Jennifer J. Donwerth, MSN, RN, ANP-BC, GNP-BC On completion of this chapter, the reader will be able to: 1. Identify key laboratory values that increase or decrease with aging. 2. Describe the effect of aging on the erythrocyte sedimentation rate. 3. Name two medications that can interfere with potassium excretion and affect serum potassium levels. 4. Explain the relationship between serum sodium levels and pseudohyponatremia. 5. Explain the difference between serum creatinine concentrations in younger adults and older adults. 6. Explain the relationship between bacteria in the urine and urinary tract infections in older adults. 7. Relate the significance of troponin levels in diagnosing cardiac emergencies. 8. Explain the relationship of the brain natriuretic peptide to congestive heart failure. 9. Discuss the role of laboratory tests in determining thyroid function in older adults. 10. Describe the nurse’s role in interpreting laboratory values for older adults. Diagnostic testing in older adults takes on a different meaning than testing in younger adults. The nurse must realize that laboratory values can be classified into three general groups in regard to aging: (1) those that change with aging; (2) those that do not change with aging; and (3) those for which it is unclear whether aging, disease, or both change the values. Researchers are eliminating the term reference ranges as it pertains to laboratory test parameters for older adults because it can be difficult to determine whether results are a symptom of a disease or are related to normal aging (Sarkozi, 2002). The gerontologic nurse must consider the effect of laboratory and diagnostic testing on an older adult’s overall health and well-being. For example, with aging, subcutaneous tissue is decreased and the fragility of veins is increased. Consequently, a frail older adult is more likely to have increased bruising and discomfort after a venous blood drawing than a younger adult. It is also important for the nurse to know what tests have been ordered so that an explanation can be given to an anxious older adult; his or her anxiety may range from concerns about the cost of tests to a concern for privacy to cultural concerns. For example, the Chinese and Vietnamese believe that drawn blood is irreplaceable and thus may become upset with repeated blood testing (Burnside, 1988). For other cultural issues, see Chapter 5. This chapter provides the gerontologic nurse with a basic understanding of the purpose of commonly ordered laboratory and diagnostic tests, the importance of selected hematologic and blood and urine chemistry components in the body’s overall function, and the relative “normal” ranges for younger and older adults. These normal ranges may vary from institution to institution, as well as in the literature (Table 21–1). Because of the scant research conducted on older adults, geriatricians and gerontologists may also disagree as to whether changes are related to aging or disease (Beers & Berkow, 2000). When interpreting laboratory values and deciding the best course of treatment, the older adult should be viewed holistically: Signs, symptoms, and test results should all be taken into account. TABLE 21–1 Adapted from Pagana KD, Pagana TJ: Mosby’s manual of diagnostic and laboratory tests, ed 4, St Louis, 2010, Mosby; Pagana KD, Pagana TJ: Mosby’s diagnostic and laboratory test reference, ed 9, St Louis, 2009, Mosby. Blood is composed of cells (erythrocytes and leukocytes), specialized cell fragments (platelets), and a fluid matrix called plasma. The cells and cell fragments are suspended in the plasma, which is the largest component of the body’s extracellular fluid (Thibodeau & Patton, 2003). Red blood cells (RBCs), or erythrocytes, are nonnucleated biconcave disks that carry