Multiple Practice Changes Promote a Culture of Shared Responsibility to Reduce Patient Falls and Fall Injuries
Marilyn S. Mokracek MSN, RN, CCRN, NE-BC1
Cheryl Novak Lindy PhD, RN-BC, NEA-BC2
1Nurse Manager mmokracek@sleh.com
2Director, Nursing and Patient Education and Research
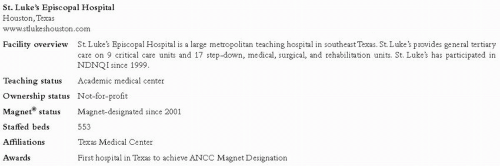
St. Luke’s Episcopal Hospital Houston, Texas
www.stlukeshouston.com
Case Study Highlights
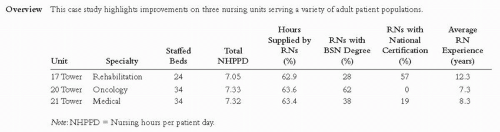
New equipment and additional staff were combined with safety huddles, visual cues communicating risk status, and immediate post-fall debriefing to reduce total and injury falls. These changes fostered a philosophy of shared responsibility for patient safety. After two years of success, injury fall rates began to trend upward and additional best practice interventions are being pursued.
Fall Rates above NDNQI Benchmark Spur Quality Improvement
In 2006, fall rates at St. Luke’s Episcopal Hospital (see Figure 1) indicated an opportunity for improvement in preventing patient falls and fall injuries. On the medical and rehabilitation units, the eight-quarter averages for total falls per 1,000 patient days were higher than the corresponding NDNQI® eight-quarter average median. Injury fall rates for the same units were equal to or below the eight-quarter NDNQI means. The hospital’s Best Practice Council facilitated a multi-faceted fall prevention initiative that was combined with new equipment and additional staff time to successfully reduce falls and related injuries throughout the hospital.
Best Practice Council Creates Fall Prevention Team
St. Luke’s Best Practice Council was created in September 2006 to replace the nursing quality program as a mechanism to promote performance improvement through evidence-based outcomes. The previous nursing quality program focused on nursing documentation compliance instead of performance improvement and patient outcomes. The Best Practice Council changed the focus to investigating patient outcomes variances and providing evidence-based direction for clinical change to enhance quality patient care. The Best Practice Council identifies quality problems
and creates interprofessional teams to review and test evidence-based practices. These smaller teams identify promising interventions and test them in the current environment to ensure positive impact. The team then makes recommendations to the larger Best Practice Council, which then mandates the practice change throughout the organization.
and creates interprofessional teams to review and test evidence-based practices. These smaller teams identify promising interventions and test them in the current environment to ensure positive impact. The team then makes recommendations to the larger Best Practice Council, which then mandates the practice change throughout the organization.
The Patient Falls Prevention Best Practice Team was one of the first teams created by the larger Council in September 2006. The team leader and membership were selected from multiple units and disciplines. Team members included nursing staff and management, physical therapy, radiology, clinical nurse specialists, and nursing research. The team was directed to identify and implement best practices to reduce the number of patient falls. The team’s original goal was to reduce total falls per 1,000 patient days to 2.0 or fewer, with no moderate or serious injury.
Development of the Falls Prevention Initiative
The team assessed the hospital’s current practice and outcomes data. Retrospective chart review demonstrated
patients were correctly assessed and identified as being at risk for falls, but interventions to prevent falls were not consistently implemented or documented by nursing staff. After evaluating current practice, the team reviewed recent research (Krauss, Evanoff, Hitcho, Ngugi, Dunagan et al., 2005; Mills, Neily, Luan, Stalhandske, & Weeks, 2005). The review of falls prevention literature revealed three recommendations for practice change:
patients were correctly assessed and identified as being at risk for falls, but interventions to prevent falls were not consistently implemented or documented by nursing staff. After evaluating current practice, the team reviewed recent research (Krauss, Evanoff, Hitcho, Ngugi, Dunagan et al., 2005; Mills, Neily, Luan, Stalhandske, & Weeks, 2005). The review of falls prevention literature revealed three recommendations for practice change:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree