chapter 6
Mental Health Nursing
After studying this chapter, the student should be able to:
1 Define ego defense mechanisms; name five examples.
2 Compare and contrast therapeutic communication techniques and ineffective responses, citing five examples of each.
3 Describe three types of anxiety disorders, including their characteristics.
4 Explain mood disorders and the role of the interventions appropriate to the specific form.
5 Describe thought disorders, citing three examples and their symptoms.
 http://evolve.elsevier.com/Mosby/comprehensivePN
http://evolve.elsevier.com/Mosby/comprehensivePN
HOLISM
A Definition: This concept of health holds that illness results from a complex interaction among the mind, body, spirit, and the environment, a concept that views an individual as more than the sum of his or her parts.
B Approaches to treatment: Multifaceted approaches are used to treat disturbances rather than simply relying on treatment aimed at specific symptoms. We are no longer content to treat the illness; we are learning to treat the whole person. Approaches include the following dimensions:
MENTAL HEALTH CONTINUUM
A Mental health and mental illness are seen as opposite poles on a continuum.
B The precise point at which an individual is deemed mentally ill is determined by the specific behavior exhibited and the context in which the behavior is seen.
C Some behaviors that are considered inappropriate in one setting may be considered normal in another setting.
D Variations are based on culture, the time or era, personality, and other variables.
E Behaviors of mentally ill people are often exaggerations of normal human behaviors.
MENTAL HEALTH
A Definition: an individual’s ability to cope with problems in life and draw satisfaction from living throughout various life stages
B Individuals may experience times of greater or lesser satisfaction with life; during times of lesser satisfaction they may seek the assistance of a therapist or counselor.
C No clear set of characteristics specific to mental health can be identified.
MENTAL ILLNESS
A Definition: a pattern of behavior that is disturbing to the individual or the community in which the individual resides; behaviors may interfere with daily activities, impair judgment, or alter reality. A mental illness is a disturbance of a person’s ability to cope effectively, which results in maladaptive behaviors and impaired functioning.
1. The person who is mentally ill may act in ways that seem unrelated to current reality. (Depressed individuals may not exhibit this type of behavior.)
2. Relationships with family and friends are frequently disturbed.
3. The person’s ability to function effectively and contribute to his or her own welfare may be impaired.
4. The person often experiences subjective discomfort.
5. The person may exhibit symptoms such as delusions, hallucinations, paranoia, hopelessness, passive-aggressive behavior, or compulsions.
B Historical perspective of mental illness
a. Mentally ill people were thought to be possessed by supernatural forces, evil spirits, or demons.
b. Mentally ill people were removed from society, frequently mistreated in other ways, and often jailed.
c. These beliefs and practices have lasted many years; some are still practiced today.
2. Classical era (Greco-Roman)
a. Early Greek physicians began to see nature as a healing force.
b. This early scientific interest led to various classification systems.
c. The idea of divine possession was rejected in favor of the humoral theory of disease.
d. Humors were thought to be basic internal fluids capable of controlling behavior.
e. The terms melancholia and hysteria are derived from these ancient beliefs.
3. The Middle Ages, Renaissance, and Protestant Reformation eras saw some reform; however, in general:
a. Society returned to the idea of divine possession or spiritual explanations for mental illness.
b. The mentally ill person was often mistreated by incarceration.
4. Individuals responsible for instituting reforms in the modern era
(1) Phillipe Pinel freed the mentally ill from chains.
(2) Benjamin Rush, known as the Father of American Psychiatry
(1) Florence Nightingale, known as the founder of modern nursing
(2) Dorothea Dix promoted legislation to establish mental hospitals.
(1) Clifford Beers wrote the book The Mind That Found Itself, which generated public concern for the mentally ill.
(2) Adolf Meyer founded the mental hygiene movement.
(3) Emil Kraepelin classified mental disorders.
(4) Eugene Bleuler coined the term schizophrenia and classified it into types.
(5) Sigmund Freud developed psychoanalytical theory.
(6) Carl Jung developed the personality theory that included introversion and extroversion.
(7) Karen Horney theorized that culture influences mental illness.
a. Discovery of phenothiazines (the major tranquilizers such as chlorpromazine [Thorazine]) in the 1950s
b. Community mental health: 1960s; still in use today. The aim is to provide care of mentally ill people in their own communities rather than in large institutions. Primary goals of the community mental health concept are to return patients to their home as quickly as possible and foster the development of culturally appropriate support systems in the community.
c. Deinstitutionalization: In the late 1970s a large number of mentally ill people were released from long-term hospitals into communities where they often did not receive treatment either because they did not seek it or because adequate types of services were not available. Some people believe that this process led to an increase of street people and homelessness.
d. Community mental health centers were established to provide comprehensive treatment within the community.
e. Development of more effective psychotropic medications has helped to decrease treatment costs.
C Common mental health terms: The following terms are not defined in other sections of this chapter
2. Hysteria—the unconscious conversion of anxiety into physical symptoms; somatization
3. Kinesics—body communication via movements, posture, expression, gesture
4. Narcissistic—self-absorption to an extreme degree
5. Paralinguistics—the voice quality; volume, tone, speed, flow, inflection, and other audible sounds other than words, for example, laugh, cry, moan
6. Proxemics—manner in which individuals relate to space and distance with others; influenced by culture
7. Self-esteem—an individual’s assessment of self-worth and value
NURSING ROLE
1. Assessment: The LPN/LVN gathers subjective and objective data through observation, interview, and examination. Data are obtained through:
(1) General description—appearance, speech, motor activity
(3) Intellect and sensorium—consciousness, memory
(4) Thought content and processes—what is thought (e.g., delusions, phobias) and how one thinks (e.g., blocking, flight of ideas)
(1) Intelligence testing—standardized tests administered by psychologists, designed to assess intellectual capacity
(2) Personality testing—standardized tests administered by psychologists, designed to assess specific personality traits
d. Self-assessment (e.g., stress scale, decision-making trees).
2. Diagnosis: Nurses diagnose and treat human responses to illness. The nursing diagnosis is formulated by the registered professional nurse; the LPN/LVN contributes to this phase of the nursing process by collecting objective and subjective data. Potential nursing diagnoses identify the problem and etiological factors of the problem; actual nursing diagnoses identify the problem, origin, and signs and symptoms. The North American Nursing Diagnosis Association International (NANDA-I) listing is used. Examples of actual and potential nursing diagnoses used in mental health nursing include the following (these are examples, not a complete listing):
a. Anxiety (panic) related to family rejection; exhibited by chest discomfort, palpitations, dizziness, diaphoresis, and trembling
b. Impaired social interaction related to negative role modeling; exhibited by verbalized and observed discomfort in social situations
c. Risk for self-directed violence related to history of suicide attempts
It is critical for nurses to consider many areas when formulating nursing diagnoses for patients experiencing mental health issues and to identify the ones that will best meet all the needs of a particular patient. These areas include:
a. Promotion of both mental and physical health and well-being
b. Overall functional ability of the individual
c. Differences in the individual’s thinking, understanding, and communication skills
d. Behaviors of the individual that, combined with mental health issues, increase the risk of danger to self or others
e. Effects of emotional stress on the individual in light of current circumstances
f. Management of unwarranted symptoms (side effects) from medications and ordered treatments
g. Barriers that could interfere with treatment and overall recovery of the individual
h. Changes in the individual’s concept of self, including that of body image
i. Physical symptoms that could result from the individual’s mental status
j. Psychological symptoms that may be due to changes in physical needs
k. Factors that influence the individual, the family, or the community (social, religious, cultural, environmental)
l. Factors that could affect the individual’s recovery (financial security/job, family/community support, housing)
Consideration of these areas will be advantageous when moving into the planning phase of the nursing process.
3. Planning: Plan of care is based on the nursing diagnosis. Specific nursing interventions are devised to attain specifically stated goals. When possible, goals should be developed jointly with the cooperation of patient or family or both. They may be short-term or long-term goals; all goals should be prioritized, emphasizing reduction or elimination of the identified problem. They usually include the anticipated length of time for accomplishment and the standard for judging whether the goal has been met.
4. Implementation: Planned nursing actions that assist patient in achieving the identified goal (e.g., health teaching, assist with activities of daily living [ADLs], other prescribed treatments, medications). This phase is ongoing, and reactions to treatment are observed and documented so the care plan may be modified periodically as goals are met.
5. Evaluation: Outcome achievement and the factors that affected the goal being met, partially met, or not met are identified. This process is followed by the decision to continue, modify, or terminate the plan. After evaluation of goal achievement, the entire nursing process and care plan are reviewed, modified, or updated to reflect new nursing diagnoses.
B Critical thinking: The application of critical thinking in the delivery of nursing care is essential. The concept incorporates the sum total of the nurse’s knowledge, experience, assessments, and clinical judgment. The nurse questions assumptions and continuously seeks the highest level of nursing practice. It is probing and creative in assessment. Thoughtful, outcome-oriented, and prudent, critical thinking contributes greatly to optimum outcomes for the patient. Critical thinking has been defined by Wilkenson (2001) as “careful, goal-oriented, purposeful thinking that involves many mental skills, such as determining which data are relevant, evaluating the credibility of sources and making inferences.”
C Principles of mental health nursing: The nurse must:
1. Provide for and maintain a therapeutic environment, called milieu therapy.
2. Understand own inner needs, thoughts, and feelings and be aware of how these affect patients.
3. Be aware of own resources and limitations so as to function effectively in mental health nursing.
4. Respect patient as a person; take time to listen to what is said.
5. Be considerate of patient’s dignity; show patience and understanding.
6. Establish a trusting relationship, which requires an accepting, nonjudgmental, and nonthreatening approach.
8. Reassure patients by being available, allaying fears, and being consistent.
9. Explain routines, rules, and regulations when appropriate.
10. Maintain a calm, hopeful attitude.
11. Encourage reality orientation, and avoid entering into patient’s unrealistic thinking.
12. Emphasize strengths that patient displays by acknowledging healthy behavior and offering warm understanding. Do not encourage overdependency or intimacy.
13. Remember that all staff members are role models and are often viewed as authority figures by patients.
14. Help reduce anxiety by making as few demands as possible on patients.
15. Explain to patient what is happening in simple, understandable language.
16. Remain objective but do not display aloofness or distance; maintain awareness of patient’s humanity and dignity.
17. Maintain a nurse-patient relationship that is always realistic and professional.
18. Remember that a reason exists for all behavior.
19. Note that behavior is changed through emotional experience rather than through rational means.
20. Patients must be allowed to exercise all of their basic human rights.
21. Use the least-restrictive method or methods of controlling behavior such as effective communication.
D Communications in mental health nursing
1. Communication: complex activity consisting of a series of events, each interdependent on the others, which results in a negotiated understanding between two or more people in a given situation
a. Communication is not merely the exchange of information.
b. Each message (input) generates an extremely complex reaction that eventually leads to a selective response (output), which in turn becomes a new input for the communicators.
a. The most apparent form is verbal (written or spoken language) communication; spoken communication is the tool frequently used in mental health nursing.