molecules of hemoglobin. The hemoglobin allows the transport and exchange of oxygen and carbon dioxide. The average life span of an erythrocyte is about 120 days. Although aging does not affect the life span of an erythrocyte, replenishment after bleeding may be delayed because of a decrease in blood-producing marrow of the long bones (McCance & Huether, 2008). RBCs are necessary for maintaining oxygen and carbon dioxide transport. A reduction in the number of circulating RBCs, a decrease in the quality or quantity of hemoglobin, and/or a decrease in the volume of packed cells (hematocrit) is classified as anemia. Anemia may be attributed to (1) impaired erythrocyte production (bone marrow disease), (2) blood loss, (3) increased erythrocyte destruction, (4) dietary problems, (5) genetic disorders, or (6) a combination of the causes (McCance & Huether, 2008). Anemia is a clinical sign, not a disease process itself. Signs of anemia may be unnoticed if the anemia is mild, or the client may experience overt symptoms such as fatigue, shortness of breath, and paresthesia (McCance & Huether, 2008). In addition, clinicians can miss signs of anemia, even in markedly anemic older clients (Ham, Sloane, & Warshaw, 2001). The combination of vague symptomatology and vague clinical presentation may lead the health care provider to attribute an older adult’s complaints to “old age” and fail to investigate adequately. The hematocrit is the percentage of total blood volume that represents erythrocytes. This is determined in the laboratory by spinning (centrifuging) a sample of blood, causing the heavier red cells to sink to the bottom of the tube while the less dense plasma rises to the top. The percentage of cells to liquid is calculated, giving the hematocrit reading. An increase in the hematocrit can signal volume depletion (Beers & Berkow, 2000). A decrease in hematocrit may be a result of disease or dietary deficiencies (Pagana & Pagana, 2003). Reported effects of aging on hemoglobin and hematocrit vary in the literature. Hemoglobin has been reported as remaining unchanged (Berghe, Wilson, & Ershler, 2004) or changing slightly, possibly from extrinsic factors rather than as a result of normal aging (Chatta & Lipschitz, 1999). Hematocrit and hemoglobin values decline slightly after the age of 90 (Sarkozi, 2002). White blood cells (WBCs), or leukocytes, are another type of cell present in the blood. Their major function is defense against foreign substances. WBCs function mainly in the interstitial fluid. Leukocytes consist of neutrophils, lymphocytes, monocytes, eosinophils, and basophils. A decrease in leukocytes in older adults may be related to drugs or severe infection (Pagana & Pagana, 2003). Drugs that can cause a decrease in leukocytes include antibiotics, anticonvulsants, antihistamines, antimetabolites, cytotoxic agents, analgesics, phenothiazines, and diuretics (Pagana & Pagana, 2004). An increase in leukocytes is generally seen with infections. However, a white cell count may be only moderately elevated in older adults when an infection, such as pneumonia, is present. Other typical symptoms of infection such as fever, pain, and enlarged lymph glands (lymphadenopathy) may be minimal or absent in older adults with infections (Mouton et al, 2001). Consequently, the nurse must be alert to other signs and symptoms of impending infection, such as the sudden onset of confusion. Pharmacologic agents have also been associated with an increase in leukocytes. These drugs include allopurinol, aspirin, heparin, steroids, and triamterene (Pagana & Pagana, 2003). Neutrophils, eosinophils, and basophils are produced in the bone marrow and possess similar structures of lobulated nuclei and many membrane-bound granules. Their primary function is phagocytosis (i.e., ingestion and destruction of particulate material). In addition, the basophil’s cytoplasmic granules contain powerful chemicals such as heparin, histamine, bradykinin, leukotrienes, and serotonin, which contribute to stimulation of the inflammatory response in tissues (McCance & Huether, 2008). The monocyte, the largest of the leukocytes, is produced in bone marrow and differs in appearance from neutrophils, eosinophils, and basophils. The monocyte has a single nucleus and is capable of destroying large bacterial organisms and virally infected cells by phagocytosis (Thibodeau & Patton, 2003). Lymphocytes, the smallest of the leukocytes, are classified into two types: B and T. The lymphocytes have a large nucleus and relatively little cytoplasm. Originating in the bone marrow and thymus, lymphocytes are housed in the lymph nodes, spleen, and tonsils. Lymphocytes do not act as phagocytes but rather produce antibodies and other specific defenses against antigens (Thibodeau & Patton, 2003). Aging does not appear to affect the function of neutrophils, although there is a reduced effect on the bone marrow to release and store these cells. Lymphocytes of older adults have shown impaired function in vitro and are suspected to be the cause of a reduction in antibody response in later life (Rothstein, 1999). There is suspicion that a decline in monocyte function exists given the increased susceptibility to infections and increased incidence of malignancies in older adults. The remaining leukocytes, eosinophils, and basophils, have not been shown to be affected by aging. The presence and function of leukocytes are necessary for the body’s resistance and response to infections, cancers, and other foreign substances. The implications for nurses related to infections and malignancies include recognizing subtle and sometimes altered responses to infections and diseases in older adults. Educating older adults about the importance of participating in cancer screenings and maintaining immunizations throughout life is essential (see Chapters 8 and 19). Folic acid is one of the eight B vitamins that make up the B-complex group. Folic acid is a water-soluble vitamin that functions as a coenzyme, which means it is inactive unless linked to an enzyme. Folic acid is necessary for the normal functioning of RBCs and WBCs. A decrease in folic acid can indicate protein-energy malnutrition, macrocytic anemia, megaloblastic anemia, and liver and renal disease. Alcohol and various other drugs are known to interfere with the absorption of folate. Some drugs have also been shown to decrease folic acid levels. These include anticonvulsants, antimalarials, and methotrexate (Pagana & Pagana, 2003). However, the effect of aging on folate is still debatable because of variance in defining the lower limits of “normal” and the different methods used to determine folate levels (Gilleece & Dexter, 2002). Because of the relationship of nutrition and alcohol consumption to folic acid levels, it is important for the gerontologic nurse to assess clients regarding their nutritional intake, including alcohol consumption habits. Elevated levels of folic acid may be seen in people with pernicious anemia, who do not have an adequate amount of B12 to metabolize folic acid. Therefore the folic acid test should be done in conjunction with assessments for vitamin B12 levels (Pagana & Pagana, 2004). Another of the water-soluble vitamins that makes up the B-complex group and acts as a coenzyme is vitamin B12, or cobalamin. Although changes in B12 levels are seen in many older adults, some scientists do not believe that aging affects the ileal absorption of B12 (Hall & Wiley, 1999). They state that problems with B12 tend to be the result of diseases and other conditions such as gastric achlorhydria, pernicious anemia, pancreatic insufficiency, and ileal disease, each of which has much greater impact on B12 absorption than aging alone (Hall & Wiley, 1999). Malabsorption of B12 can be caused by the effect of antibodies on gastric parietal cells and a decrease in intrinsic factor, the underlying cause of pernicious anemia. The prevalence of pernicious anemia increases significantly with aging (Chatta & Lipschitz, 1999). B12 is important for normal erythrocyte maturation (McCance & Huether, 2008) and acts as a coenzyme with folic acid. The synthesis of nucleic acids, and therefore the structure of deoxyribonucleic acid (DNA), depends on adequate B12 intake (Grodner, Long, & DeYoung, 2004). Vitamin B12 deficiency can lead to degeneration of the dorsal and lateral spinal columns, which in turn can lead to paresthesias of the feet and fingers and progression to spastic ataxia (Gaspard, 2002). Low B12 levels may also lead to fatigue, weakness, and altered mental status. The combination of vitamin B12, B6, and folate tends to reduce the levels of homocysteine, thereby decreasing the risk of coronary artery disease (Grodner, Long, & DeYoung, 2004). Total iron binding capacity (TIBC) measures the amount of iron and the amount of available transferrin in the serum (McCance & Huether, 2008). Transferrin is a major transport protein responsible for the transport of iron in the body. Transferrin is a protein in the plasma that collects iron and transports it to the bone marrow for incorporation into hemoglobin. Increased TIBC and transferring levels may indicate iron deficiency anemia; decreased levels may indicate anemia of chronic disease. Iron is found in the hemoglobin of the RBCs. When iron-containing foods are ingested, the iron is absorbed by the small intestine and transported to the plasma (Pagana & Pagana, 2003). Iron is necessary for controlling protein synthesis in the mitochondria and generating energy in the cells (Freedman & Sutin, 2002). Serum iron levels show progressive decreases in both genders with advancing age, although the ability to absorb iron appears to remain intact (Hall & Wiley, 1999). Iron deficiency anemia is the most common form of anemia seen in older adults. However, in spite of the decreases in serum iron levels seen with aging, anemia in older adults is not a normal consequence of aging. The gerontologic nurse should assess older adults for a lack of iron-containing foods in their diets, occult or chronic blood loss, and poor absorption of iron (Ahluwalia et al, 2004). Uric acid is a product of metabolism, specifically purine catabolism. Uric acid is excreted by the kidneys. Age-related changes in uric acid levels are significantly different between the genders. Because estrogen is thought to promote the excretion of uric acid, elevated levels are rarely seen in women before the onset of menopause (McCance & Huether, 2008). Problems with uric acid may be a result of faulty excretion (e.g., kidney failure), overproduction of uric acid, or the presence of other substances that compete for excretion sites (e.g., ketoacids) (Pagana & Pagana, 2004). Elevated uric acid levels are seen in clients with gout. Gout is a common condition in older adults involving a disturbance in the body’s control of uric acid production or excretion. Excess uric acid accumulates in the body’s fluids, especially the blood and synovial fluids, forming crystals at high concentrations. These crystals deposit in the connective tissue of the body causing painful, inflamed joints. Thiazide diuretics, caffeine, low-dose aspirin, and antiparkinsonian drugs are also a common cause of increased uric acid levels in older adults (Pagana & Pagana, 2004). Prothrombin is a plasma protein that is converted to thrombin in the first step of the clotting cascade. Clotting is necessary to prevent the loss of vital body fluids that occurs when blood vessels rupture (Thibodeau & Patton, 2003). In addition to measuring prothrombin time (PT), health care professionals also measure the effectiveness of the activity of fibrinogen and coagulation factors V, VII, and X. The results of the PT laboratory test also reveal how effectively the vitamin K–dependent coagulation factors of the extrinsic and common pathways of the coagulation cascade are performing (McCance & Huether, 2008). An increased PT is seen in liver disease, vitamin K deficiency, bile duct obstruction, and salicylate intoxication. Some medications can also cause an increase in a patient’s PT. They are allopurinol, cephalothins, cholestyramine, clofibrate, and sulfonamides (Pagana & Pagana, 2003). Pagana and Pagana (2003) also report that digitalis and diphenhydramine can cause a decreased PT level. Older adults are often prescribed the drug warfarin (Coumadin) after open-heart surgery and in cases of chronic atrial fibrillation. Warfarin interferes with the production of vitamin K–dependent coagulation factors, thereby decreasing the chance of thrombus formation. Warfarin can interact with many medications, especially those often taken by older adults, such as aspirin, quinidine, sulfa, indomethacin, and nonsteroidal antiinflammatory drugs (NSAIDs) (Pagana & Pagana, 2003). Gerontologic nurses should help clients understand the importance of keeping their appointments for PT checks and consulting their health providers before taking any medications not prescribed. The adequacy of warfarin therapy can be assessed by following a client’s PT level. The PT value is traditionally reported in seconds and includes a value called the international normalized ratio (INR). INR is a mathematic “correction” of the results of the one-stage PT and was created to standardize results caused by the variation in reagents. The INR should be between 2.0 and 3.0 for most thrombosis and embolus conditions and between 3.0 and 4.5 for clients with a history of recurrent thromboembolism or mechanical heart valves (O’Neill, 2002) (see Nutritional Considerations Box and Chapter 10 for in-depth information on nutrition). The erythrocyte sedimentation rate (ESR) test measures the time that RBCs take to settle in normal saline over 1 hour. The measured values are reported in millimeters. The test does not relate to one specific condition or disorder but does indicate the presence of inflammation, so it is useful in monitoring the course of inflammatory activity in commonly occurring rheumatic diseases such as polymyalgia rheumatica, temporal arteritis, and rheumatoid arthritis. In addition, when the test is performed with a white cell count, an elevation can indicate infection. Kane, Ouslander, and Abrass (1999) state that mild elevations of 10 to 20 mm/hr in the ESR may be age related. Other scientists report that elevations as high as 30 to 35 mm/hr above normal adult values may be seen, even though no evidence of inflammatory disorders is present. This makes interpretation of the results of this test in older adults difficult without other clinical data and makes it harder to consider differential diagnoses (Calkins, 1999). C-reactive protein (CRP) is a marker present in the acute phase of an inflammatory response (Gambino, 1997). Said to be an earlier indicator than the ESR of any acute processes present in the body (SmithKline Beecham, 1998), CRP is useful to researchers in assessing clients with cardiovascular disease, myocardial infarction, and organ transplants, as well as those recovering from surgical procedures (Gambino, 1997; Oltrona et al, 1997; SmithKline Beecham, 1998). Smith et al (1995) concluded that a persistently high CRP or rising CRP level