Shock: the basic mechanisms346
Shock: The Basic Mechanisms
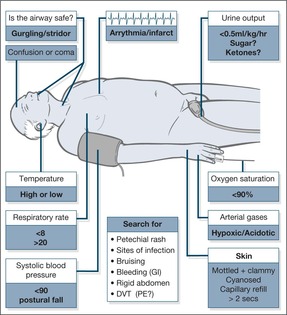
Fig. 10.1
Cardiogenic shock
Hypovolaemic shock
Clinical observations
% of total blood volume
BP
Pulse
Respiratory rate
Mental state
IV therapy
BLOOD LOSS
750ml
15%
N
90
N
THIRSTY
SALINE
1500ml
30%
LOW
120
>20
ANXIOUS CONFUSED
BLOOD
Redistributive (low-resistance) shock
Acute Severe Hypotensive Collapse
CASE 1
Initial observations
CASE 2
Initial observations
CASE 3
Initial observations
Importance of Immediate Resuscitation
Resuscitation of the patient with hypotensive collapse
Rapid assessment in the critically ill: the importance of ABCDE
Common examples of the critically ill
Recognition of a deteriorating patient
Threats to the airway
Respiratory failure
Circulatory failure
Falling level of consciousness
Critical nursing tasks in assessing hypotensive collapse
Maintain the safety of the patient
Measure the respiratory rate and the oxygen saturations
Measure the radial and apical pulse rates
Measure the lying blood pressure and look for any postural decrease
Ensure large-bore venous access
Obtain an immediate 12-lead ECG
Keep the relatives on the ward
Important nursing tasks in assessing hypotensive collapse
Monitor the heart
Assess the site and severity of any pain
Reassure the patient about the management plan and initiate symptom relief
Explain
Acute LVF:
less dyspnoeic, falling pulse, good diuresis
Upper gastrointestinal bleeding:
less thirsty, less light-headed, no further vomiting, clearing of melaena
Speak to the relatives
Access further information
Basic management plan
Nursing observations to monitor the response
When do we use dopamine, dobutamine and noradrenaline (norepinephrine) in patients with shock?
Which one to use?
How to monitor their effectiveness
Ensuring Adequate Oxygen Delivery to Vital Organs: Maintaining the Oxygen Saturation and the Blood Pressure
Oxygen therapy

Fig. 10.2
Oxygen masks
The blood pressure
When is a central line used?
Inserting a central venous line: subclavian and internal jugular venous cannulation
The central venous pressure
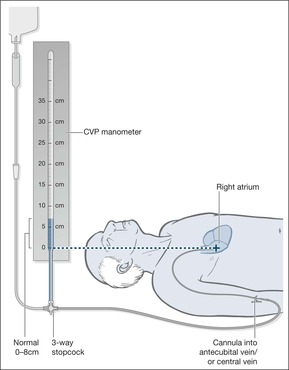
Fig. 10.3
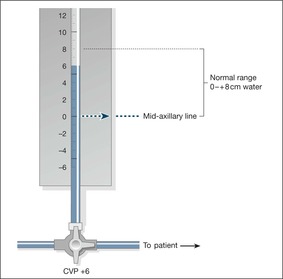
Fig. 10.4
Fluid challenge
Which Critically Ill Patients May Need Transfer to Intensive Care/HDU?
Surviving Sepsis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Multisystem failure
Surviving sepsis365
Anaphylactic shock365
In the early stages, the extremities are cool as blood is diverted to more important areas, the pulse increases and the blood pressure starts to fall.
Once established, shock causes a cold clammy skin, tachycardia and increased respiratory rate. Oxygen saturations decrease. The urine output is reduced due to impaired blood flow to the kidneys. The release of lactic acid from ischaemic, poorly perfused tissues leads to an acidosis. Acidosis in turn impairs cardiac function and leads to further falls in the blood pressure.
In severe shock, reduced perfusion to the brain leads to agitation, restlessness and eventual coma. By this stage, the reduced blood supply to the kidneys means there may be little or no urine output.
Box 10.1
• A systolic blood pressure of less than 90mmHg
• A tachycardia
• An increased respiratory rate (above 20 breaths/min) and reduced oxygen saturations
• Mottled, cool and clammy skin
• Evidence of hypovolaemia: dry mouth, dry axillary skin, postural hypotension, thirst
• Low urine output (less than 0.5ml/kg per h)
• Confusion or agitation progressing to coma
There are three forms of shock: cardiogenic shock, hypovolaemic shock and redistributive (low-resistance) shock.
In cardiogenic shock, the heart as a pump fails to propel blood around the circulation. The common causes of cardiogenic shock are:
1. Heart muscle damage – a myocardial infarction severe enough to damage a large part of the left ventricle will reduce the cardiac output sufficiently to produce shock.
2. Severe arrhythmia – an acute rapid arrhythmia, most commonly atrial fibrillation, can reduce the blood pressure enough to cause shock. This commonly occurs in the setting of a pre-existing acute illness such as DKA or pneumonia.
3. Valve disease – acute valve failure is an important reversible cause of cardiogenic shock. Sudden mitral regurgitation can complicate myocardial infarction and acute aortic incompetence can complicate bacterial endocarditis.
4. Output obstruction – this is seen in massive pulmonary embolus: the output from the right side of the heart is suddenly cut off by a clot lodging in the main pulmonary arteries, leading to sudden profound shock.
Hypovolaemic shock is probably the most important type to recognise; it is relatively easy to treat and is rapidly fatal if allowed to progress. In hypovolaemic shock, there is a reduction in the circulating blood volume due to either external fluid loss or ‘internal loss’ by fluid being sequestrated within the body’s internal compartments.
Common medical causes of acute external fluid loss are:
• upper gastrointestinal bleeding (Table 10.1)
• severe diarrhoea and vomiting
• diabetic ketoacidosis
Internal fluid loss is seen in:
• acute pancreatitis
• severe paralytic ileus
Redistributive shock is due to the effect of circulating toxins disturbing the normal distribution of blood flow within the body. Some vessels, notably those in the skin, open up and provide little or no resistance to blood flow. Other vessels shut down in a pattern in which organs such as the kidney are starved of blood. In contrast to the other forms of shock, in redistributive shock the overall resistance to blood flow is reduced: the cardiac output is therefore high, the pulse is bounding and the peripheries are warm. The patient appears flushed and warm rather than grey and clammy. Without treatment, however, the progression is the same as that in other forms of shock – to kidney failure and to increasingly severe acidosis.
The main causes of redistributive shock are:
• sepsis, especially from gut and renal tract infections
• anaphylaxis
Clinically, patients with shock present to the Acute Medical Unit as a problem of acute severe hypotensive collapse. Given this clinical situation, there are five groups of conditions to consider:
Case Studies 10.1
A 70-year-old woman is admitted with collapse.
She is coughing frothy sputum and cannot lie flat. She has pulse 160 beats/min, blood pressure 90/60mmHg, saturations 80%, respiratory rate 35 breaths/min, and temperature 37.4°C.
• This is pulmonary oedema due to acute heart failure – cardiorespiratory collapse
• She needs to be sat up and given immediate oxygen
• Her low blood pressure and high pulse are due to the heart problem
An 80-year-old man with a urinary catheter is admitted with confusion and rigors.
He is hot and delirious, with rigors. He has pulse 115 beats/min, blood pressure 70/40mmHg, saturations 82%, respiratory rate 30 breaths/min, and temperature 38.5°C.
• This is septicaemic shock
• He needs urgent oxygen, i.v. fluids and immediate antibiotics
• Progress can be judged from the blood pressure and urine output
A 50-year-old man has collapsed after vomiting a large amount of fresh blood.
He is cold, clammy and very restless. He has pulse 130 beats/min, blood pressure 100/50mmHg lying and unrecordable on sitting, saturations 88%, respiratory rate 40 breaths/min, and temperature 36.5°C.
• This is hypovolaemic shock
• He needs urgent oxygen, a large cannula, rapid i.v. fluids then blood
• Progress can be judged from the falling pulse rate and increasing blood pressure
2. massive pulmonary embolus
3. septicaemia (→ Case 2 in Case Studies 10.1)
4. hypovolaemia (→ Case 3 in Case Studies 10.1)
5. anaphylaxis
These deficiencies in the first critical hours of admission have an impact on the patient’s chance of recovery, especially, as in Case Study 10.2, where there is sepsis. Once the condition deteriorates to septic shock, the mortality rate approaches 50%. In this case, the priority should have been to correct the oxygen saturation and try and restore a blood pressure within the first half hour of admission. The admitting nurse and doctor must share their information from the initial assessments in order to draw up an effective management plan. There are critical time intervals between the admission and the first:
• dose of antibiotics
• treatment with oxygen
• initiation of i.v. fluids
• correction of the blood pressure
Case Study 10.2
A patient came in at 13.30h and was clerked in at 16.30h. Although the nursing notes record a blood pressure of 90/40mmHg, this is not recorded in the doctor’s clerking. Blood gases were taken on admission, but the results were not recorded in the notes.The chest X-ray showed a right upper lobe pneumonia.
