chapter 5
Medical-Surgical Nursing
After studying this chapter, the student should be able to:
1 Describe the nursing care responsibilities surrounding diagnostic tests.
2 Identify signs and symptoms of common medical diagnoses.
3 Plan nursing interventions for individuals with nursing diagnoses.
4 Evaluate the effectiveness of nursing interventions for individuals with select nursing diagnoses.
5 Describe the responsibilities of the nurse regarding the patient who is undergoing surgery.
 http://evolve.elsevier.com/Mosby/comprehensivePN
http://evolve.elsevier.com/Mosby/comprehensivePN
ANATOMY AND PHYSIOLOGY: AN OVERVIEW
A Anatomy: the study of the structure of the body, its many parts, and their relationship to one another
B Physiology: the study of how the body and its many parts function
C Homeostasis: a state of constancy or dynamic equilibrium within the body
1. Anatomical position: the body is erect, with arms at sides and palms turned forward
2. Anterior: toward the front of the body
3. Posterior: toward the back of the body
6. Inferior: toward the lower aspect
9. Proximal: nearest the origin of a structure (elbows are proximal to the fingers, shoulder is proximal to the elbow)
1. Dorsal: pertaining to the back; has two subdivisions that are continuous with each other
a. Cranial: the space inside the skull; contains the brain
b. Spinal: extends from the cranial cavity nearly to the end of the vertebral column; contains the spinal cord
2. Ventral: pertaining to the front; contains structures of the chest and abdomen; has two subdivisions
STRUCTURAL UNITS
Cell
A Definition: basic unit of structure and function of all living things; made of protoplasm (meaning “original substance”), which is composed of oxygen, hydrogen, nitrogen, carbon, sulfur, and phosphorus; varies in size and shape
a. Cytoplasmic membrane: keeps cell whole and intact; allows certain substances to pass through and prevents others from entering (semipermeable membrane)
b. Cytoplasm: area in which most cellular activity occurs; the working and storage area
c. Nucleus: the control center; directs cell activity and is necessary for reproduction; the site of the genetic material, deoxyribonucleic acid (DNA)
a. Irritability: respond to stimuli
b. Growth and reproduction: get larger in size and are able to increase in number
c. Metabolism: chemical reaction consisting of:
(1) Anabolism: forming new substances to build new cell material; constructive
(2) Catabolism: breaking down of substances into simpler substances and disposing of waste; destructive
d. Contractility: the ability to shorten and thicken in response to a stimulus
e. Conductivity: ability to transfer an electrical charge or impulse
a. Movement of substances through cell membranes
(1) Diffusion: movement of dissolved particles through a semipermeable membrane from an area of high concentration of particles to an area of low concentration of particles. Diffusion continues until the particles are evenly distributed.
(2) Osmosis: movement of water through a semipermeable membrane from an area in which a large amount of water (dilute solution) exists to an area of a low concentration of water (a concentrated solution). Osmosis occurs until the water is evenly distributed.
(3) Filtration: movement of water and particles through a membrane because of a greater pushing force on one side of the membrane (hydrostatic pressure)
b. Reproduction mitosis: process of cell division; distributes identical chromosomes (DNA molecules) to each cell formed; enables cells to reproduce their own kind
Tissues
A Definition: groups of similar cells having like functions
B Classifications and functions
1. Epithelial: cells are packed closely together; contain no blood vessels; three main types:
a. Simple squamous: single layer of cells through which substances can pass; function is absorption; lines air sacs of lungs, lines blood vessels, and covers membranes that line body cavity
b. Stratified squamous: several layers of closely packed cells; protect the body against invasion of microorganisms; outer layer of skin, epidermis
c. Simple columnar: single layer of cells; lines the stomach, intestines, and respiratory tract; specializes in secreting mucus and absorption
2. Connective: cells are separated by intercellular material; located in all parts of the body; various types include areolar, adipose, bone, and cartilage; function to support and protect
3. Muscle: three types of muscle tissue
a. Skeletal or striated (voluntary): cells have striations; attach to bones; contractions are controlled voluntarily; cause movement.
b. Cardiac or striated (involuntary): cells have cross-striations; cardiac muscle cells have the inherent power of rhythmical contraction.
c. Visceral or nonstriated (smooth involuntary): cells appear smooth; help form walls of blood vessels and intestines; contractions cannot be controlled; cause movement.
4. Nerve: composed of cells called neurons; all neurons receive and conduct electrochemical impulses; important in control of the entire body.