suggests the failure of antibiotic treatment or the development of a complicated bacterial infectious process. Although still a relatively underused and undervalued test to many practitioners, the CRP is now being examined for its value in place of the ESR in detecting many inflammatory conditions (Gambino, 1997; SmithKline Beecham, 1998). Platelets are small, irregular bodies, also known as thrombocytes, which are essential for clotting. They are formed in the bone marrow and stored in the spleen. When an injury occurs to a blood vessel, platelets are released and become “sticky,” forming a plug at the site and helping to trigger a cascade of other clotting functions (Thibodeau & Patton, 2003). Platelets are important for normal body functioning because of their essential part in normal blood clotting. Decreases in platelet counts (to less than 100,000/mm3) require investigation. In one condition, known as myelodysplastic syndrome (MDS), pancytopenia is noted in more than half the clients diagnosed. Pancytopenia is when the levels of RBCs, WBCs, and platelets are all below normal. More than 50% of the cases found are in adults older than the age of 70. Treatment usually consists of transfusions with red cells or platelets, although most older adults will die of other disorders rather than MDS. This condition has been known to progress to acute leukemia (Gilleece & Dexter, 2002). At platelet levels below 20,000/mm3, the nurse should observe for spontaneous bleeding. If the client’s levels are 40,000/mm3 or below, prolonged bleeding after procedures can occur (Pagana & Pagana, 2003). Older adults in particular may have serious problems with electrolyte imbalances. Dehydration is the most common form of electrolyte disorder that occurs in older adults, and it can usually be attributed to excess loss of water or impaired water ingestion. Excess water loss can occur from infections, such as pneumonia and cystitis, or environmental conditions. Impaired water ingestion may be a result of the age-related decrease in thirst sensation in older adults or a result of decreased functional ability that limits the intake of water (Davis & Minaker, 1999). This includes being bedridden, chemically or physically restrained, or limited by sensory changes. The test for sodium (Na+) measures the amount of sodium in the circulating blood, but it is actually an index of body water deficit or excess. Sodium regulation is important for the maintenance of blood pressure, transmission of nerve impulses, and regulation of body fluid levels in and out of the cells. This movement of sodium affects blood volume, which is tied to the thirst mechanism and total body fluids (Grodner, Long, & DeYoung, 2004). Although sodium is also present in the intracellular fluid, the majority resides in the extracellular fluid, which makes it the major cation of the extracellular fluid. The result of sodium testing describes the balance between ingested sodium and that excreted by the kidneys (Pagana & Pagana, 2003). In older adults, kidney changes such as a decrease in the glomerular filtration rate (GFR) and in the number of nephrons do not lead to disability or disease (Beck, 1999). However, these changes could mean that an older adult may have difficulty in maintaining homeostasis in the presence of crises such as sodium depletion or overload (Table 21–2). TABLE 21–2
Laboratory and Diagnostic Tests
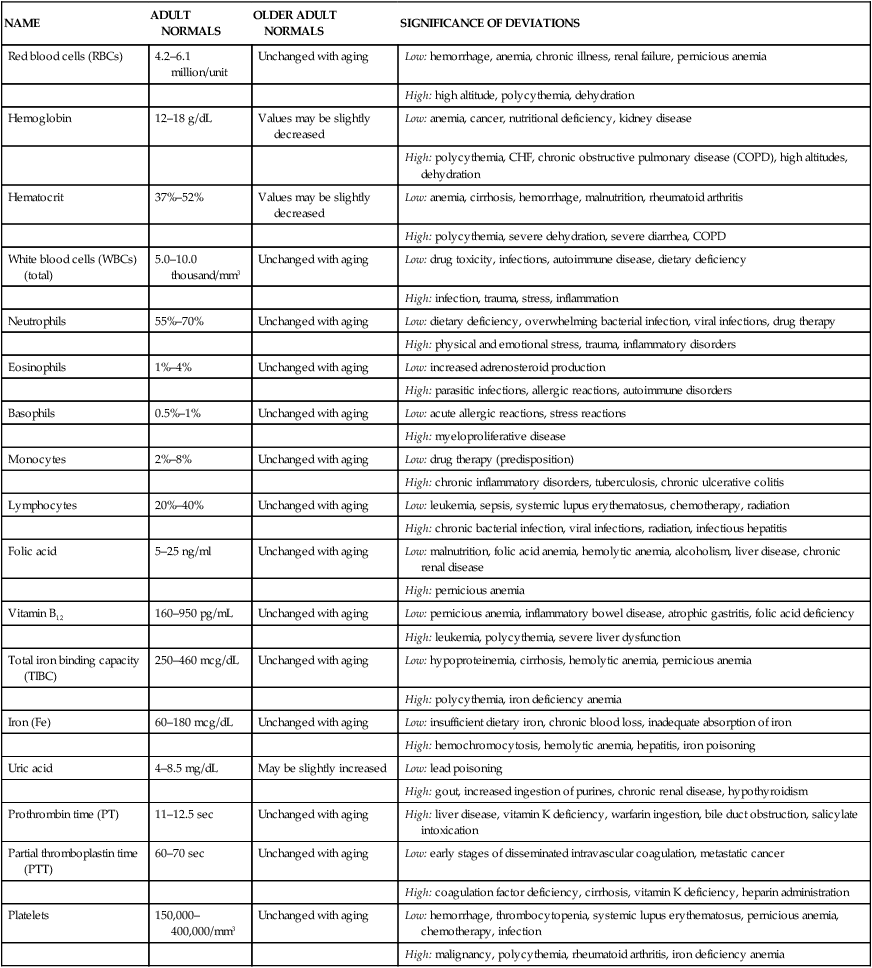
NAME
ADULT NORMALS
OLDER ADULT NORMALS
SIGNIFICANCE OF DEVIATIONS
Red blood cells (RBCs)
4.2–6.1 million/unit
Unchanged with aging
Low: hemorrhage, anemia, chronic illness, renal failure, pernicious anemia
High: high altitude, polycythemia, dehydration
Hemoglobin
12–18 g/dL
Values may be slightly decreased
Low: anemia, cancer, nutritional deficiency, kidney disease
High: polycythemia, CHF, chronic obstructive pulmonary disease (COPD), high altitudes, dehydration
Hematocrit
37%–52%
Values may be slightly decreased
Low: anemia, cirrhosis, hemorrhage, malnutrition, rheumatoid arthritis
High: polycythemia, severe dehydration, severe diarrhea, COPD
White blood cells (WBCs) (total)
5.0–10.0 thousand/mm3
Unchanged with aging
Low: drug toxicity, infections, autoimmune disease, dietary deficiency
High: infection, trauma, stress, inflammation
Neutrophils
55%–70%
Unchanged with aging
Low: dietary deficiency, overwhelming bacterial infection, viral infections, drug therapy
High: physical and emotional stress, trauma, inflammatory disorders
Eosinophils
1%–4%
Unchanged with aging
Low: increased adrenosteroid production
High: parasitic infections, allergic reactions, autoimmune disorders
Basophils
0.5%–1%
Unchanged with aging
Low: acute allergic reactions, stress reactions
High: myeloproliferative disease
Monocytes
2%–8%
Unchanged with aging
Low: drug therapy (predisposition)
High: chronic inflammatory disorders, tuberculosis, chronic ulcerative colitis
Lymphocytes
20%–40%
Unchanged with aging
Low: leukemia, sepsis, systemic lupus erythematosus, chemotherapy, radiation
High: chronic bacterial infection, viral infections, radiation, infectious hepatitis
Folic acid
5–25 ng/ml
Unchanged with aging
Low: malnutrition, folic acid anemia, hemolytic anemia, alcoholism, liver disease, chronic renal disease
High: pernicious anemia
Vitamin B12
160–950 pg/mL
Unchanged with aging
Low: pernicious anemia, inflammatory bowel disease, atrophic gastritis, folic acid deficiency
High: leukemia, polycythemia, severe liver dysfunction
Total iron binding capacity (TIBC)
250–460 mcg/dL
Unchanged with aging
Low: hypoproteinemia, cirrhosis, hemolytic anemia, pernicious anemia
High: polycythemia, iron deficiency anemia
Iron (Fe)
60–180 mcg/dL
Unchanged with aging
Low: insufficient dietary iron, chronic blood loss, inadequate absorption of iron
High: hemochromocytosis, hemolytic anemia, hepatitis, iron poisoning
Uric acid
4–8.5 mg/dL
May be slightly increased
Low: lead poisoning
High: gout, increased ingestion of purines, chronic renal disease, hypothyroidism
Prothrombin time (PT)
11–12.5 sec
Unchanged with aging
High: liver disease, vitamin K deficiency, warfarin ingestion, bile duct obstruction, salicylate intoxication
Partial thromboplastin time (PTT)
60–70 sec
Unchanged with aging
Low: early stages of disseminated intravascular coagulation, metastatic cancer
High: coagulation factor deficiency, cirrhosis, vitamin K deficiency, heparin administration
Platelets
150,000–400,000/mm3
Unchanged with aging
Low: hemorrhage, thrombocytopenia, systemic lupus erythematosus, pernicious anemia, chemotherapy, infection
High: malignancy, polycythemia, rheumatoid arthritis, iron deficiency anemia
Components of Hematologic Testing
Red Blood Cells
Hematocrit
White Blood Cells
Folic Acid
Vitamin B12
Total Iron Binding Capacity
Iron
Uric Acid
Prothrombin Time
Erythrocyte Sedimentation Rate
C-Reactive Protein
Platelets
Components of Blood Chemistry Testing
Electrolytes
Sodium
TEST NAME
ADULT NORMALS
OLDER ADULT NORMALS
SIGNIFICANCE OF DEVIATION
Sodium
136–145 mEq/L
Unchanged with aging
Low: decreased intake, diarrhea, vomiting, diuretic administration, chronic renal failure, congestive heart failure (CHF), peripheral edema, ascites
High: increased intake, Cushing’s syndrome, extensive thermal burns
Potassium
3.5–5 mEq/L
Unchanged with aging
Low: deficient intake, burns, diuretics, Cushing’s syndrome, insulin administration, ascites
High: excessive dietary intake, renal failure, infection, acidosis, dehydration
Chloride
98–106 mEq/L
Unchanged with aging
Low: overhydration, CHF, vomiting, chronic gastric suction, chronic respiratory acidosis, hypokalemia, diuretic therapy
