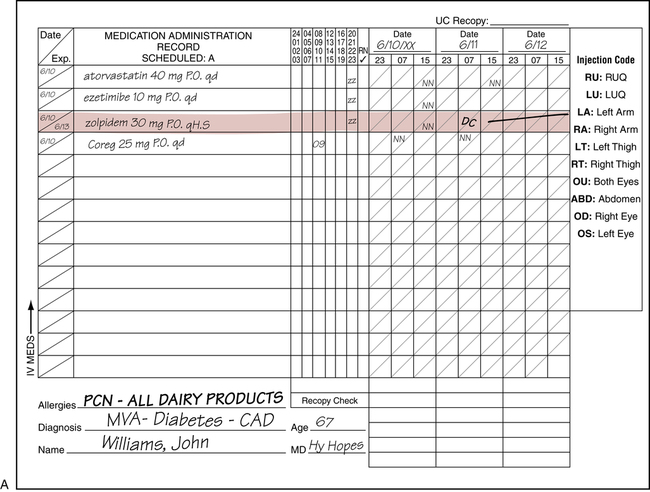
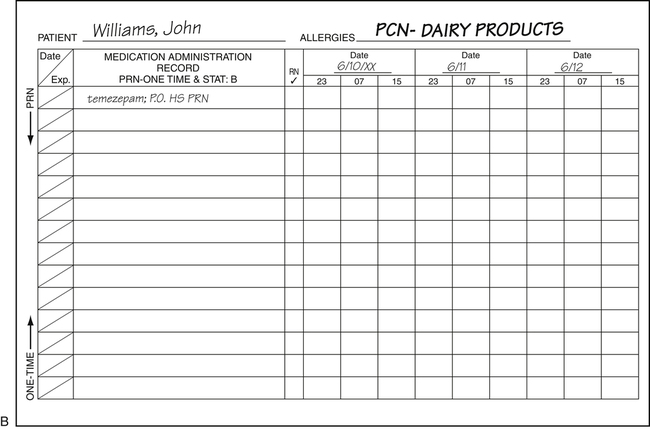
On completion of this chapter, you will be able to: 1. Define the terms in the vocabulary list. 2. Write the meaning of the abbreviations in the abbreviations list. 3. Identify at least four causes of medication errors, and explain how the use of computer physician order entry (CPOE) with clinical decision support systems (CDSS) decreases the risk of errors. 4. Compare the health unit coordinator (HUC) roles regarding medication orders with and without electronic medical records (EMRs) with CPOE. 5. Discuss two types of medicine carts and their use, and identify two medications that would be found in the medication stock supply. 6. Discuss the use of the medication administration record (MAR) when EMRs are used and when paper charts are used. 7. List the five components of a medication order. 8. List at least four routes by which medications may be administered. 9. Describe the general purpose for provided drug groups. 10. Identify four categories of medications that are controlled substances. 11. Explain the importance of notifying the pharmacy of changes or pending changes to a patient’s total parenteral nutrition (TPN) orders. 12. Define standing, prn, one-time, short-series, and stat medication orders. 13. Name three common skin tests performed, and explain the purpose of each. 14. Discuss how medications are renewed, discontinued, and changed when the EMR is used and when paper charts are used. The result of adding a medication to a bag of intravenous solution. Injuries or harmful reactions that result from the use of a drug. Drug Enforcement Administration (DEA) Food and Drug Administration (FDA) Injection of a substance between the layers of the skin (used for skin tests). Injection of medication directly into the muscle. Administration of a substance directly into a vein. Intravenous or IV Piggyback (IVPB) Method of giving concentrated doses of medication directly into the vein. Medication Administration Record (MAR) Controlled drug that relieves pain or produces sleep. Patient-Controlled Analgesia (PCA) Agents given to reduce or relive anxiety, stress, or excitement. Agents given to induce sleep and to relieve anxiety. Subcutaneous Injection (sq or sub-q) Injection of a small amount of a medication under the skin into fatty or connective tissue. Direct application of medication to the skin, eye, ear, or other parts of the body. See Table 10-1 for a list of incorrect and correct abbreviations, as approved by The Joint Commission (TJC). Some hospitals have additional abbreviations to avoid using, such as those listed in Table 13-1. TABLE 13-1 A Hospital’s List of Additional Abbreviations to Avoid Health unit coordinators (HUCs) working in hospitals that have implemented an EMR system with CPOE no longer have the responsibility of interpreting doctors’ handwritten medication orders. It is, however, beneficial that the HUC recognize medication orders. The HUC will still have some responsibilities involving medications, such as ordering stock medications for the nursing unit and printing required computerized medication pamphlets prior to a patient’s discharge. The HUC may also be required to include some types of medications on requisitions (such as anticonvulsants for a neurodiagnostics test). The goal is for all hospitals to have EMR with CPOE in 2014, but as of 2012 most hospitals do not have electronic prescription systems (stand-alone or as part of an EMR program) in use. Electronic prescription systems are costly and difficult to integrate into the sometimes chaotic hospital structure. The HUC is still transcribing medication orders in many hospitals. Transcription of medication orders will vary among hospitals and may involve writing ordered medications on the patient’s paper medication administration record (MAR) or entering medications into the patient’s computerized MAR. (Review transcription of medication orders in Chapter 9.) Medications are usually stored in a medicine cart that is prepared by the pharmacy and sent to the units daily. Use of medication carts reduces the risk of mislabeled medications, ensuring that regulations of the Food and Drug Administration (FDA) are met. Two types of medication carts are used. One is a unit dose medicine cart that contains “unit doses” in separate drawers or bins specifically labeled for each patient as ordered by the doctor(s). The pharmacist fills these orders by reading the computerized orders written by the physician, or by reading a hard or faxed copy of the physician’s orders. The unit dose medication cart can be wheeled to the patient’s bedside for administration of the medication (Fig. 13-1). The second type is a computerized medication cart such as a Pyxis that requires the nurse to enter a confidential user identification (ID) and password to unlock the cart. The nurse always verifies the name of the medication, the dose, and the patient’s name before removing the medication. The computerized medication carts remain in the medication room and are not taken from room to room. Some hospitals lock intravenous (IV) solutions in a storage cabinet that is located next to the computerized medication cart, and both can be opened