Membranes
A Definition: thin, soft sheets of tissue that cover, line, lubricate, and anchor body parts
B Classification and functions
1. Epithelial: lubricate and protect the body against infection; two types
a. Mucous: line body cavities that open to the exterior (mouth, nose, intestinal tract, urinary tract, vaginal canal); secrete mucus, which protects against bacterial invasion
b. Serous: line cavities that do not open to the exterior; cover the lungs, stomach, and heart; secrete thin fluid that prevents friction
2. Connective: cover bone or hold body parts in place
Systems
A Definition: groups of organs that contribute to the function of the whole; they perform a more complex function than does a single organ. No system can function independently of another system.
1. Integumentary (skin): covers and protects the body; aids in fluid balance
2. Musculoskeletal: supports and allows movement; framework of the body
3. Circulatory: transports food, water, oxygen, and waste
4. Digestive: processes food and eliminates waste
5. Respiratory: supplies oxygen and eliminates carbon dioxide
7. Nervous: controls and coordinates body activities
8. Endocrine: regulates body activities
MUSCULOSKELETAL SYSTEM
ANATOMY AND PHYSIOLOGY OF THE SKELETAL SYSTEM (FIGURE 5-1)
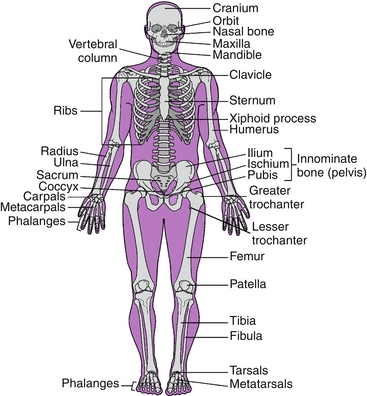
FIGURE 5-1 Bones of the body. (From Sorrentino SA, Remmert LN: Mosby’s textbook for nursing assistants, ed 8, St Louis, 2012, Mosby.)
1. Support: forms framework for body structures and provides shape
2. Protection: protects the internal organs
3. Movement: supplies levers that are activated by the contraction of an attached muscle
4. Mineral storage: stores calcium and minerals used by the body when needed
5. Produces blood cells: forms erythrocytes and thrombocytes and red marrow of bone
1. Composed of 33% organic material and 67% inorganic mineral salts
2. Collagen: organic part derived from a protein; fibrous material with a jellylike substance between the fibers; gives bone flexibility
3. Inorganic substance consists of large amount of mineral salts: calcium phosphate, calcium carbonate, calcium fluoride, magnesium phosphate, sodium oxide, and sodium chloride, which give bone its hardness and durability
1. Long bone: consists of diaphysis, epiphysis, and medullary cavity (e.g., femur)
2. Short bone: contains more spongy bone than compact; generally cube shaped (e.g., wrist bone)
3. Flat bone: thin and flat; two thin layers of compact bone with a spongy bone between them; red blood cells (RBCs) manufactured here (e.g., sternum)
4. Irregular: do not fall into preceding categories; are not symmetrical (e.g., vertebrae)
1. Long bones are similar to other bones in the body in structure, development, and function.
2. They are longer than wide and have a shaft with heads at both ends. Bones of extremities are long bones.
3. Diaphysis or shaft: hollow cylinder of hard, compact bone; contains medullary canal, which is filled with yellow bone marrow. In the adult it is primarily a storage area for adipose tissue.
4. Epiphysis: ends of the diaphysis composed of spongy bone covered by a thin layer of compact bone; contains red marrow where some RBCs are manufactured during childhood and adolescence. Erythropoietic activity in the adult occurs mainly in flat bones and vertebrae.
5. Periosteum: strong fibrous membrane that covers the bone and contains blood vessels; lymph vessels; nerves; and bone cells necessary for growth, repair, and nutrition.
6. Epiphyseal disk (flat plate made up of hyaline cartilage): allows for lengthwise growth of long bones. At puberty when growth stops, it calcifies and becomes the epiphyseal line.
7. Haversian canals: run lengthwise through bone matrix, carrying blood vessels and nerves to all areas of the bone. They nourish the osteocytes, or bone cells.