High: dehydration, Cushing’s syndrome, kidney dysfunction, metabolic acidosis, hyperventilation
Calcium
9–10.5 mg/dL
Tends to stay the same or decrease
Low: renal failure, vitamin D deficiency, osteomalacia, malabsorption
High: Paget’s disease of the bone, prolonged immobilization, lymphoma
Phosphorus
3–4.5 mg/dL
Slightly lower
Low: inadequate dietary ingestion, chronic antacid ingestion, hypercalcemia, alcoholism, osteomalacia, malnutrition
High: renal failure, increased dietary intake, hypocalcemia, liver disease
Magnesium
1.3–2.1 mEq/L
Decrease 15% between third and eighth decade
Low: malnutrition, malabsorption, alcoholism, chronic renal disease
High: renal insufficiency, ingestion of magnesium-containing antacids or salts, hypothyroidism
Fasting glucose
70–105 mg/dL
Increase in normal range after age 50
Low: hypothyroidism, liver disease, insulin overdose, starvation
High: diabetes mellitus, acute stress response, diuretic therapy, corticosteroid therapy
Postprandial glucose
Less than 140 mg/dL 2 hr after meal
Less than 160 mg/dL 2 hr after meal
Low: hypothyroidism, insulin overdose, malabsorption
High: diabetes mellitus, malnutrition, Cushing’s syndrome, chronic renal failure, diuretic therapy, corticosteroid therapy
Amylase
60–120 Somogyi units/dL
Slightly increased in elderly
High: acute pancreatitis, perforated bowel, acute cholecystitis, diabetic ketoacidosis
Glycosylated hemoglobin (Hgb A1c)
2.2%–4.8%
Unchanged with aging
Low: hemolytic anemia, chronic renal failure
High: newly diagnosed diabetes, poorly controlled diabetes, nondiabetic hyperglycemia
Total protein
6.4–8.3 g/dL
Unchanged with aging
Low: liver disease, malnutrition, ascites
High: hemoconcentration
Albumin
3.5–5 g/dL
Decrease slightly with aging
Low: malnutrition, liver disease, overhydration
High: dehydration
Blood urea nitrogen (BUN)
7–22 mg/dL
May be slightly higher
Low: liver failure, overhydration, malnutrition
High: hypovolemia, dehydration, alimentary tube feeding, renal disease
Creatinine
0.7–1.5 mg/dL
Decrease in muscle mass may cause decreased values
Low: debilitation, decreased muscle mass
High: reduced renal blood flow, diabetic neuropathy, urinary tract obstruction
Creatinine clearance
87–107 mL/min
Values decrease 6.5 mL/min/decade of life due to a decline in glomerular filtration rate (GFR)
Low: impaired kidney function, CHF, cirrhosis
High: high cardiac output syndromes
Cholesterol (total)
>200 mg/dL
Increases until about middle age but decreases thereafter (or can increase abruptly in women)
Low: malabsorption, malnutrition, cholesterol-lowering medication, pernicious anemia, liver disease, myocardial infarction
High: hypercholesteremia, hyperlipidemia, hypothyroidism, uncontrolled diabetes mellitus
High-density lipoprotein (HDL)
>45 mg/dL
Unchanged with aging
Low: familial low HDL, liver disease, hypoproteinemia
High: familial HDL lipoproteinemia, excessive exercise
Low-density lipoprotein (LDL)
60–180 mg/dL
Increases with aging after menopause
Low: hypolipoproteinemia
High: hypothyroidism, alcohol consumption, chronic liver disease, Cushing’s syndrome
Alkaline phosphatase
30–120 U/L
Slightly higher
Low: hypothyroidism, malnutrition, pernicious anemia
High: cirrhosis, healing fracture, Paget’s disease
Acid phosphatase
0.13–0.63 U/L
Unchanged with aging
Low: thrombosis
High: heparin administration, cirrhosis, prostate cancer
Aspartate transaminase (AST)
0–35 U/L
Values slightly higher
Low: acute renal disease, diabetic ketoacidosis, chronic renal dialysis
High: myocardial infarction, hepatitis, cirrhosis, multiple trauma, acute hemolytic anemia
Creatinine kinase (CK)
30–170 U/L
Unchanged with aging
High: diseases or injury affecting heart muscle, skeletal muscle, and brain ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