b. Spoken communication is always accompanied by at least one of the following additional communication forms:
(1) Paralanguage: voice quality, tones, grunts, and other nonword vocalizations
(2) Kinesis: facial expression, gestures, and eye and body movements
(3) Proxemics: the spatial relationship between people
(4) Touch and messages to other sensory organs: aromas and cultural artifacts (jewelry, clothing, hairstyle)
c. Effective communication includes:
3. Therapeutic communication (Box 6-1)
4. Blocks to communication (Table 6-1)
Table 6-1
Ineffective Responses That Hinder Therapeutic Communication
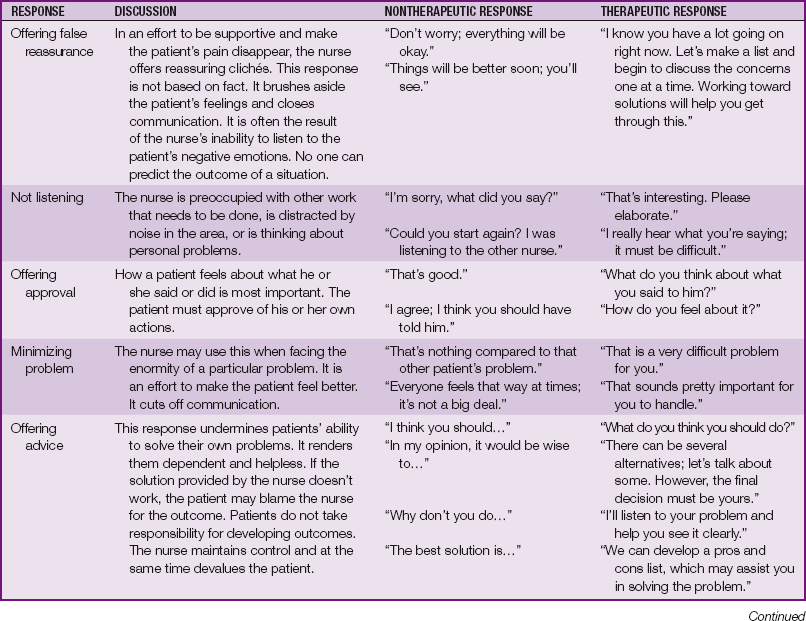
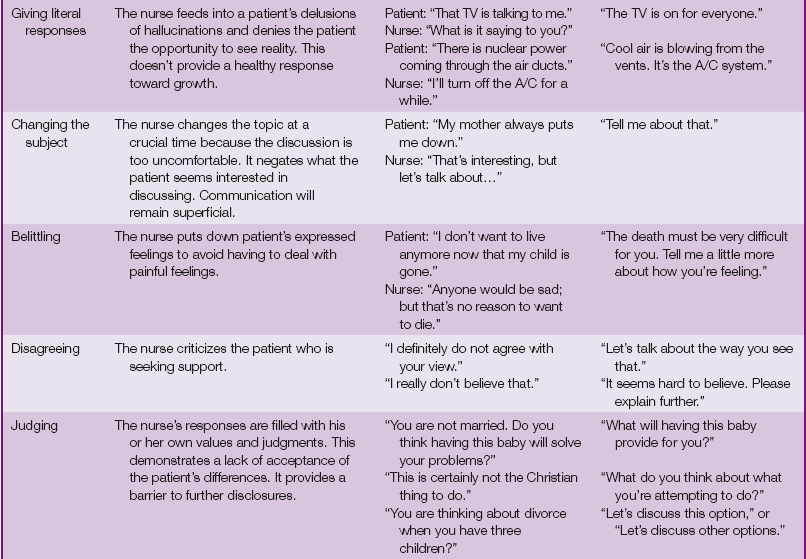
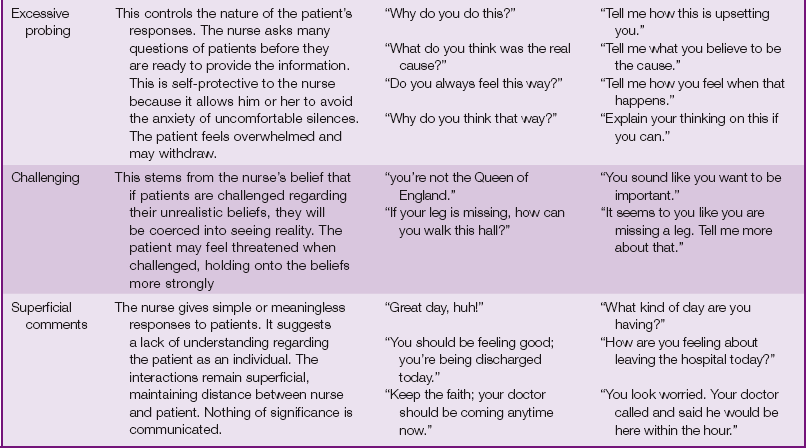
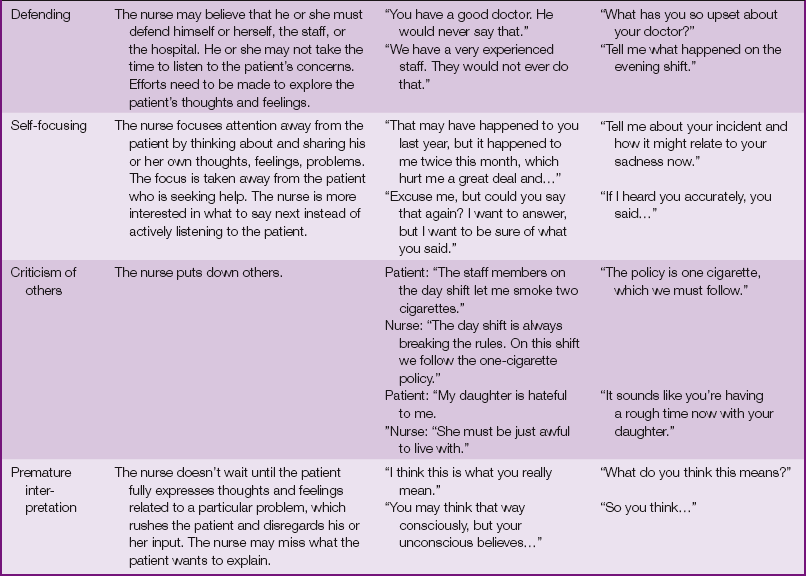
Modified from Fortinash KM, Holoday Worret PA: Psychiatric–mental health nursing, ed 4, St Louis, 2008, Mosby.
1. One-on-one relationship between a nurse and a patient
4. Not for nurse’s satisfaction
5. Focus on modification of patient behavior, increasing patient’s self-worth, and improving patient’s coping strategies
6. Therapeutic, not social, relationship
a. Preorientation (preparation): about patient; self-analysis of attitudes, biases, and perceptions by the nurse
b. Orientation: two to ten sessions. Nurse and patient become acquainted; trust and rapport are established; parameters of the relationship are also established; discussions are contracted; patient problems are identified. The plan is built on patient’s strengths.
c. Working begins when patient demonstrates responsibility to uphold terms of the contract. Establish priorities and goals with patient. Help patient achieve behavior change (e.g., discussion, role playing). Focus on the present. Reinforce the contract terms as necessary.
d. Termination begins during orientation phase; purpose is to conclude the relationship. Focus on patient growth, and help patient with expression of feelings about relationship closure.
Note: Some authors and models list three phases: orientation, maintenance, and termination.
F Settings of mental health nursing
PERSONALITY DEVELOPMENT
A Definition: the sum total of unique components (i.e., thoughts, feelings, physical composition, behavioral traits, and attitudes) that distinguish one individual from another
1. Personality is influenced by inherited characteristics, both physical and psychological.
2. Controversy exists regarding the extent of genetic influence on specific human behaviors.
1. The environment is a strong determining factor in the individual’s development.
2. Environment includes the intrauterine environment and all of the external factors that influence the individual after birth.
D Physical basis: Personality can develop normally if the necessary physical basis is present.
1. The brain is the major organ of thought and is vital to the development of personality.
2. The endocrine system strongly influences behavior as well.
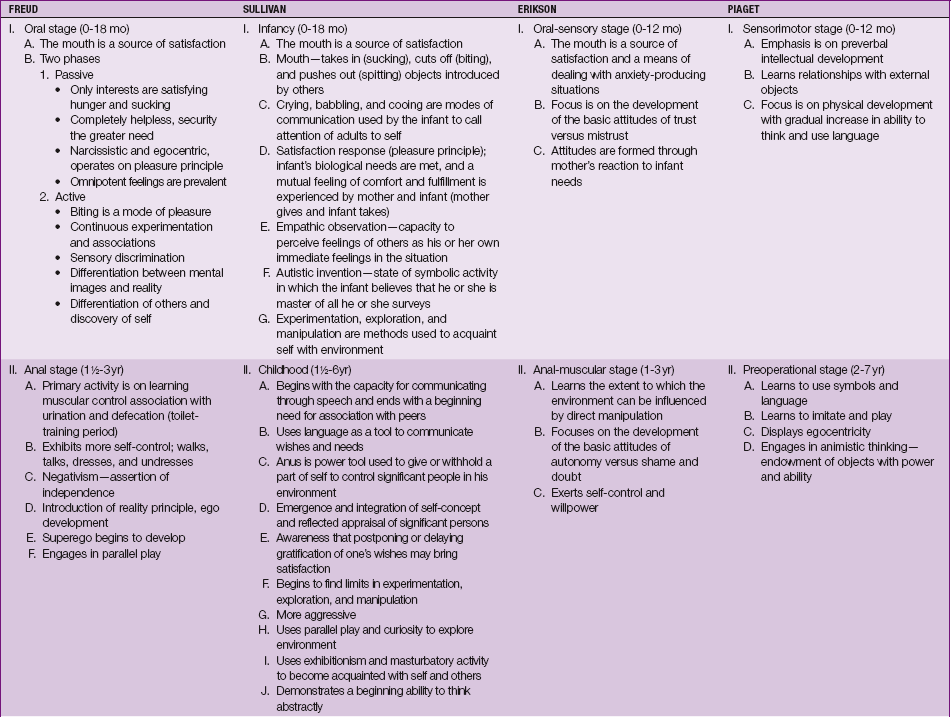
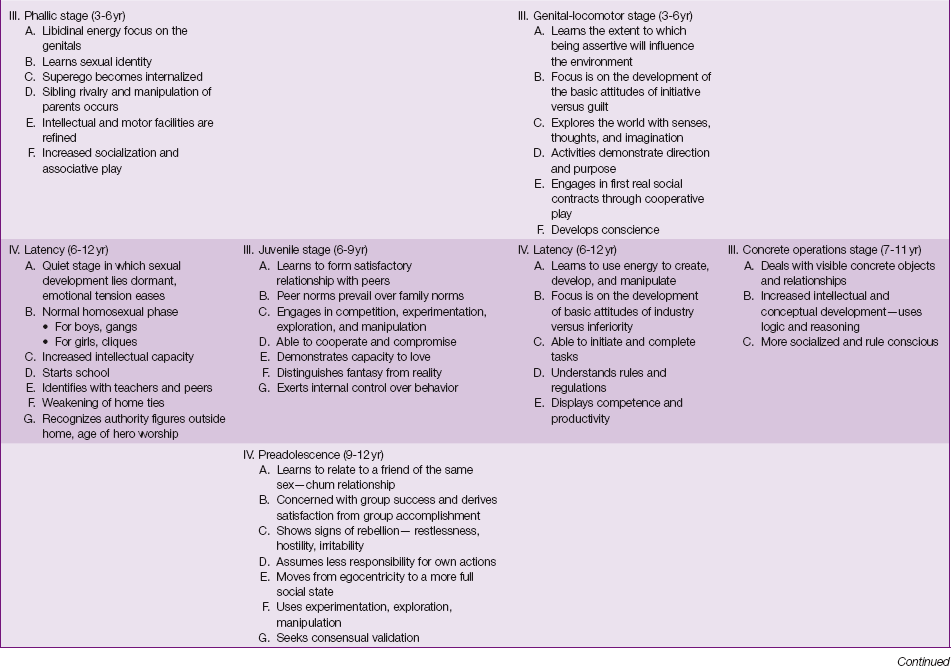
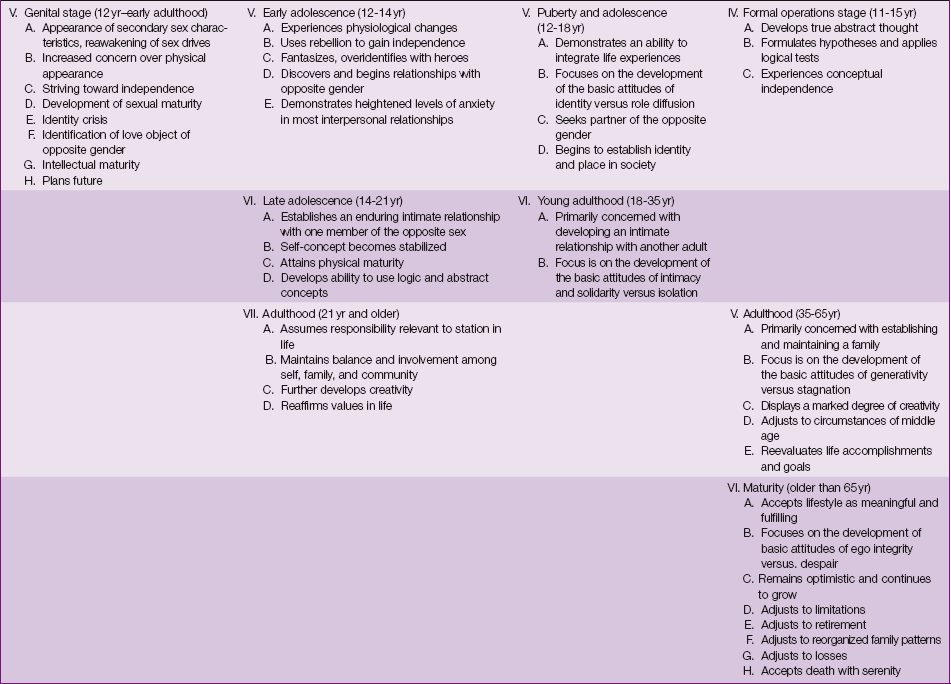
E Major theorists: comparison of Freud, Sullivan, Erikson, and Piaget (Table 6-2)
F Elements of personality (Freud)
a. The unconscious: always outside the awareness of the individual; influences actions in ways the individual may not understand; thought to include dreams
b. The preconscious: usually outside awareness; available to the conscious mind in special circumstances such as under hypnosis or during therapy