only when a nurse enters an assigned code (Fig. 13-2). All medications and/or IV solutions that are removed can be tracked on the computer by the code entered at the time of removal. When a computerized medication cart is used, the pharmacist enters the instructions for each patient’s medications into the cart (usually for a 24-hour period). The medication administration record (MAR), as described in Chapter 8, is a form on which nursing personnel record all medications given to the patient; it is a permanent part of the patient’s chart (electronic or paper). Nurses use the MAR as a reference while preparing medications for administration (if medication carts are not used) and while administering medications. The nurse signs the MAR electronically (when the EMR is used) or manually (when paper charts are used) at the bottom of the form at the end of each shift to indicate that the patient received the medications as charted or did not receive any medications if none were ordered. Currently, three methods of completing MARs are used. A handwritten MAR is used when CPOE or the printed MAR initiated by the pharmacy has not been implemented. Transcribing of medication orders may require the HUC to write the order on the MAR. In some hospitals, nurses are responsible for writing their assigned patients’ medication orders on the MAR. Accuracy in copying the medication order from the physician’s order sheet onto the MAR is absolutely essential. The HUC initiates the record on the patient’s admission. The record varies in the number of days (3 to 10 days) that medications may be entered. When the last date of the dated period on the MAR has been reached, a new record with new dates is prepared, and all medications still in use are copied onto the new form. Handwritten MARs are also a permanent part of the patient’s chart. The MAR is a legal document, so entries are required to be written in ink (usually black) (Fig. 13-3). To discontinue medications on the MAR, indicate “DC” on the correct day and time, and draw a line through the days the medication will not be given. A yellow or pink highlight is usually drawn over the medication entry that is discontinued (see Fig. 13-3, A).
Medication Orders
Abbreviation
Meaning
Example of Usage on a Doctor’s Order Sheet
ADE
adverse drug event
[ADEs are common and costly]
ASA
acetylsalicylic acid or aspirin
ASA 81 mg PO q day
BCOC or LOC
bowel care of choice or laxative of choice
BCOC as per patient request
LOC as per patient request
BS
bedside
NTG 0.4 mg subling prn, keep @ BS
cc
(same as “mL” and may not be allowed in some facilities, as it may be confused with “U” or “u” if poorly written)
cubic centimeters
MOM 30cc po prn
G, gm, or g
gram
cefadroxil 1 g IVPB q6h
gr
grain
chloral hydrate gr XV PO hs prn
HA or H/A
headache
Tylenol 650 mg prn H/A
IM
intramuscular
vitamin B12 1000 mcg deep IM tomorrow
IV
intravenous
D/C IV if infiltrates
IVP
intravenous push
theophylline 5 mg/kg IVP now
IVPB
intravenous or IV piggyback
cephalothin 0.5 g IVPB q8h
KCl
potassium chloride
Add 40 mEq KCl to each IV
L
liter
1 L 5% D/W to run @ 125 mL/hr
mcg
microgram
vitamin B12 1000 mcg IM
mEq
milliequivalent
Give 20 mEq KCl per open heart protocol
mg
milligram
ciprofloxacin 250 mg PO q12°
mL or ml
milliliter (same as cubic centimeter)
1000 mL 5% D/W @ KO rate
noc
night
Ambien 10 mg po q noc
NTG
nitroglycerin
NTG 0.4 mg subling for heart pain prn
OTC
over-the-counter
The patient was not taking any OTC medications
oz
ounce
Add 8 oz of juice to Metamucil packet
PCA
patient-controlled analgesia
PCA morphine sulfate 2 mg q15 min
PCN
penicillin
PCN 250 mg PO q 6 hr
PO or po
per os (by mouth)
lorazepam 2 mg PO tid
Pr or R
per rectum
bisacodyl supp 10 mg pr now
prn
pro re nata (as needed)
Maalox 30 mL prn GI discomfort
sq, or sub-q
subcutaneous
heparin 5000 unit sub-q daily
subling, sl
sublingual (under tongue)
nitroglycerin tab sl prn anginal pain
supp
suppository
acetaminophen supp prn for temp ↑ 100°(R)
syr
syrup
ipecac syr 15 mL now
tinct or tr
tincture
Apply tinct of benzoin around operative site before applying tape
Abbreviation
Potential Problem
Preferred Term
IM
Because of poor writing, often misinterpreted as “IV,” causing the medication to be given via the wrong route
Write out “intramuscular”
D/C
Patient’s medications may be prematurely discontinued when D/C means “discharge” and is followed by a list of medications
Write out “discontinue”
HS
May be misinterpreted as “hour of sleep” when written as meaning “half-strength”
Write out “half-strength”
IVP
When written to mean “intravenous push,” may be mistaken for “intravenous piggyback” (IVPB)
Write out “intravenous push”
S/C or S/Q
When poorly written, often mistaken for “SL” (sublingual)
Write out “subcutaneous”
Slash mark: /
Misunderstood as the number “1” rather than the intended meaning “per”
Write out “per”
Computer Physician Order Entry and Clinical Decision Support System
Health Unit Coordinator Role Regarding Medication Orders with and without an Electronic Medical Record with Computer Physician Order Entry
Administration of Medication
Medication Carts
The Medication Administration Record
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Medication Orders
Get Clinical Tree app for offline access