased by 75%
OR
Serum creatinine >4 mg/dL with acute rise ≥0.5 mg/dL
Urine output <0.3 mL/kg/hr for 24 hr (oliguria)
OR
Anuria for 12 hr
Loss
Persistent acute kidney failure; complete loss of kidney function >4 wk
—
End-stage kidney disease
Complete loss of kidney function >3 mo
—
Oliguric Phase.
Urinary Changes.
Potassium Excess.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Management: Acute Kidney Injury and Chronic Kidney Disease
Get Clinical Tree app for offline access