At 19.30h the registrar was asked to see the patient because of persistent hypotension. A blood pressure of 60/40mmHg was noted, as were the abnormal blood gases and a high creatinine (indicating a renal problem). Intensive i.v. fluids were started.
The patient had a central line put in at 01.30h, 12h after admission, and was transferred to the ITU. Noradrenaline (norepinephrine) was needed to restore the blood pressure. By the second day, the whole of the right upper lobe had consolidated due to the rapid progression of pneumococcal pneumonia.The pneumococcus bacterium was grown in two sets of blood cultures taken on admission.
It is important to identify the patient who needs a high priority for resuscitation. This is done by the triage system, ABCDE. In these critically ill patients, resuscitation will commence before the full diagnosis is apparent.
Look. A respiratory rate of < 8 breaths/min (depressed respiration) or > 20 breaths/min suggests a serious problem.
• Remember that an increased respiratory rate is seen in any cause of shock, even if the lungs are normal.
• Measure the oxygen saturation: a level below 90% indicates severe hypoxia.
• Does breathing look like hard work or is the patient tired and losing interest?
• Does this look like acute asthma?
In LVF, the patient will be sitting upright and coughing frothy sputum.
Listen. Gurgling indicates aspiration and needs urgent aspiration of the mouth and oropharynx (attempting to aspirate the larynx or trachea may trigger laryngospasm) with a rigid Yankauer suction catheter.
• Acrowing sound or a harsh inspiratory stridor suggests acute upper airway obstruction, which is seen in acute epiglottitis or severe tonsillitis
• Snoring suggests an unsafe airway and is seen in coma or stroke
• Wheezing occurs in COPD, asthma, LVF and massive pulmonary embolus
Feel. A finger sweep may be needed to clear an airway or obstruction. Well-fitting dentures can be left, as they will make it easier to apply a mask and maintain an airway.
C: The circulation. An impalpable pulse suggests a systolic blood pressure of less than 80mmHg. Hypotension is the major finding in shock and, if severe, will be associated with an increased respiratory rate, anxiety and confusion due to reduced blood flow to the brain. Other features of a low blood pressure will be cool and clammy skin, reduced capillary refill and a low hourly urine output (< 0.5ml/kg per hour). Capillary refill time provides an important assessment of the state of the circulation: after digital pressure has been applied to a finger tip for 5s, the capillaries should refill in less than 2s – a delay indicates an impaired circulation and is a useful sign, especially in hypovolaemic shock.
Important: An increased pulse rate may only appear as a late sign of shock, especially in otherwise fit young patients, and occasionally the response to a major internal bleed may be a slowing of the pulse. An increase in respiratory rate is frequently the first sign in shock.
D: Disability. Check the consciousness level quickly using the AVPU score (alert, responding to voice/pain, unresponsive; →Chapter 4: Acute neurological problems; p. 104). Use the GCS for a later more detailed assessment if the conscious level is impaired.
Shocked patients are restless and often uncooperative due to impaired circulation to the brain.
Cardiac arrhythmia. A man comes in with very rapid atrial fibrillation and hypotension after suffering a painless myocardial infarction at home.
Massive pulmonary embolus. An obese woman in her 20s collapses with breathlessness, syncope and hypotension a week after a caesarean section.
Anaphylaxis. A young man with nut allergy collapses with wheeze and hypotension after inadvertently consuming peanuts during a Chinese meal.
Gastrointestinal bleed. A man in his 40s vomits a pint of fresh blood and passes a large melaena stool. He comes in with hypotensive collapse.
Acute abdomen. A woman aged 35 years, known to have gallstones, comes in with a 12-h history of increasing abdominal pain, hypotension and signs of acute pancreatitis.
Septicaemia. An elderly lady has a week’s history of vomiting and diarrhoea and is admitted to hospital with hypotension and renal failure. Her blood cultures yield Salmonella.
Pneumonia. A 35-year-old man becomes increasingly breathless and confused during an influenza epidemic. He is hypotensive and hypoxic. The chest film shows pneumonia.
Soft tissue infection. A 60-year-old woman with multiple sclerosis is admitted with hypotension and drowsiness. She has necrotic infected sacral pressure sores and positive blood cultures.
Chapter 1 outlined the basis of using simple nursing observations in scoring systems which can be used to recognise the patient who is deteriorating and is at risk. The scores are used to document clinical progress and to trigger corrective measures, particularly through the involvement of Critical Care Outreach Teams.
The assessment aims to recognise what is initially reversible that, unless corrected, will progress to:
1. persistent hypotension
2. increasing acidosis
3. kidney failure
4. cardiorespiratory failure
5. cardiorespiratory arrest
Box 10.2 summarises the clinical findings that need urgent attention on the Acute Medical Unit.
Box 10.2
N.B. Patients who have a cardiac arrest often go through a warning period of unrecognised deterioration in their vital signs.
• Impending obstruction: anaphylaxis with swollen tongue, epiglottitis
• Unsafe airway: impaired consciousness level or stroke
• Respiratory arrest
• Respiratory rate low (< 8 breaths/min) or very high (> 30 breaths/min)
• Poor arterial gases: pO2 less than 8.0 kPa on at least 60% oxygen pCO2 more than 6.5 kPa pH less than 7.2
• Pulse less than 40 or greater than 140 beats/min
• Systolic blood pressure less than 90mmHg
• Urine output (i.e. circulation to the kidneys) of less than 30ml/h
• GCS of less than 12 or a fall of 2 or more
Secure the airway and maintain oxygenation.
Choose the most appropriate oxygen delivery system to bring the saturations above 90%. When there is doubt, administer continuous high-flow oxygen at 15 L/min through a tight-fitting mask with a reservoir bag. The doctors will do urgent blood gas measurements to:
• assess the adequacy of the oxygen therapy
• look at the degree of acidosis (low pH and low bicarbonate)
• use the CO2 levels as a measure of adequate ventilation
• measure the blood lactate levels (high) as evidence of poor overall tissue perfusion
These critical results must be communicated to the medical staff.
If the pulse is weak, use the monitor or an ECG trace. Rapid atrial fibrillation will give a deficit between the apical and radial pulses.
Hypotension will, in general, require i.v. fluid replacement or drugs to support the heart. A patient with a systolic blood pressure of less than 90mmHg will show signs of reduced blood flow to the brain – restlessness, confusion and a reduced conscious level. Reduced blood flow to the kidneys results in reduced hourly urine output.
Venous access must be obtained immediately, as the priority in shock is often the need for urgent fluid replacement.
This will exclude myocardial infarction and acute arrhythmias as the cause of the hypotension.
▪ Maintain the safety of the patient
▪ Measure the respiratory rate and oxygen saturations
▪ Measure the radial and apical pulse rates
▪ Measure the lying blood pressure and look for any postural decrease
▪ Ensure large-bore venous access
▪ Obtain an immediate 12-lead ECG
▪ Keep the relatives on the ward
You may require urgent information concerning:
• the recent history (in the elderly, any sudden deterioration can be due to sepsis)
• previous health and levels of dependence, history of substance or alcohol abuse
• details of medications and allergies
• information to inform future discussions regarding resuscitation status
For the best trace, use adhesive electrodes placed over bony prominences. The skin should be shaved and cleaned with alcohol. The red electrode should be placed below the right clavicle, the yellow one in the same position on the left, and the green electrode below the left rib margin.
Examples of pain in sudden hypotensive collapse are:
• severe chest pain: myocardial infarction or pulmonary embolus
• severe abdominal pain: perforation/acute pancreatitis/leaking abdominal aneurysm
• Relieve breathlessness: give oxygen and sit the patient up if he wishes (unless hypovolaemic)
• Ensure the mask is comfortable and tight-fitting and that the patient understands that he is to keep it on
• Prepare the patient for possible further procedures:
— blood gas sampling (wrist arterial puncture)
— central venous line placement (via internal jugular or subclavian veins)
— urinary catheterisation
— further tests (endoscopy, CT, ultrasound). It is critical that resuscitative measures are not compromised while the patient is off the ward
Explain what has gone wrong and what will be the signs of improvement, e.g.:
• Explain what they will see: drips, monitors, urinary catheters, masks
• Explain the management plan
• Explain the signs of improvement or deterioration
• Forewarn the relatives that the patient may need to be transferred to an HDU/ITU
Obtain the previous hospital records and any previous laboratory results urgently.
An example of the immediate management of hypotensive collapse in a man with abdominal pain is given in Case Study 10.3.
Case Study 10.3
A 30-year-old man was admitted with a 3-day history of upper abdominal pain. He was reluctant to give many details and denied any significant past history, but he was clearly in considerable discomfort and was very agitated. His wife was with him and added that he had been drinking a litre of strong cider a day for several years and that, 6 months previously, he had been investigated for alcohol-related liver damage and told that he should stop drinking for good.
Initial assessment was of a wasted man lying restlessly in bed with severe upper abdominal pain. His GCS was 15 but he scored only 7/10 on an abbreviated mental test score. His respiratory rate was 30 breaths/min and oxygen saturations 88%. His pulse rate was regular at 120 and his blood pressure was 90/70mmHg lying and 70/50mmHg sitting up. On general exposure there was scattered bruising and he appeared moderately jaundiced. His abdomen was distended, tense and silent but only moderately tender.The BM stix was satisfactory at 7.0mmol/L.
1. He was given high-flow oxygen at 60% with immediate improvements in his saturation to 98%
2. Venous access was obtained with difficulty and blood was taken for:
— FBC – to look for bleeding (low Hb) and infection (high white cell count)
— platelets – he is bruised, and alcoholics have low platelet counts
— biochemistry:
• to check for dehydration (U&E)
• to exclude acute pancreatitis
• to check the liver function tests
— Clotting – bruising can indicate a serious coagulation disturbance
3. Arterial blood gases were taken to look at the oxygen level and to identify acidosis (a common problem resulting from hypotension in the setting of an acute serious illness)
4. While awaiting initial results a small dose of i.v. opiates was administered to provide immediate pain relief and he was reassured that further analgesia would be available once the test results had been seen.
The investigations showed a very high amylase (1500 IU), abnormal liver function and early kidney failure. Combined with the clinical assessment the overall picture was of acute pancreatitis complicated by redistributive shock:
• hypotension
• confusion
• hypoxia
• poor kidney function due to hypotension
• Administer continuous oxygen immediately
• Provide effective analgesia
• Bring up the blood pressure urgently
— assess the i.v. fluid requirements with a central venous pressure line
— administer sufficient i.v. fluid to bring the CVP up to 15 cmH2O of water
— if this does not bring up the blood pressure consider inotropic support
• Use the urine output to assess the response to the improved blood pressure (catheter)
• Rest the gastrointestinal tract with nasogastric intubation on free drainage
• Hourly urine output to aim at > 50ml/h
• Hourly pulse
• Hourly blood pressure
• Hourly pain score
• 2-hourly oxygen saturations
• 2-hourly temperature (shock, central lines and the underlying disease can all lead to sepsis)
• Careful charting of input and output
• Continuous cardiac monitoring
In this man’s case the initial urine output was 10ml in the first 3h, in spite of vigorous fluid replacement, and his blood pressure remained low. He was therefore started on i.v. dopamine at 5μg/kg per min. His blood pressure responded, followed after 2h by an increase in his urine output.
Dopamine. Dopamine is used in the range 2–20mg/kg per min. At the lower dose it acts to improve kidney perfusion (although the clinical value of this is questionable), in the mid range it also begins to stimulate the heart, and at the higher doses it begins to constrict peripheral arteries to produce additional beneficial effects on the blood pressure. It is the most widely used ‘general-purpose’ inotrope. It is usual to start with the lower dose and increase accordingly.
Dobutamine. Dobutamine only stimulates the heart and tends to be reserved for cardiogenic shock.
• The blood pressure
• The mental state (brain blood flow)
• The hourly urine output (kidney blood flow), which should be kept above 0.5ml/kg per h
• The blood lactate levels (lactate levels fall as tissue perfusion improves)
There are two adverse effects that must be identified:
1. if the vasoconstrictor effect on the peripheral vessels is too strong, the patient can develop ischaemic tips to their fingers and toes, i.e. fixed blue/black discolouration
2. the cardiac stimulation can lead to marked tachycardia and then arrhythmias: these patients need close cardiac monitoring
The main indications for emergency oxygen therapy are:
• oxygen saturations of less than 90%
• systolic blood pressure of less than 100mmHg
• respiratory distress (respiratory rate of more than 20 breaths/min)
• cardiac or respiratory arrest
• acidosis on blood gas results
There is understandable anxiety about the correct dose of oxygen in patients with COPD, but in general the problem in acutely ill medical patients is not giving too much oxygen, but in giving too little. The aim, whatever the circumstances, should be to give sufficient oxygen to raise the oxygen saturation above 90%. Oxygen is a drug and, unless in an emergency, it should be prescribed – the prescription should specify the mask, the flow rate and, in the case of the Venturi mask, the oxygen concentration. A target oxygen saturation should also be specified. The aim should be for a normal saturation (94% to 98%) in most acutely ill medical patients and for saturations of 88% to 92% in those (usually patients with severe COPD) who are at risk from Type II (hypercapnic) respiratory failure. The different techniques of oxygen administration are illustrated in Fig. 10.2.
• Simple face masks (Hudson masks, MC masks) – these provide up to 60% oxygen at flow rates of 6–10 L/min, but underperform at rates of less than 5 L/min. These masks are suitable for most situations in which emergency oxygen is needed.
• Nasal prongs – the percentage of oxygen delivered by nasal prongs at 2 L/min is between 25% and 30%. At 4 L/min around 40% will be delivered. Nasal prongs are less intrusive than masks and tend to be better tolerated in uncooperative patients. Although oxygen delivery with nasal prongs may be inadequate for a critically ill patient, they are suitable for most situations in which emergency oxygen is needed.
• Non-rebreathing mask with reservoir bag – Depending on their fit, these masks can administer from 60% to 100% oxygen with flow rates set at 15 L/min. Proper use requires some expertise because the mask must fit tightly, the reservoir bag must be filled before the patient starts to breathe and the flow rate requires adjustment to ensure the bag remains at least half full throughout the respiratory cycle. Non-rebreathing masks with reservoir bags are used in the critically ill to correct severe hypoxia.
• Oxygen therapy during nebuliser treatment – In patients with acute asthma the nebuliser can be driven by oxygen at 6 L per minute or by compressed air combined with nasal prongs to maintain target saturations. In COPD oxygen should not be used to drive the nebuliser but nasal prongs at 2 L min during air-driven nebulisation should keep the saturations between 88 and 92%.
There are two main reasons why the blood pressure can suddenly fall in the critically ill. First, the heart may start to fail as a pump – examples would be an acute myocardial infarction or the toxic effects of septicaemia. Secondly, there may not be enough fluid returning to the heart to fill it sufficiently; examples would be rapid blood or fluid loss or the sudden loss of vascular tone seen in overwhelming sepsis. Improving the circulation of the blood by restoring the blood pressure is as important as correcting the amount of oxygen contained in it. It is critical to ensure there is sufficient circulating volume to carry any additional oxygen to the tissues. If there is hypotension and evidence of inadequate tissue perfusion – notably oliguria, poor capillary refill and impaired conscious level – an urgent challenge with 500–1000ml of i.v. saline should be considered.
• To assess the state of the circulation from the central venous pressure
• To gain access to major veins:
— when there is no peripheral access
— for administration of irritant infusions or drugs, e.g. dopamine and amiodarone
• To insert a temporary pacemaker
These are the two preferred sites for inserting central venous lines. Placement involves the Seldinger technique, in which the vein is first cannulated with a needle, through which is pushed a guide wire. The needle is removed, leaving the wire in place, and then the cannula is fed into the vein over the guide wire, which itself is then withdrawn. Success rates have improved and complications are less common with the use of portable ultrasound machines to locate the central veins before cannulation.
The procedure
1. Are the results of clotting studies available to the operator?
2. This is a sterile procedure: masks, gowns, drapes, gloves and full skin preparation are required.
3. 2% aqueous chlorhexidine is more effective as a skin disinfectant than povidone-iodine
4. The patient must be 20° head-down to prevent air entering the cannula (air embolus) during insertion.
5. The operator must check the trolley and packs before starting the procedure.
6. The infusion should be run through and ready.
7. If a multi-lumen catheter is inserted, the staff must be pre-briefed about its correct use.
8. Decide beforehand what dressings are to be used to secure the site.
9. Explain and reassure the patient (and the relatives) about the procedure:
— the rationale for needing a central line
— the fact that it is a routine method of monitoring/administering certain treatments
— local anaesthetic will be used
— the doctor will provide an appropriate level of information on the benefits and risks
— it would be normal practice to obtain written consent if the patient is well enough.
The CVP is a simple measurement that gives important information about the overall state of the circulation, and specifically about the degree of hydration. The measurement is taken from the height of a vertical column of fluid that is in free communication with a central venous catheter (→Fig. 10.3 and Fig. 10.4). If the patient is lying flat, the reference point from which the measurement is made is in the mid-axillary line at a point vertically below the sternal angle. This coincides with the position of the right atrium.
The normal central venous pressure is from 0 to + 8 cmH2O
The central venous pressure is abnormally high in congestive cardiac failure and in overtransfusion; it is too low in hypovolaemic and septic shock, in which values of −3 cmH2O or less will be found.
In a sick patient with a low blood pressure, the CVP provides invaluable information on the fluid requirements, which may not be obvious from simple observation. In particular, patients who are septic tend to be dehydrated:
• they have a poor intake
• they have been sweating
• the respiratory rate is increased, so there is increased respiratory fluid loss
• patients with sepsis often have diarrhoea
In these patients, a fluid challenge can be given with confidence if there is a combination of hypotension and a low CVP. Conversely, if the blood pressure is low but the CVP is high, the cause may be cardiac and a fluid challenge would be inappropriate.
Hypovolaemia is the most likely cause of hypotension (systolic blood pressure < 90mmHg) in the critically ill patient and in these circumstances, once the airway is secured and oxygen saturations are corrected, the circulating volume is expanded using relatively large amounts of fluid over a short period of time. The term ‘fluid challenge’ applies to the combination of aggressive volume expansion and a careful assessment of its effect on the patient. Either a crystalloid (500–1000ml of isotonic saline or 5% dextrose) or a colloid (300–500ml of polygeline [Haemaccel]) is given over 30 min and if necessary repeated. The response is evaluated using the vital signs, capillary refill, and urine output. The patient is observed for signs of fluid overload: overfilling of the neck veins (increased JVP), and new-onset breathlessness with wheezing and crackles (pulmonary oedema) at the lung bases.
• When there has been a respiratory arrest – these patients remain at marked risk until the underlying problem (pneumonia, asthma, etc.) has been treated.
• Arespiratory rate of less than 8 or more than 40breaths/min – extremes of respiratory rate indicate severe illness with impending cardiorespiratory arrest.
• Oxygen saturations that remain less than 90% in spite of at least 50% oxygen by mask – these patients will need extra respiratory support, possibly even intubation and ventilation of the lungs.
• Apulse rate of less than 40 or greater than 140beats/min in spite of treatment – this can be evidence of circulatory failure, although clearly straightforward uncontrolled atrial fibrillation would not come into this category.
• Asystolic blood pressure that stays below 90mmHg in spite of fluid replacement – this suggests established shock and may need support with inotropic drugs.
• An unexpected and sudden fall in the conscious level – (a fall in GCS of more than 2 points). This may be a manifestation of falling cerebral blood flow due to persistent shock.
• Increasing arterial carbon dioxide tension with acidosis – deteriorating blood gases in spite of treatment is a warning of impending respiratory arrest
• Any patient giving cause for concern in whom there is a reasonable expectation of recovery
There is increasing concern about the rising incidence of severe sepsis as a cause of critical illness and the very high associated mortality – approaching 40% in the UK – some of which can be reversed with better early resuscitation, particularly in the first 6h of admission. The key is to recognise:
• significant sepsis-induced tissue under-perfusion
• increased respiratory rate
• hypotension
• increased blood lactate levels (> 2–4mmol/L)
Once sepsis is recognised, initial therapy with aggressive fluid challenge (20ml/kg of saline), oxygen, early antibiotics and if necessary dobutamine/noradrenaline (norepinephrine) will significantly improve the outlook.
Get Clinical Tree app for offline access

