Perinatal and neonatal nurses frequently perform the first head-to-toe physical assessment of the newborn. Ideally, this examination occurs in the presence of the parents. Conducting the examination while parents observe allows the nurse to use this time to identify and discuss normal newborn characteristics and note variations. It also provides an opportunity for parents to ask questions about the newborn’s physical appearance and condition. The focus of this chapter is the physical assessment and findings that the perinatal nurse may observe during the time the newborn is in the hospital or birthing center. Home care nurses may also find the information pertinent during early postpartum home visits. Although some references are made to preterm newborns, that subject is not the intended focus of this chapter. It is also assumed that the reader has basic knowledge of physical assessment skills and terminology. Normal findings and common variations for each body system are identified in the text. Tables describe pathologic findings and their causes.
Physical assessment skills of observation, palpation, and auscultation are used frequently throughout the examination. Percussion is not commonly used in the newborn exam. When performing a physical assessment, the following equipment should be available: scale, tape measure, tongue blades, stethoscope with a neonatal diaphragm and bell, and an ophthalmoscope. The initial physical assessment may be conducted with the infant under a radiant warmer or in an open crib. Regardless of the location, attention should be given to avoiding hypothermia and cold stress. Adequate lighting is also essential.
The sequence in which the nurse conducts the physical assessment is a matter of personal preference and most often depends on the cooperation of the newborn. Although we present the newborn assessment as a sequential examination covering one system at a time, the exam can be appropriately conducted in a cephalocaudal fashion, system by system, and more than one system concurrently.
The physical assessment usually begins by observing the breathing pattern, overall skin color, general state or level of alertness, posture, and muscle tone. The newborn’s
state refers to general level of alertness and is a reflection of a group of characteristics that occur together. In the newborn, these characteristics include body activity, eye movement, facial movements, breathing pattern, and level of response to internal and external stimuli (
Pearson, 1999). Understanding the differences in state provides information about how the newborn will respond to the nurse or parents and about the condition of the newborn’s health, and it has implications for parent education.
Appendix 19-A describes newborn states, deep sleep, light sleep, drowsy, quiet alert, active alert, and crying and the implications these states have for caregivers.
The newborn is weighed and measured. It is normal for newborns to lose up to 10% of their birth weight during the first few days of life.
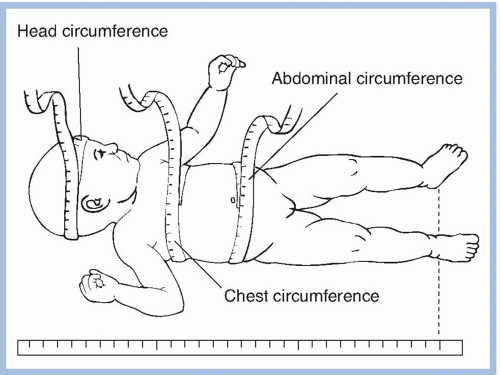
Figure 19-1 illustrates the technique for obtaining accurate measurements. Normal measurements are:
Head circumference, 32 to 38 cm (13 to 15 inches)
Chest circumference, 30 to 36 cm (12 to 14 inches)
Length, 45 to 55 cm (18 to 22 inches)
GESTATIONAL AGE ASSESSMENT
The
American Academy of Pediatrics (AAP) and American College of Obstetricians and Gynecologists (ACOG) (2007) recommend that the gestational age of newborns
be established by incorporating both obstetric and the initial physical and neurologic findings of the newborn. A gestational age assessment, evaluating physical and neuromuscular characteristics, is usually performed as part of the initial physical examination. Although some hospitals make gestational age assessment of all newborns a routine practice, other institutions have established criteria for performing gestational age assessment such as birth weight less than 2,500 g or more than 4,082 g, suspected intrauterine growth restriction (IUGR), gestation less than 37 weeks, and cesarean birth; and in some organizations, it is not part of the nursing assessment but instead determined during the primary care provider’s assessment. Identifying newborns that are preterm, term, or postterm and those who are IUGR, small for gestational age (SGA), appropriate for gestational age (AGA), or large for gestational age (LGA) increases the likelihood of early identification and timely interventions for potential complications related to birth weight and gestational age during the immediate newborn period.
The original tool used for gestational assessment was the Dubowitz Scoring System. It contained 20 items combining neurologic and physical parameters that successfully estimated gestational age in infants older than 34 weeks (
Dubowitz, Dubowitz, & Goldberg, 1970). The tool was revised in 1999, increasing the number of items on the neurologic exam. The test expanded the neurologic exam to include behavior states, tone, primitive reflexes, motility, and some aspects of behavior (
Dubowitz, Ricci, & Mercuri, 2005).
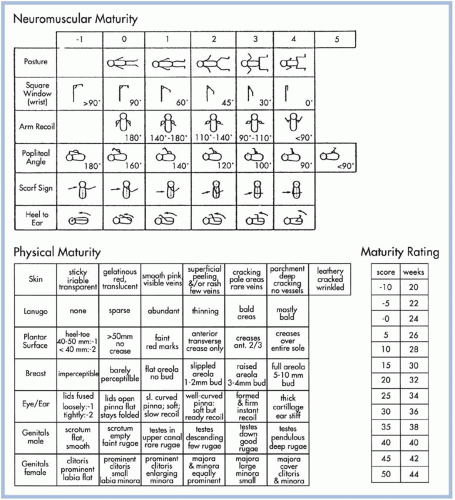
The Ballard Maturational Score (BMS), developed in the late 1970s (
Ballard, Novak, & Driver, 1979), is commonly used for determining gestational age. The original BMS contained 12 items based on the Dubowitz Scoring System. As more low-birth-weight infants were born and survived the initial neonatal period, an instrument that could accurately measure their gestational age was needed to plan initial care. In 1991, the BMS was reevaluated and expanded resulting in the development of a New Ballard Score (
Fig. 19-2), which is what most organizations are using today. Criteria were broadened to provide greater accuracy when evaluating extremely premature neonates (
Ballard et al., 1991).
The BMS is conducted by comparing the individual newborn’s characteristics with the pictures on the form and assigning a number for each characteristic.
Appendix 19-B describes each characteristic evaluated. Controversy exists about the timing of this assessment. The BMS is most accurate if performed between 10 and 36 hours of age. Assessment of newborns younger than 26 weeks’ gestation is best conducted within the first 12 hours (
Gagliardi, Brambilla, Bruno, Martinelli, & Console, 1993). The examination is separated into two parts: neuromuscular maturity assessment and physical maturity assessment. Scores from both sections are added together to determine gestational age.
SKIN ASSESSMENT
The newborn’s entire body, as well as skin folds and scalp, should be inspected and palpated for changes in texture and the presence of masses that are not visible. Color, birth marks, rashes, skin lesions, texture, and turgor are noted. At birth, newborn skin may be covered with vernix, an odorless, white, cheesy, protective coating produced by sebaceous glands. Vernix develops during the third trimester and increases with gestational age. At about 37 weeks, the amount of vernix begins to decrease, and at term, it is present only in the creases of the arms, legs, and neck.
COLOR
Skin color reflects circulation, oxygenation, and hemoglobin saturation. Color is best observed in a well-lit room while the newborn is quiet. At birth, color ranges from pale to plethoric, depending on hematocrit and general perfusion. Skin pigmentation depends on ethnic origin and deepens over time. Caucasian newborns have pinkish red skin tones a few hours after birth, and African American newborns have a reddish-brown skin color. Hispanic and Asian newborns have an olive or yellow skin tone. Changes in the skin color of Caucasian newborns may be the first sign of illness such as sepsis, cardiopulmonary disorders, or hematologic diseases. Variations in skin color indicating illness are more difficult to evaluate in African American and Asian newborns.
Generalized or
central cyanosis may be seen initially at the time of birth as the newborn transitions from fetal to neonatal circulation. Central cyanosis occurring beyond the initial minutes following birth refers to bluish color of the tongue, skin, lips and nail beds in the newborn and, when seen, requires urgent attention by a
physician or advanced practice nurse as it usually indicates a pathologic condition. It is the usually seen when there is less than 5 g of unsaturated hemoglobin per 100 mL of blood or a saturation of < 85% (
Hernandez & Glass, 2005).
Acrocyanosis, the blue discoloration of newborn hands and feet, and
circumoral cyanosis, a bluish color seen around the newborn’s mouth, are normal findings and are often seen in the first 24 to 48 hours of life. Acrocyanosis is related to vasomotor instability and tends to worsen if the newborn becomes cold.
JAUNDICE
Jaundice, a bright yellow or orange discoloration of the skin, results from deposits of unconjugated bilirubin. Up to 60% of healthy term newborns develop some degree of jaundice (
Kaplan, Wong, Sibley, & Stevenson, 2011). Jaundice results from the reduced ability of the newborn’s liver to conjugate bilirubin. A mildly elevated indirect bilirubin level is considered normal in the first few days of life. An elevated direct bilirubin level that may occur as early as 24 hours of life is never normal and suggests some pathology involving the liver. The skin color change associated with an elevated direct bilirubin has a greenish hue (
Gomella, Cunningham, & Eyal, 2009a). Jaundice progresses in a cephalocaudal fashion. Seen first on the head and face, jaundice progresses downward to the trunk and extremities and then to the sclera of the eye. When gentle pressure is applied to skin over cartilage or a bony prominence, skin blanches to a yellow hue on the face when bilirubin levels are 5 mg/dL, on the upper chest when levels are about 10 mg/dL, on the abdomen when
levels are 12 mg/dL, and on the palms and soles of the feet when levels are greater than 15 mg/dL (
Gomella et al., 2009b). Newborns with a positive Coombs test result almost certainly develop jaundice. In dark-skinned newborns, jaundice is more easily observed in the sclera and buccal mucosa.
BRUISING
Ecchymosis may occur over the head or buttocks if forceps or a vacuum extractor was applied or after a breech or face presentation. Petechiae (small pinpointsized reddish to purple spots on the skin) are common over the presenting part, especially when there has been a rapid descent during second stage of labor, but generalized or widespread petechiae are abnormal, may signify low platelet counts, and should be further investigated. Bruising may also result from a tight nuchal cord or an umbilical cord wrapped tightly around the upper body.
VARIATIONS RELATED TO VASOMOTOR INSTABILITY
Cutis marmorata, mottling, or a lacelike pattern on the skin is a vasomotor response to chilling. Parents should be aware that this may continue after discharge. The harlequin sign occurs when some newborns are positioned on their sides. The dependent side of the body becomes pink, and the superior half of the body is pale. This phenomenon is considered benign. The color change lasts 1 to 30 minutes and disappears gradually when the infant is placed on the abdomen or back (
Witt, 2009).
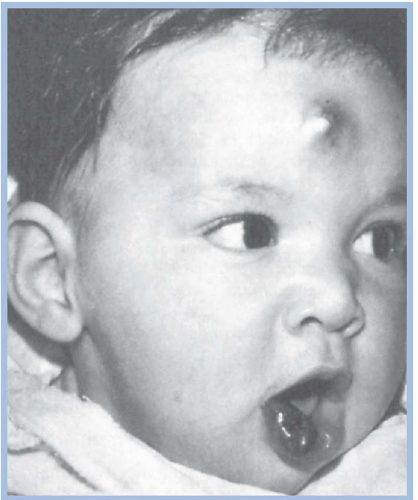
Hemangiomas
Hemangiomas are vascular soft tissue tumors. They may be present at birth and may begin as a pale macule with threadlike markings and develop into a bright red elevated tumor that ranges in size. They can also develop in the first several weeks of life. One percent to 3% of newborns have hemangiomas, and they are more likely to occur in females than in males (
Fig. 19-3). They are generally benign and self-limiting in that they often initially grow but then involute without treatment. However, they may ulcerate, become cavernous, and cause disfigurement or may require intervention (
Hoath & Narendran, 2011).
NEVUS SIMPLEX
Commonly referred to as “stork bites” or salmon patches, these lesions composed of dilated capillaries are macular, irregularly shaped, reddish-colored patches that blanch with pressure and become darker when the newborn cries. Lesions may last 1 to 2 years or persist into adulthood. The most common newborn skin lesion, they are most often seen at the back of the neck, on the forehead, on eyelids, on the bridge of the nose, and over the base of the occipital bones. They may occur in up to 70% of newborns (
Hoath & Narendran, 2011).
PORT-WINE STAIN
Port-wine stains are irregularly shaped, flat pink to reddish markings that are most often present at birth. Color varies from pink in Caucasian infants to black or deep purple in African American newborns or newborns of color. Most often seen on the head and neck, port-wine stains have discrete borders, do not blanch when pressure is applied, and do not lighten as the child ages (
Witt, 2009). These lesions composed of dilated capillaries are generally benign unless they occur along the trigeminal nerve root, in which case they may be associated with glaucoma or optic atrophy, seizures, and mental retardation (
Hoath & Narendran, 2011). Certain types of lasers effectively remove port-wine stains and can be used safely on infants.
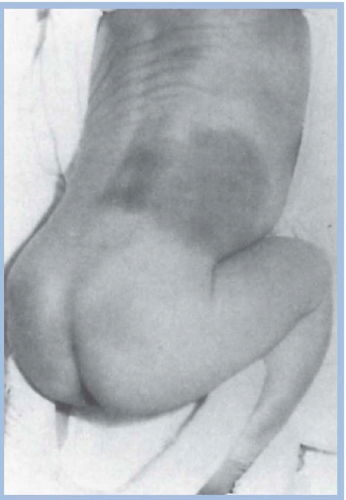
MONGOLIAN SPOTS
Mongolian spots are large, nonblanching, blue-gray lesions resembling a bruise that are most often seen over the sacrum and flanks but may be present on the posterior thighs, legs, back, and shoulders (
Fig. 19-4). They occur frequently in African American, Asian, and Native American infants but can be observed in Caucasian infants (
Hoath & Narendran, 2011). Mongolian spots are caused by infiltration of melaninforming cells into the dermal skin layer rather than the epidermis. Mongolian spots may persist into early childhood but usually fade.
ERYTHEMA TOXICUM
Erythema toxicum, also called newborn rash, is benign and generally occurs within 5 days of birth in approximately 50% of term newborn infants (
Lund & Kuller, 2007). In preterm newborns, the rash may not develop for several days or weeks. Erythema toxicum is composed of small, yellow papules surrounded by an erythematous margin. The rash continues to appear and disappear over various parts of the body for several days. Most commonly seen on the face, trunk, and limbs, it may continue to appear up to 3 months of age (
Witt, 2009).
MILIA
Milia are clogged sebaceous glands that appear as tiny, white, pinhead-sized papules presenting at birth over the chin, cheeks, forehead, and nose. They are benign and disappear during the first month of life (
Lund & Kuller, 2007).
TEXTURE
Skin is evaluated for texture and the presence of lanugo during the physical examination and as part of the gestational age assessment. Texture ranges from smooth to cracked and peeling. Shortly after birth, most term newborns have dry, flaky skin. Peeling, leathery skin with deep cracks indicates postmaturity. Lanugo, a fine, downy hair that covers the body, begins to develop around 12 weeks and is abundant by 17 to 20 weeks’ gestation (
Moore & Persaud, 2008). It is seen in abundance on premature infants. However, it becomes less abundant as gestation increases and is rarely on newborns that are post-40 weeks. At term, lanugo is usually confined to the shoulders, ears, and forehead.
TURGOR
Skin turgor is the natural rebound elasticity of the skin. It can be assessed anywhere on the body by pinching the skin between the examiner’s thumb and index finger and then quickly releasing it. Skin turgor is best assessed on the abdomen. Healthy, elastic tissue rapidly resumes its normal position without creases or tenting. Skin that remains tented indicates poor hydration and nutritional status.
Table 19-1 identifies skin findings during the physical assessment that are abnormal and their related pathology.
HEAD ASSESSMENT
The newborn head is examined using inspection and palpation and assessed for size, shape, and symmetry. The head of a term, AGA newborn has an occipital-frontal circumference (OFC) of 32 to 38 cm (12.5 to 14.5 inches). To measure the newborn’s head, a tape measure is placed just above the eyebrows and continues around to the occipital prominence at the back of the skull (see
Fig. 19-1). At birth, most skull deformities are the result of position in utero, decrease in space in utero due to multiple gestation, decreased amniotic fluid, or intrapartum events (
AAP, 2003). Vaginal birth may cause the cranial bones to overlap (i.e., molding) as the fetus descends through the birth canal or as a result of the application of vacuum or forceps, giving the head an elongated, asymmetric appearance (
Fig. 19-5). The overlapping cranial bones can be palpated along the suture lines. Molding may last several days and cause the head circumference to be smaller immediately after birth. The circumference returns to normal within 2 to 3 days after birth. Newborns delivered by cesarean section or in breech position have a more rounded, symmetric head.
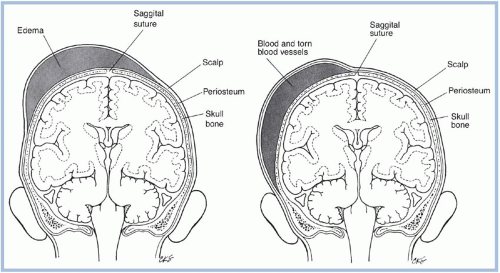
Examination of the newborn head may reveal evidence of birth trauma such as bruising or swelling. A cephalhematoma is a common finding following vaginal delivery. It is a collection of blood between the skull and periosteum, which causes a distinct swelling on the newborn head. Cephalhematomas have clearly demarcated edges and are restricted by suture lines. Common locations for cephalhematomas are the occipital and parietal bones. If large, they can contribute to hyperbilirubinemia and jaundice but in general will resolve in several weeks or months.
Caput succedaneum, edema under the scalp, is caused by pressure over the presenting part of the newborn’s head against the cervix during labor. Caput feels soft and spongy, crosses suture lines, and resolves within a few days.
Figure 19-6 pictorially compares the location of caput succedaneum and cephalhematoma.
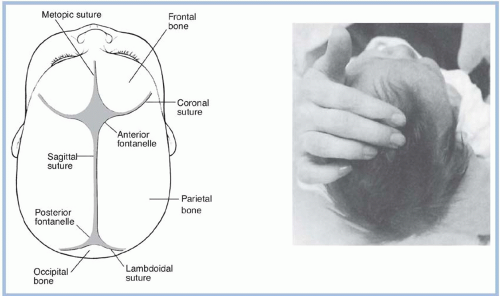
The newborn’s head is palpated for the presence of all suture lines (
Fig. 19-7). Suture lines feel like soft depressions between the cranial bones. If instead a ridge of bone is felt, the examiner should determine whether it is the result of molding or premature closure of the suture. Normal mobility of the cranial bones is determined by placing each thumb on opposite sides of the suture and alternately pushing in slightly on each side. Lack of mobility of cranial bones indicates premature closure of the sutures (i.e., craniosynostosis). Craniosynostosis causes an abnormally shaped head, as the contents of the cranium enlarge, but the cranial bones do not. This abnormally shaped head may be apparent at birth or later in infancy.
The skull is palpated for masses and assessed for craniotabes. Craniotabes are a softening of cranial bones caused by pressure of the fetal skull against the bony pelvis. When pressure is exerted with the examiner’s fingers at the margins of the parietal or occipital bones, a popping sensation similar to indenting a ping-pong ball is felt. Craniotabes is primarily seen in breech presentations and usually disappears within a few weeks.
Anterior and posterior fontanelles, the soft membranous coverings where two sutures meet, are palpated and measured (see
Fig. 19-7). Fontanelles are measured diagonally from bone to bone rather than from suture to suture. They vary in size. The anterior fontanelle is diamond shaped, generally measures 1 to 4 cm, and closes around 18 months of age. The posterior fontanelle is triangular, generally measures less than a fingertip, and closes between 2 and 4 months (
Gardner & Hernandez, 2011). Fontanelles are best palpated when the newborn is quiet. The anterior area should be soft, often is depressed slightly, and may bulge with crying. Arterial pulsations may be felt over the anterior fontanelle. Molding may make it impossible to palpate fontanelles in the first few hours of life. Large fontanelles may be associated with various disorders (such as congenital hypothyroidism) and are a notable finding.
The scalp is examined for distribution, amount, and texture of hair. Hair is silky and may be straight, curly, or kinky, depending on ethnic origin. Bruising, lacerations, and bleeding are frequently seen as the result of the application of a scalp electrode or vacuum extractor.
Table 19-2 identifies findings during the physical assessment of the head that are abnormal and their related pathology.
EYE ASSESSMENT
The newborn’s eyes are assessed using inspection and an ophthalmoscope. This can be done early in the examination as part of the assessment of the head or whenever the newborn spontaneously opens his or her eyes. Although rarely accomplished, it is best done prior to insertion of prophylaxis. Eyes should be symmetric in size and shape. Lids may be edematous and puffy at birth. The distance between the eyes, measured from the inner canthus of each, is 1.5 to 2.5 cm
(
Hernandez & Glass, 2005). Eyes spaced closer (i.e., hypotelorism) or farther apart (i.e., hypertelorism) may be a variation of normal or associated with other anomalies. Eyes with small palpebral fissures (i.e., eye openings) may also be normal or associated with other anomalies.
The colors of eye structures are observed. The iris is usually slate gray, brown, or dark blue. Eye color becomes permanent at about 6 months of age. The normally blue-white sclera may contain subconjunctival hemorrhages, the result of ruptured capillaries during the birth process. Subconjunctival hemorrhages usually resolve within a week. A yellow sclera indicates hyperbilirubinemia. Years ago when silver nitrate was the standard of care for prophylaxis against ophthalmia neonatorum, the conjunctiva would frequently become inflamed. Today, most hospitals are using erythromycin ointment, which usually does not cause this complication.
Tears are usually absent in the newborn until the lachrymal duct becomes fully patent at about 4 to 6 months of age. Prominent epicanthal folds (i.e., Mongolian slant) is a normal finding in Asian infants but may suggest Down syndrome in other ethnic groups.
Blink reflex, size, and reactivity of pupils are evaluated in a darkened room with a pen light or light from the ophthalmoscope. Pupils are equal and reactive to light (PERL). When a light is shined at an angle toward the eye, the lens should be clear. Equal color, intensity, and clarity of the red reflex in both eyes without opacities or white spots within either red reflex is considered a normal exam (
AAP, 2008). Presence and clarity of the red reflex indicates an intact cornea and lens. Lack of a red reflex suggests congenital glaucoma or cataracts. Pale red reflexes are a normal variation in darkskinned newborns.
Movement of the eye is observed. Strabismus, a cross-eyed appearance, is often seen in newborns because of weak eye musculature and lack of coordination. Nystagmus (i.e., constant, rapid, involuntary movement of the eye) may occur and usually disappears by 4 months of age. Newborns are nearsighted at birth and respond to bright or primary colors and to high contrast between colors such as black and white. They see objects clearly 8 to 10 inches in front of them.
Table 19-3 identifies findings during the physical assessment of the eye that are abnormal and their related pathology.
EAR ASSESSMENT
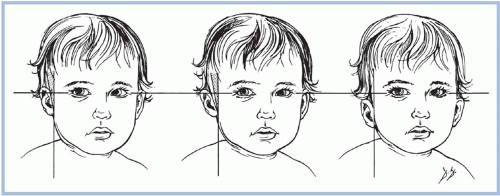
The newborn ear is assessed by inspection and palpation. External structures are examined for position, presence of abnormal structures, and injury, which may have occurred during the birth process. The pinna normally lies on or above an imaginary line drawn from the inner to the outer canthus of the eye, back toward the ear (
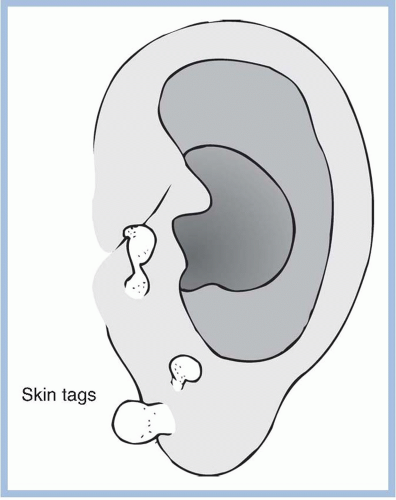
Fig. 19-8). Low-set ears, those that fall below this line, may be associated with genetic
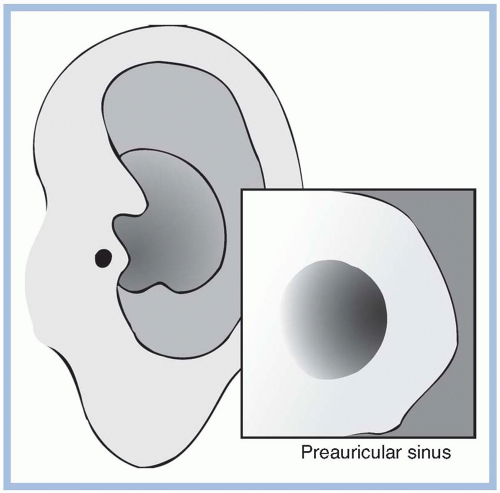
syndromes. Temporary asymmetry of the ears can result from intrauterine position. Skin tags (
Fig. 19-9) and small pits (
Fig. 19-10) located anterior to the ear are usually benign, may be familial, but can also be associated with hearing loss and renal abnormalities. Malformation of the ears may be associated with renal abnormalities, chromosomal abnormalities, and other congenital problems (
Gardner & Hernandez, 2011). Presence of ecchymosis, swelling, abrasions, or lacerations may be the result of pressure during the birth process, application of forceps or vacuum, or injury during cesarean section.
The ear is palpated as part of the gestational assessment to determine the presence and firmness of cartilage. By 38 to 40 weeks’ gestation, the pinna is firm and well formed by cartilage, and incurving is present over two thirds of the ear. A soft pinna lacking cartilage is seen in premature newborns. At term, folding the pinna of the ear inward and releasing should result in brisk recoil. The more premature a newborn is, the slower the pinna will be to return to its normal position. The pinna of an extremely premature infant may remain folded.
The ear canal is inspected for patency. Use of the otoscope is limited because newborn ear canals contain vernix, mucus, and cellular debris. The ear canals clear spontaneously several days after birth. At this time, the tympanic membrane is visualized by pulling
the pinna back and down. The tympanic membrane appears gray-white and highly vascular. If a neonatal ear infection is suspected, otoscopic examination of the ear is indicated.
Although hearing is well developed at birth, it becomes more acute as the ear canals clear. The newborn responds to high-pitched vocal sounds and the familiar voice of his or her mother and father and becomes quiet and relaxed when spoken to in a soft, calm manner. The incidence of hearing loss is 1 to 3 cases per 1,000 well newborns and 2 to 4 cases per 1,000 newborns admitted to intensive care nurseries (
AAP, 1995). In 1994, the Joint Committee on Infant Hearing (JCIH), of which the AAP was a member, first proposed universal hearing screening of all newborns (
AAP, 1995). The
AAP (2007) currently recommends that all newborns should receive hearing screening using a physiologic measure by 1 month of age (preferably before hospital discharge). Two technologies are available for hearing screening: evoked otoacoustic emissions (OAE) and auditory brainstem response (ABR). Both methods are noninvasive, quick, and easy to perform. However, OAEs reflect only the status of the peripheral auditory system up to the cochlear outer hair cells, while ABRs can also detect neural dysfunction. It is for this reason that infants that have been hospitalized in the neonatal intensive care unit (NICU) for greater than 5 days are to have ABR screening rather than OAE screening, so that neural hearing loss can be identified (
AAP, 2007).
Support for universal newborn hearing screening (UNHS) is based on the premise that if identification and intervention occur by 6 months of age for newborns that are hard of hearing or deaf, the infants will perform significantly higher on vocabulary, articulation, and other school-related measures because of the ability for language development (
AAP, 2007).
Table 19-4 identifies findings during the physical assessment of the ear that are abnormal and their related pathology.
NOSE ASSESSMENT
The newborn’s nose is assessed using inspection. The nose should be symmetric and midline but may be misshapen at birth because of the neonate’s positioning in utero. If the septum cannot be easily straightened and the nose remains asymmetric, treatment may be required. A flattened or bruised nose may result from passage through the birth canal.
Nasal stuffiness and thin, white mucus is not an uncommon finding immediately after birth. Newborns sneeze to clear the upper respiratory tract. Nasal flaring, widening of the nares, is a compensatory mechanism that decreases upper airway resistance, allowing more air to enter the nasal passages. Nasal flaring is abnormal and one of the first symptoms observed when respiratory distress occurs.
Table 19-5 identifies findings during the physical assessment of the nose that are abnormal and their related pathology.
Bilateral nasal patency should be established in all newborns as they are obligatory nose breathers. Patency should be determined by either obstructing one nare and observing breathing through the opposite nare or passing a 5 French catheter down each nare. However, if a newborn is breathing comfortably and patency is established by obstructing one nare, there is no need to pass a catheter, and this should be done only if nare obstruction is suspected.