E Processes: bony prominences that serve as landmarks
1. Acromion: highest point of the shoulder
2. Olecranon: upper end of the ulna; forms the point of the elbow
3. Iliac crest: curved rim along the upper border of the ilium
4. Ischial spine: lies at the back of the pelvic outlet
5. Acetabulum: deep socket in the hip bone
6. Greater trochanter: large protuberance located at the top of the shaft of the femur
F Factors that affect bone growth and maintenance
1. Heredity: Each person has a genetic potential for height, with genes inherited from both parents
2. Nutrition: Nutrients such as calcium, phosphorus, and proteins are raw materials of which bones are made; without nutrients, bones cannot grow properly.
3. Hormones: Produced by endocrine glands, they help regulate cell division, protein synthesis, calcium metabolism, and energy production.
4. Exercise: bearing weight such as walking. Without exercise, bones become weak and fragile because of the loss of calcium.
G Joints: points at which bones meet; classification determined by the extent of movement
1. Synarthroses: Fibrous connective tissue holds joining bones close together with no movement (e.g., sutures in skull).
2. Amphiarthroses: There is slight movement (e.g., joints between the vertebrae).
3. Diarthroses: Free movement; all have a joint capsule, a joint cavity, and a layer of cartilage.
a. Ball-and-socket joint: Ball-shaped head of one bone fits into a concave socket of another bone (e.g., hip joint).
b. Hinge joint: It allows movement in only two directions, flexion and extension (e.g., knee).
c. Pivot joint: A small projection of one bone pivots in an arch of another bone (e.g., vertebrae of the neck).
d. Saddle joint: It exists only between the metacarpal bone and a carpal bone of the wrist (e.g., thumb and wrist).
e. Gliding joint: Bone surfaces slide over one another (e.g., wrist, ankle).
H Ligaments: connective tissue bands that hold bones together
I Tendons: connective tissue bands that attach bones to muscles
J Bursa: a sac or cavity filled with fluid (synovia or synovial fluid) that reduces friction at joints
ANATOMY AND PHYSIOLOGY OF THE MUSCULAR SYSTEM (FIGURE 5-2)
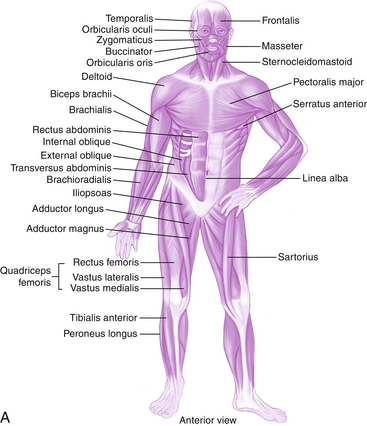
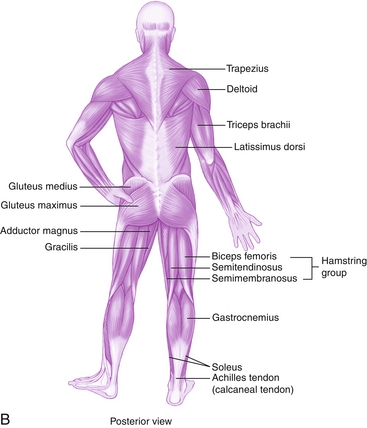
FIGURE 5-2 Major muscles of the body. A, Anterior view. B, Posterior view. (From Herlihy B: The human body in health and illness, ed 4, St Louis, 2011, Saunders.)
1. Produces movement by contraction (Table 5-1)
Table 5-1
| Muscle | Location | Function |
| Sternocleidomastoid | Neck | Flexion and rotation of head |
| Trapezius | Upper back | Helps hold head erect; also assists in moving head sideways |
| Latissimus dorsi | Lower back | Extension and adduction of upper arm |
| Pectoralis major | Chest | Flexion and abduction of upper arm |
| Deltoid | Shoulder | Adduction of upper arm |
| Biceps brachii | Anterior upper arm | Flexion of arm and forearm |
| Triceps brachii | Posterior upper arm | Extension of arm and forearm |
| Gluteus maximus | Fleshy part of hips and buttocks | Extension of thigh |
| Gluteus medius | Lateral part of hips and buttocks | Abduction of thigh when limb is extended |
| Hamstring group | Posterior thigh | Flexion of lower leg and extension of thigh |
| Quadriceps femoris | Anterior thigh | Flexion of thigh and extension of lower leg |
| Gastrocnemius | Calf of leg | Helps in extension of foot and flexion of leg |
1. Striated: skeletal, voluntary muscle; attached to bones and accounts for body movement; controlled consciously
2. Smooth: visceral, nonstriated, involuntary muscle; found in the walls of internal organs and blood vessels; works automatically
3. Cardiac: found only in the heart; striated, branched, and involuntary
1. Excitability: capacity to respond to stimulus
2. Contractility: ability to shorten and thicken in response to a stimulus
3. Extensibility: ability to stretch
4. Elasticity: ability to regain original size and shape
1. Muscles move bones by pulling on them; as muscle contracts, it pulls insertion bone toward its original bone.
2. Several muscles contract at the same time to produce movement.
a. Agonist: prime mover; responsible mainly for producing movement
b. Antagonists: responsible for relaxing when the prime mover is contracting
3. To contract, muscle must first be stimulated by nerve impulses.
a. Subminimal stimulus: does not cause contraction
b. Minimal stimulus: does cause contraction
c. Maximal stimulus: causes all muscle fibers in muscle to contract
d. Supramaximal stimulus: strength of stimulus above maximal; no effect on strength of contraction
a. Isometric: increase the tension without causing movement
c. Tonic: do not produce movement but increase firmness of muscles that maintain posture
d. Twitch: a quick, jerky contraction
MUSCULOSKELETAL CONDITIONS AND DISORDERS
NURSING ASSESSMENT
A Observation (objective data)
a. Comparison of affected and unaffected sides
b. Limited ability or loss of ability to move body part
c. Diminished muscle strength to passive resistance
d. Limited range of motion (ROM)
e. Degree of ability to perform activities of daily living (ADLs)
B Patient description (subjective data)
a. Patient’s account of location, character, frequency, duration, onset
b. May use the PQRST method of assessment
DIAGNOSTIC TESTS AND METHODS
1. Complete blood count (CBC): an aid in determining anemia or the presence of infection
2. Erythrocyte sedimentation rate (ESR): if elevated, evidence of an inflammatory process
3. Rheumatoid factor: protein found in the blood of most people with rheumatoid arthritis
4. Uric acid: high concentration found in persons who have gout
5. Lupus erythematosus (LE) cell
1. Roentgenogram (x-ray): film to determine the presence of a deformity, fracture, or tumor of the skeletal system
2. Aspiration: withdrawal of fluid from a joint to obtain a specimen for diagnostic purposes
3. Bone biopsy: removal and examination of bone tissue
4. Bone scan: isotope imaging of the skeleton
5. Computed tomography (CT): use of roentgen rays to obtain accurate images of thin cross-sections of the body
6. Magnetic resonance imaging (MRI): aids in diagnosing musculoskeletal conditions through the clear differentiation of various types of tissue such as bones, fat, and muscle; nursing care includes removal of metal jewelry and assessing for metal implants
7. Arthroscopy: endoscopic examination that allows for direct visualization of a joint
8. Electromyography (EMG): used to evaluate nerve conduction in skeletal muscle
9. Positron emission tomography (PET): using an isotope, scans the brain for evaluation of structure function
10. Myelogram: x-ray examination of the spinal cord after injection with radiopaque dye (important to inquire about any known allergies to dyes)
C Nursing interventions after a myelogram
1. After procedure, patient must remain flat in bed for 8 to 12 hours before resumption of usual activities.
2. Encourage fluids to 2000 to 3000 mL every 24 hours.
3. Observe for alterations in normal motor and sensory states.
4. Observe for nausea and vomiting.
5. Administer medication as ordered by physician should patient complain of headache after the procedure.
FREQUENT PATIENT PROBLEMS AND NURSING CARE
A Disturbed body image related to immobility
1. Provide atmosphere of acceptance; be an active listener
2. Express empathy, warmth, and friendliness.
3. Encourage acceptance of self-limitations.
B Impaired skin integrity: potential breakdown related to immobility and assistive devices
1. Change patient’s position frequently (usually every 2 hours).
2. Keep the skin clean, dry, and lubricated.
4. Provide sheepskin, polyurethane foam padding, or alternating pressure mattress when appropriate.
C Risk for injury: joint contracture related to incorrect body alignment
1. Place hands, feet, and knees in the natural position of function.
2. Provide devices to protect against poor alignment of body part.
3. Assist in performing active and passive ROM exercises.
4. Provide trapeze over patient’s bed.
5. Avoid pillows under knee or any prolonged pressure on popliteal space.
D Ineffective airway clearance related to increased secretions resulting from immobility
1. Change patient’s position frequently (usually every 2 hours).
2. Encourage coughing and deep breathing and use of incentive spirometer if provided.
3. Observe for coughing, fever, and green-yellow sputum.
E Ineffective tissue perfusion: potential for thrombi and emboli related to impaired physical mobility or edema
1. Inquire about history of deep vein thrombosis (DVT), other varicosities.
2. Encourage patient to move lower extremities.
3. Encourage adequate hydration.
4. Avoid use of pillows under knee.
5. To avoid release of emboli, never rub legs.
6. Encourage use of antiembolism stockings.
F Acute pain related to bone fracture or disease
1. Inspect and palpate the painful site, looking for inflammation, edema, bruising, tenderness, and skin warmth; do not rub site, to avoid causing emboli.
2. Support the affected body part.
3. Apply warm, moist compress to affected body part where prescribed. Use ice for injuries within the first 24 to 48 hours.
5. Evaluate effectiveness of pain relief measures.
6. Patient teaching for early recognition and reporting of discomfort or pain.
G Impaired physical mobility related to cast or traction confinement, joint pain, stiffness, or inflammation
1. Explain the reason for and intended effect of ROM exercises.
2. Have patient maintain body alignment.
3. Provide total exercising of muscles and joints unless severe pain or inflammation is present. Movement is contraindicated if recent surgery was performed on or near the joint.
1. Massage the area around the cast except for leg casts.
3. Elevate extremity to reduce swelling.
4. Inspect the skin for irritation.
5. Observe for cyanosis and assess capillary refill times of the extremity in a cast.
6. Observe for complaints of numbness and tingling of the extremity in a cast.
I Self-care deficits (feeding, bathing, hygiene) related to impaired physical mobility
MAJOR MEDICAL DIAGNOSES
Rheumatoid Arthritis
A Definition: chronic, systemic disease in which inflammatory changes occur throughout the connective tissue in the body, destroying joints internally. Joints most involved are hands, wrists, elbows, knees, and ankles.
B Pathology: cause is unknown. Related theories include autoimmune causes, microorganisms, viruses, and genetic predisposition.
D Diagnostic tests and methods
2. Slightly elevated white blood cell (WBC) count
3. Presence of serum rheumatoid factors
5. X-ray film to reveal joint deformity
1. Antiinflammatory agents, analgesics, corticosteroids, gold salts, antineoplastics (methotrexate), immunosuppressive drugs
2. Heat applications such as paraffin dip, hot packs, and warm tub baths or showers for analgesia or muscle relaxation
3. Surgical intervention to prevent deformities or remove damaged joints
1. Provide undisturbed periods of rest—should receive 8 to 10 hours of sleep per night with frequent naps during the day.
2. Use firm mattress, footboards, splints, and sandbags to maintain proper body alignment.
3. Encourage self-performance activities such as combing hair, feeding self, and brushing teeth. Provide assistive devices for improving hand grasp and participation in ADLs as per occupational therapy.
4. Assist with ROM exercises within limits of pain tolerance.
Osteoarthritis (Degenerative Joint Disease)
A Definition: local joint disorder affecting weight-bearing joints (hips, knees); results in disintegration of the cartilage covering the ends of bones
B Pathology: cause is unknown; predisposing factors include aging, joint trauma, and obesity
D Diagnostic tests: X-ray studies reveal joint abnormalities.
1. Weight reduction to relieve strain
2. Heat and massage for aching and stiffness
3. Physical therapy to maintain optimum level of functioning
5. Surgical intervention to prevent deformity, relieve inflammation, delay progression, or replace affected joint
Gouty Arthritis (Gout)
A Definition: disorder in which excessive amounts of uric acid are retained in the blood
1. Cause is related to a disorder of purine metabolism.
2. Uric acid crystals are deposited in the joints and cartilage and form calculi (tophi).
3. Deposits cause local irritation and an inflammatory response; big toe most common site.
4. Men older than 30 years of age are most commonly affected.
D Diagnostic tests and methods
1. Dietary restriction of foods high in purine such as organ meats
2. Uricosuric drugs to increase uric acid excretion; allopurinol to inhibit uric acid formation
3. Weight loss and periodic blood glucose screening because a relationship may exist between gouty arthritis and insulin resistance
4. Colchicine to reduce pain and relieve swelling
5. Alkaline ash diet to increase urinary pH (includes foods that reduce to an alkaline ash such as milk, cheese, cream)
1. Instruct patient to avoid foods high in purine content.
2. Encourage physical activity to promote optimal muscular and skeletal function.
3. Use bed cradle (or tent sheets over side rails) to prevent pressure of linen on feet and legs.
4. Encourage fluid intake of 2000 to 3000 mL daily to avoid renal calculi unless contraindicated.
5. Instruct patient to limit alcohol intake, which may precipitate an acute attack.
6. Instruct patient to avoid salicylates because of antagonistic actions of uricosuric drugs.
Systemic Lupus Erythematosus
A Definition: chronic multisystem inflammatory disorder involving the connective tissues such as the muscles, kidneys, heart, and serous membranes; may affect the skin, lungs, and nervous system
1. Cause is unknown; it is believed to be an autoimmune disorder.
2. Inflammation produces fibroid deposits and structural changes in connective tissue of organs and blood vessels.
3. It results in problems with mobility, oxygenation, and elimination.
1. Corticosteroids, analgesics, and medications for anemia
2. Hydroxychloroquine (antimalarial drug) and chemotherapy drugs indicated in some individuals
1. Provide emotional support to patient and family in coping with poor prognosis.
2. Encourage alternative activities and planned rest periods.
3. Instruct to avoid persons with infections, undue exposure to sunlight, and emotional stress, which can cause exacerbations.
4. Encourage intake of foods high in iron: liver, shellfish, leafy vegetables, and enriched breads and cereals.
5. Encourage patient to seek medical attention before conceiving.
Scleroderma (Progressive Systemic Sclerosis)
A Definition: fiberlike changes in the connective tissue throughout the body caused by collagen deposits and subsequent fibrosis
1. An insidious, chronic, progressive disorder; scleroderma usually begins in the skin.
2. Skin becomes thick and hard; fingers and toes become fixed in a position.
3. Other disorders that occur are difficulty in swallowing, impaired gastrointestinal (GI) mobility, cardiac and renal problems, and osteoporosis.
D Diagnostic tests and methods
1. Provide emotional support to patient and family in addressing physical and psychological needs.
2. Encourage moderate exercise to promote muscular and joint function.
3. Force fluids; encourage fluid intake of at least 1500 to 2500 mL/day unless contraindicated by patient’s condition.
4. Advise to avoid cold temperatures; use gloves to remove items from freezer.
6. Provide assistive devices to help with ADLs (eating, grooming).
Osteomyelitis
A Definition: bone inflammation caused by direct or indirect invasion of an organism
B Pathology: bacteria enter bloodstream through an open fracture or wound or by secondary invasion from bloodborne infection from a distant site such as bone or infected tonsils
D Diagnostic tests and methods
1. Long-term intravenous (IV) antibiotic therapy
2. Drainage from abscess with continuous irrigation of wound
1. Use strict aseptic technique when changing dressings.
2. Keep affected limb in proper alignment with pillows and sandbags.
3. Maintain drainage and secretion precautions for disposal of dressings.
4. Provide a high-calorie, high-protein diet and adequate hydration.
5. Provide undisturbed rest periods.
Osteoporosis
A Definition: metabolic bone disorder in which bone mass is decreased. Bones become weak and brittle. Prevention is crucial; adequate calcium intake must be maintained throughout life.
1. Common in postmenopausal women, especially Caucasian and Asian individuals
2. May be caused by deficit of estrogen and androgens, prolonged immobilization, insufficient calcium intake or absorption, vitamin D deficiency, or endocrine disorder
3. Sites usually affected are vertebrae, pelvis, hip, wrist, and femur
D Diagnostic test: X-ray film reveals bone demineralization and compression of vertebrae.
1. Physical activity and exercise to prevent atrophy
2. Estrogen replacement to provide calcium balance
3. Diet high in protein and calcium
5. Support of spine with brace or corset
6. The medications alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) are bone resorption inhibitors and are used to help alleviate bone loss.
1. Encourage patient to use a walker or cane to stabilize balance when ambulating.
2. Encourage fluid intake of 2000 to 3000 mL daily, unless contraindicated, to avoid formation of renal calculi.
3. Give instruction on foods that are high in protein and calcium content.
4. Emphasize need to follow prescribed daily activity and exercise.
5. If confined to bed, give passive ROM exercises and assist with active ROM exercises.
6. Teach safety measures to protect from fractures.
7. Teach patient about relationship between sun exposure and vitamin D.
Osteogenic Sarcoma
A Definition: tumor located in the bone and composed of cells derived from connective tissue
1. Highly malignant tumor that may metastasize to the lungs
2. Affects children, adolescents, and young adults
3. Usually occurs in shaft of long bones, especially affecting the femur
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