2. Structures: Some theorists refer to personality structures.
a. Freud: ego, id, and superego
b. Berne: child, adult, and parent
(1) Eric Berne was the psychiatrist best known as the founder of Transactional Analysis; he labeled the three ego states as child, parent, and adult as opposed to id, ego, and superego.
(a) The child interactions reflect feelings and desires—for example, “I’m afraid.”
(b) The parent interactions focus on aspects such as values, moral concepts, and rules—for example, “Please shut the door,” “Be quiet in church.”
(c) In adult interactions the individual uses learned concepts and prior knowledge—for example, “The stove is hot,” “A broken clock is right twice a day.”
(2) Berne also established the concept of strokes, which can be either positive or negative.
(3) He believed that individuals receiving positive strokes will thrive and be encouraged to have positive interactions. (Morrison-Valfre)
3. Functions: Each structure is thought to perform specific functions (Freud).
G Development levels: Various theorists describe levels of development.
1. Freud (infant, child): oral, anal, phallic, latency, genital
2. Erikson (incorporates levels across the life span): basic trust versus mistrust; autonomy versus shame and doubt; initiative versus guilt; industry versus inferiority; identity versus role diffusion; intimacy versus isolation; generativity versus stagnation; ego integrity versus despair
H Development of the self-concept
EGO DEFENSE MECHANISMS
Ego defense mechanisms are basic psychological tools that individuals use at various times to manage life’s crises. These mechanisms may also be referred to as ego defenses, defense mechanisms, or protective mechanisms. As such they defend the ego or self from untoward anxiety, help resolve conflicts, and return the individual to a point of psychological homeostasis or comfort. These mechanisms are usually outside conscious awareness and are not considered pathological in and of themselves; they should not be removed or challenged until the individual is ready and has adequate strength to tolerate the stressful situation. Common defense mechanisms are listed in Table 6-3.
Table 6-3
| Defense Mechanism | Example |
| Compensation: process by which a person makes up for a perceived deficiency by strongly emphasizing a feature that he or she regards as an asset | A businessman perceives his small physical stature negatively. He tries to overcome this by being aggressive, forceful, and controlling in business dealings. |
| Denial: avoidance of disagreeable realties by ignoring or refusing to recognize them; probably the simplest and most primitive of all defense mechanisms | Mrs. P has just been told that her breast biopsy indicates a malignancy. When her husband visits her that evening, she tells him that no one has discussed the laboratory results with her. |
| Displacement: shift of emotion from a person or object to another, usually neutral or less dangerous, person or object | A 4-year-old boy is angry because his mother just punished him for drawing on his bedroom walls. He begins to play war with his soldier toys and has them battle and fight with each other. |
| Dissociation: the separation of any group of mental or behavioral processes from the rest of the person’s consciousness or identity | A man is brought to the emergency department by the police and is unable to explain who he is and where he lives or works. |
| Identification: process by which a person tries to become like someone he or she admires by taking on thoughts, mannerisms, or tastes of that individual | Sally, 15 years old, has her hair styled similarly to that of her young English teacher whom she admires. |
| Intellectualization: excessive reasoning or logic used to avoid experiencing disturbing feelings | A woman avoids dealing with her anxiety in shopping malls by explaining that she is not engaging in the frivolous waste of time and money by not going into them. |
| Introjection: intense type of identification in which a person incorporates qualities or values of another person or group into his or her own ego structure; one of the earliest mechanisms of the child and is important in formation of conscience | Eight-year-old Jimmy tells his 3-year-old sister, “don’t scribble in your book of nursery rhymes. Just look at the pretty pictures,” thus expressing his parents’ values to his little sister. |
| Isolation: splitting off of emotional components of a thought, which may be temporary or long term | A second-year medical student dissects a cadaver for her anatomy course without being disturbed by thoughts of death. |
| Projection: attributing one’s thoughts or impulses to another person; through this process one can attribute intolerable wishes, emotional feelings, or motivations to another person | A young woman who denies that she has sexual feelings about a co-worker accuses him without basis of being a “flirt” and says he is trying to seduce her. |
| Rationalization: offering a socially acceptable or apparently logical explanation to justify or make acceptable otherwise unacceptable impulse, feelings, behaviors, and motives | John fails an examination and complains that the lectures were not well organized or clearly presented. |
| Reaction formation: development of conscious attitudes and behavior patterns that are opposite to what one really feels or would like to do | A married woman who feels attracted to one of her husband’s friends treats him rudely. |
| Regression: retreat in face of stress to behavior characteristic of any earlier level of development | Four-year-old Nicole, who has been toilet trained for more than a year, begins to wet her pants again when her new baby brother is brought home from the hospital. |
| Repression: involuntary exclusion of a painful or conflictual thought, impulse, or memory from awareness; the primary ego defense, and other mechanisms tend to reinforce it | Mr. R does not recall hitting his wife when she was pregnant. |
| Splitting: viewing people and situations as either all good or all bad; failure to integrate the positive and negative qualities of oneself | A friend tells you that you are the most wonderful person in the world one day and how much she hates you the next day. |
| Sublimation: acceptance of a socially approved substitute goal for a drive whose normal channel of expression is blocked | Ed has an impulsive and physically aggressive nature. He tries out for the football team and becomes a star tackle. |
| Suppression: a process often listed as a defense mechanism but really a conscious counterpart of repression; intentional exclusion of material from consciousness | A young man at work finds that he is thinking so much about his date that evening that it is interfering with his work. He decides to put it out of his mind until he leaves the office for the day. |
| Undoing: act or communication that partially negates a previous one; primitive defense mechanism | Larry makes a passionate declaration of love to Sue on a date. On their next meeting, he treats her formally and distantly. |
Modified from Stuart GW, Laraia MT: Principles and practice of psychiatric nursing, ed 9, St Louis, 2009, Mosby.
ANXIETY DISTURBANCES AND RESOURCES
ANXIETY
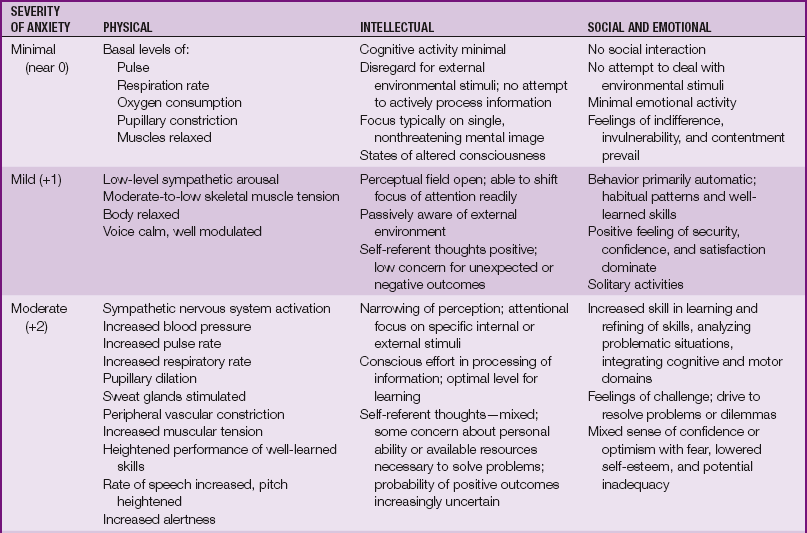
A Definition: a state of alertness or apprehension, tension or uneasiness; a major component of many mental disturbances. Anxiety is an internal state that the individual experiences when a perceived threat to the physical body or the psychological integrity of the person exists. It interferes with concentration, focusing attention on the perceived threat. In its mild form anxiety serves to alert the person to danger and prepare the body to react to danger; in its severe form it is debilitating and may immobilize the person and interfere with activities. Anxiety is usually described in degrees or levels.
1. Adaptive coping: The problem creating the anxiety is resolved.
2. Palliative coping: The problem creating the anxiety is not resolved but rather temporarily reduced; the problem can return at a later date.
3. Maladaptive coping: Energy is channeled toward reducing the anxiety, and no effort is made to solve the problem.
4. Dysfunctional coping: The problem is not solved, and the anxiety not reduced.
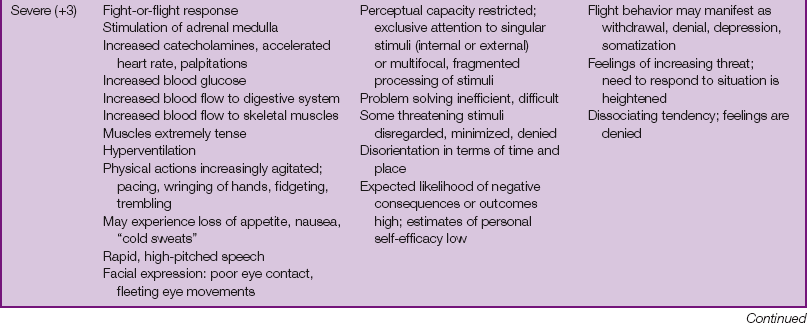
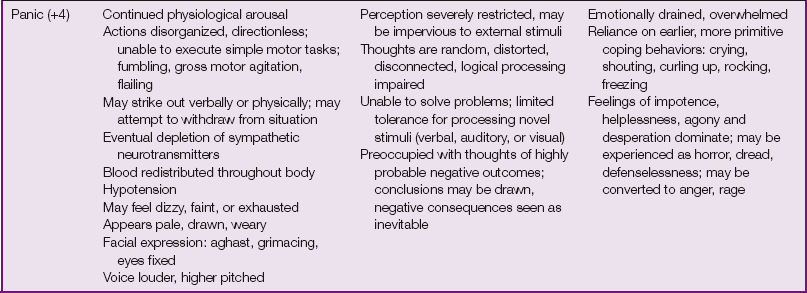
C Levels of anxiety (Table 6-4)
1. Remain with the highly anxious patient; leaving him or her alone increases anxiety.
2. Maintain a calm milieu, which reduces stimuli.
3. Remain in control and calm; patient fears losing control and needs to feel secure.
4. Communicate with clear, simple, short sentences because patient’s ability to deal with complex, abstract statements is compromised. Similarly, ask questions requiring brief, concise responses.
5. Use of as-necessary (pro re nata [p.r.n.]) medications may be needed to decrease patient anxiety to a manageable level (e.g., benzodiazepines, such as lorazepam [Ativan] or alprazolam [Xanax]).
6. Encourage use of relaxation and other stress-reduction techniques, such as guided imagery or deep-breathing exercises.
7. When appropriate, assist patient with recognizing early signs of anxiety and developing effective ways to prevent its escalation.
8. Provide opportunities for discussing the relationship of thoughts and emotions to anxiety.
9. More restrictive interventions such as seclusion, restraints, or both may be necessary if patient is a danger to self or others.
PHOBIAS
A Definition: irrational, continual fears of an activity, situation, object, or event that are obsessive
B Types (examples, not inclusive)
1. Agoraphobia (literal meaning: fear of the marketplace) without panic attacks: fear of being away from a safe environment or person from which escape may not be readily available
2. Social phobia: irrational fear of exposure to the scrutiny of others
3. Simple or specific phobia: disabling fear of some specific object or situation such as the fear of animals (zoophobia) or of being in a high place (acrophobia)
1. History and physical examination, including family history
2. Panic or anticipatory anxiety or both
3. Recognition of phobia as irrational
4. Defense mechanisms of displacement and repression
6. Interference with demands of daily activities
1. Accept patient and his or her fears.
2. Encourage involvement in activities that do not increase anxiety.
3. Help patient recognize that his or her behavior is an attempt to cope with anxiety.
4. Use a calm, nonauthoritative approach.
5. Reassure patient that he or she will not be made to confront the phobia in treatment until ready to do so.
OBSESSIVE-COMPULSIVE DISORDER (OCD)
A Definition: obsessive thoughts (troublesome, persistent thoughts) usually triggered by anxiety and compulsions (ritualistic behaviors) that are repetitive and represent an attempt to reduce anxiety
1. Compulsive, ritualistic behavior
3. Alterations in normal functioning
6. Suicidal thoughts or feelings
7. Rumination (preoccupation with specific thoughts)
1. Always follow patient’s behavioral support and modification plan regarding the behavioral rituals exhibited.
2. If permitted by the plan, allow patient time to perform rituals. Limit but do not interrupt the compulsive act because it may increase anxiety.
3. Ensure that basic daily needs are met.
4. Redirect rumination positively.
5. Do not initially call attention to or interfere with the compulsive act.
6. Demonstrate concern for and interest in the patient.
7. Encourage verbalization of concerns and feelings.
8. As anxiety decreases and patient feels comfortable talking with the staff, encourage him or her to talk about his or her behavior and thoughts.
9. Encourage patient to try to reduce the frequency of compulsive behavior.
10. Observe patient response to ordered medications such as antianxiety or antidepressant agents.
PERCEPTION
A Definition: awareness acquired through the five senses
B Alterations: thought to be pathological conditions resulting from anxiety
1. Illusion: an actual stimulus in the environment that is misinterpreted or misperceived
2. Hallucination: a sensation without an external stimulus; it may be:
a. Auditory: hearing nonexistent voices or sounds.
b. Olfactory: smelling nonexistent odors or aromas.
c. Visual: seeing nonexistent things, people, or animals.
d. Tactile: feeling somatic sensations.
3. Delusion: false belief, not based in fact, that cannot be changed by reasoning
C Ideas of reference: feeling that certain events or words have special meaning for self
THOUGHT DISORDERS
1. Disorganized: includes frequent incoherence, nonsystematic delusions, and inappropriate affect
2. Catatonic: includes stupor, negativity, rigidity, excitement, and posturing
3. Paranoid: includes persecutory delusions, grandiosity, delusional jealousy, and hallucinations; may include aggressive, argumentative, or hostile behaviors
4. Undifferentiated: does not fit criteria of other categories or combines them; delusions, hallucinations, or both are prominent
5. Residual: presence of residual symptoms (e.g., marked social isolation, inappropriate affect, odd beliefs) without delusions, hallucinations, or gross disorganization of thought
1. History and physical, including family history
2. Delusions of being controlled
3. Somatic delusions (grandiosity, religious, or nihilistic)
4. Persecutory delusions accompanied by hallucinations
5. Auditory hallucinations of a running commentary on behavior or thought
6. Auditory hallucination on several occasions with content of more than one word
7. Incoherence, looseness of association, illogical thinking with a deterioration in function
3. Do not enter into patient’s delusions; maintain own view of reality without demeaning patient’s view of reality. This is done by letting patient know that what he or she is experiencing is real to him or her but that you are not experiencing it.
4. Do not argue about hallucinations; the patient views them as real.
5. Offer reassurance: most patients are experiencing pain and fear from their symptoms.
6. Touch only with permission; the thought-disordered patient may have a distorted sense of his or her own person and may easily misinterpret the actions of others.
7. If you are afraid, be aware that the patient senses this; be sure that you have sufficient backup for your own safety and comfort.
8. Maintain patient safety; reassess frequently for potential for harm to self or others.
9. Medicate as ordered. Observe patient for therapeutic effect and side effects (e.g., extrapyramidal symptoms [EPSs], or neuroleptic malignant syndrome); see Chapter 3.
AFFECTIVE DISORDERS
DEPRESSIVE DISORDERS
A Major depression is the predominant mental illness in the United States and Canada, with ranges from 7% to 12% in the male population and 26% to 30% in the female population.
1. History and physical examination, including family history, to rule out medical causes contributing to patient’s condition
2. Persistent sadness, hopelessness, or tearfulness
3. Loss of interest in some or all usual activities (anhedonia), fatigue, inability to concentrate
4. Change in appetite: usually decreased
5. Changes in weight: usually a loss in weight
6. Sleep disturbances: usually insomnia but may be sleeping more during the day
7. Withdrawal from family and friends; feeling guilty and unworthy
8. Hopelessness and helplessness that may become profound and lead to delusions or fantasies of ending it all
9. If left in this pattern, patient eventually might justify how nonexistence may solve the problems.
10. Patient may start to dwell on death and devise a plan of self-destruction.
11. Self-destruction becomes the goal; this is suicidal ideation.
C See discussion of suicide prevention and suicide intervention.
BIPOLAR DISORDERS
A Category used when one or more manic episodes are noted, whether or not a depressive episode is or has been experienced
B Mania characterized by unstable, elevated, or irritable mood; pressured speech; irritability; and increased motor activity. Patient often displays racing thoughts, impulsivity, attention-seeking or agitated behavior, psychosis, and alterations in sleep.
1. Demonstrate sincere interest.
2. Accept patient’s feelings. Anger may be directed at the nearest safe object, often the nurse, and should not be taken personally.
3. Allow patient to express feelings (e.g., crying) in a dignified environment.
4. Be aware of patient’s limited ability to control his or her behavior, and encourage expression of feelings (e.g., crying) only within a safe context.
5. If patient is overactive, limit-setting or reduction of stimuli may be necessary to allow him or her to regain self-control and increase focus.
6. Avoid power struggles: use force only if necessary to protect patient or others in the environment.
EATING DISORDERS
A Obesity and compulsive overeating: consuming more than the required number of calories, which results in weight gain; not burning as many calories as consumed. The person is usually considered obese when weight is 20% more than is recommended for his or her height.
B Anorexia nervosa: an eating disorder characterized by refusal to maintain a minimally normal body weight. It is most often seen in adolescent women (may occur with bulimia or separately).
C Bulimia: an eating disorder characterized by episodes of binging and then purging. Person may not appear overweight or underweight. With nonpurging bulimia the person uses laxatives, diuretics, fasting, or exercise to control his or her weight. Bulimia often leads to other symptoms such as menstrual irregularities, gastric dilation, aspiration pneumonia, dental caries (caused by frequent vomiting), and esophagitis.
D Interventions: Treatment of these disorders will vary; however, it is centered around the following goals:
PERSONALITY DISORDERS
A The American Psychiatric Association in its DSM-5 classifies personality disorders as follows:
1. Eccentric Personality Disorders
a. Paranoid Personality Disorder: characterized by suspicion, rigidity, secretiveness, oversensitivity and alertness, distortions of reality, and the use of projection as a major defense mechanism
b. Schizoid: limited emotional expression, distant, seemingly detached in social situation and interactions
c. Schizotypal: often considered strange because of behaviors, appearance, excessive anxiety, illogical or confused speech, odd beliefs and ideas of reference; prefer to be alone and avoid social interactions
2. Erratic Personality Disorders
a. Antisocial Personality Disorder: characterized by lack of remorse and willingness to exploit others for personal gains; use dishonest methods and tactics to achieve desired outcomes; disregard rights of others, laws, and social norms but expect others to conform to the same; persist in dishonest and unlawful behaviors without regret, remorse, or concern for their victims; can be charming, clever, and entertaining in their efforts to deceive
b. Borderline Personality Disorder: at times moderately neurotic; at other times overtly psychotic; extremely difficult to treat and often unstable after numerous treatment attempts; lack emotional control and the ability to form and maintain relationships with others; can engage in self-injurious behaviors (SIBs) and suicidal gestures when fearful of separation or rejection; social relationships characterized by highs and lows (love and hate), which drives away those with whom they desire relationships; split staff by allegations and manipulation
c. Histrionic Personality Disorder: have highly emotional responses, short attention spans; are superficial, lack depth; seek attention, affection, and approval of others.
d. Narcissistic Personality Disorder: seek approval and admiration of others and use attention-seeking behaviors; demonstrate little empathy and can be grandiose; see themselves as special, deserving of special consideration; demonstrate a sense of entitlement and seem arrogant
3. Fearful/Anxious Personality Disorders
a. Avoidant Personality Disorder: fear rejection; avoid social relationships, yet desire the closeness they avoid out of fear; see themselves as social misfits, uninteresting, and less acceptable than others; can also be depressed and anxious and dwell on health concerns
b. Dependent Personality Disorder: fear separation and being left alone because they believe that they cannot survive alone; have a clinging manner, seek others to care for day-to-day matters, avoid personal responsibility and submit to others in most matters; tolerate unhappy and even abusive relationships in an effort to prevent separation; disorder often found in individuals who are disabled or have ongoing medical conditions
c. Obsessive-Compulsive Personality Disorder: fear uncertainty, lack of total control, disorder, unpredictability and delegation; are focused on rules, regulations, procedures, lists, and organization; are devoted to tasks, work, and process, but drive for perfection prevents accomplishment; personal relationships can be superficial and controlled in spite of real affection for others
2. Help patient increase coping skills.
3. These patients are often manipulative and attention seeking, requiring a firm, consistent response by staff. Limit-setting is very important here.
4. They tend to view people or situations in extremes such as all good or all bad.
5. Patients need to begin developing meaningful relationships in which they can begin to trust.
6. Consistency is important; patients may split the staff to play one staff member against another.
7. Patients need to take responsibility for their behaviors and the consequences of these behaviors.
C Codependency: meeting goals successfully by relying on another person for the answers. Characteristics of the codependent person include the following:
1. Partners are dependent on each other to make a whole relationship.
2. One of the partners in this relationship assumes a passive role.
3. One or both may have low self-esteem.
4. One or both may have poor self-image.
5. One or both may have an addictive disorder (e.g., alcohol, drugs).
6. They tend to be manipulative—a constant conflict exists, either between them or within the family.
7. They tend to operate in a series of delusions.
8. Because of delusions, they tend to promote their version of any story as the absolute truth.
9. They exhibit poor boundaries (limits) in relationships.
10. They are somewhat to totally insensitive to others’ emotions and feelings.
11. If the codependency exists within a family, it is highly likely that a dysfunctional family unit will emerge and the children will become part of the codependency.
12. Codependency may be generational and therefore cyclical.
13. In helping the dependent individual, the codependent can become an enabler—especially by helping a chemically dependent person escape the consequences of his or her addiction.
14. The treatment of codependent people is designed to identify the underlying emotions that are fostering the codependency.
D Substance abuse disorders: pattern of pathological use of substances that entails factors such as the need for daily use, loss of control, efforts to control use, overdoses, impairment of social functioning, family disruptions, and legal problems. Abuse is distinguished from dependency by tolerance of the substance (increasing use requires increasing doses to achieve the same effect) and the presence or absence of a withdrawal syndrome.
a. Abuse is distinguished from recreational use by features such as daily drinking; frequent need for the chemical; blackouts; social impairment; and evidence of decreased ability to function, such as job loss, driving while intoxicated, and arrests.
b. A pattern of acute alcohol ingestion may result in a condition formerly known as delirium tremens (DTs), now known as acute alcohol withdrawal syndrome; key features are hallucinations, extreme agitation, and disorientation; treatment includes anxiolytics (benzodiazepines), anticonvulsants, and hydration.
c. Long-term use may lead to peripheral neuropathy; Wernicke syndrome (confusion, ataxia, abnormal eye movements); or Korsakoff syndrome (alcoholic amnesia syndrome), which manifests with memory loss and confabulation. Confabulation can be the primary component. These effects are largely caused by deficiency of thiamine and may be partially reversed by provision of thiamine. Korsakoff syndrome is usually irreversible but may be arrested by thiamine replacement therapy and cessation of alcohol abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree