CHAPTER 20 Medical Emergencies
I. GENERAL STRATEGY
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
B. Analysis: Differential Nursing Diagnoses/Collaborative Problems
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC MEDICAL EMERGENCIES
A. Reye’s Syndrome
The manifestations of Reye’s syndrome are not unique to this syndrome. There is no test specific for Reye’s syndrome; therefore, the diagnosis must be one of exclusion. Signs and symptoms of Reye’s syndrome correlate with illness stages and include protracted vomiting with or without clinically significant dehydration, encephalopathy in afebrile patients with minimal or absent jaundice, and hepatomegaly in 50% of patients (Table 20-1). Some authorities postulate that antiemetics mask early symptoms, whereas others propose that antiemetics may further predispose the individual to the disease. Although it is rare, Reye’s syndrome needs to be considered in any child presenting with altered mental status and vomiting. An appropriate history should be obtained for all children presenting with symptoms similar to those of Reye’s syndrome to determine whether an inborn error of metabolism (IEM) should be considered. Diarrhea and hyperventilation may be the first signs in children younger than 2 years of age.
Table 20-1 STAGES OF REYE’S SYNDROME
| Stage | Signs and Symptoms |
|---|---|
| Stage 0 | Awake and alert |
| Stage I | |
| Stage II | Delirium, combativeness, hyperreflexia, dilated pupils with sluggish response, tachycardia, appropriate response to noxious stimuli, hepatic dysfunction, EEG abnormalities |
| Stage III | Hyperventilation, obtunded, coma, decorticate posturing, normal pupillary and oculovestibular responses, continued hepatic changes, EEG changes |
| Stage IV | Deeper coma, decerebrate rigidity, fixed and dilated pupils, loss of oculocephalic reflex, abnormal oculovestibular reflex, minimal liver dysfunction, abnormal EEG findings |
| Stage V | Seizure, flaccidity, areflexia, dilated, nonreactive pupils, apnea, isoelectric EEG findings |
| Stage VI | Patients who cannot be classified because they have been treated with medication that alters level of consciousness |
EEG, Electroencephalogram.
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
B. Gout/Pseudogout
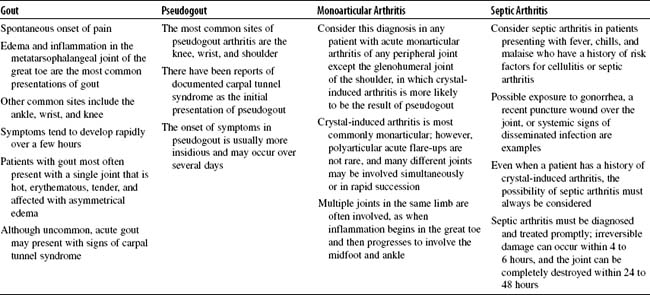
Three stages of gout occur: asymptomatic hyperuricemia, acute gout, and tophaceous gout. Nephrolithiasis may occur at any time. For gout, the male-to-female ratio is 9:1. Extra-articular deposits of MSU, known as tophi, may be seen along the Achilles tendon or on the ear helix, olecranon bursa, or prepatellar bursa. Acute monoarticular arthritis, septic arthritis, gout, and pseudogout can manifest in very similar ways (Table 20-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree