Intrapartum Fetal Surveillance
Learning Objectives
After studying this chapter, you should be able to:
• Identify the purposes of fetal surveillance before birth.
• Explain the normal and pathologic mechanisms that influence fetal heart rate (FHR).
• Describe appropriate nursing responses to nonreassuring FHR patterns.
• Use the nursing process to plan care for a woman having electronic fetal monitoring.
![]()
http://evolve.elsevier.com/McKinney/mat-ch/
Fetal surveillance uses any of several methods to identify signs associated with well-being or with compromise. Accurate assessment of these signs promotes appropriate and timely care to reduce hazards to the fetus. Before birth there are two patients: the mother and her fetus. The purposes of antepartum and intrapartum fetal surveillance are to evaluate the fetal condition during pregnancy and to identify possible hypoxic insult to the fetus during labor. Fetal surveillance cannot identify every compromised fetus. Although this chapter focuses on fetal surveillance of the woman during labor, many of these techniques and guidelines may be used in the care of a woman with an antepartum complication.
Two basic approaches are taken to intrapartum fetal surveillance—low-tech and high-tech approaches. Each has advantages and limitations. Neither is superior. The low-tech approach uses intermittent auscultation (IA) of fetal heart rate (FHR) and palpation of uterine activity. Electronic fetal monitoring (EFM) is the second approach to intrapartum fetal surveillance. Although EFM is dominant in U.S. hospital births, its routine use remains controversial because its benefits to the fetus are not always clear. Other data, such as assessment for fetal movement (see Chapter 15), or cord blood gases, may be added to FHR and contraction data to provide a balanced view of the fetal condition.
Fetal Oxygenation
Adequate fetal oxygenation requires five related factors:
• Normal maternal blood flow and volume to the placenta
• Normal oxygen saturation in maternal blood
• Adequate exchange of oxygen and carbon dioxide in the placenta
• An open circulatory path between the placenta and the fetus through vessels in the umbilical cord
Labor is stressful for a fetus, but several mechanisms compensate for these stresses. One must understand the dynamics of uteroplacental exchange and fetal circulation to understand fetal responses to labor. (See also Chapter 12 for a discussion of fetal circulation and placental functions.)
Uteroplacental Exchange
Oxygen-rich and nutrient-rich blood from the mother enters the intervillous spaces of the placenta through the spiral arteries (see Figure 12-7). Oxygen and nutrients in the maternal blood pass into the fetal blood that circulates in capillaries in the intervillous spaces. Carbon dioxide and other waste products pass from the fetal blood into the maternal blood at the same time. Maternal blood carrying fetal waste products drains from the intervillous spaces through endometrial veins and returns to the mother’s circulation for elimination by her body. Substances pass back and forth between mother and fetus without mixing of maternal and fetal blood if fetal capillaries remain intact.
During labor, contractions gradually compress the spiral arteries, temporarily stopping maternal blood flow into the intervillous spaces. During contractions, the fetus depends on the oxygen supply already present in body cells, fetal erythrocytes, and the intervillous spaces. The oxygen supply in these areas is enough for about 1 to 2 minutes. As each contraction relaxes, freshly oxygenated maternal blood re-enters the intervillous spaces and waste-laden blood drains out.
Fetal Circulation
The fetal heart circulates oxygenated blood from the placenta throughout the body and returns deoxygenated blood to the placenta. The umbilical vein carries oxygenated blood to the fetus, and the two umbilical arteries carry deoxygenated blood from the fetus to the placenta (see Figure 12-7).
Fetal Heart Rate Regulation
Mechanisms that regulate FHR are balanced to maintain cardiac output at a level that keeps the fetal heart and brain oxygenated. Fetal cardiac output increase is accomplished primarily by an increase in the heart rate. Conversely, a marked decrease in FHR decreases the cardiac output.
Five fetal factors that interact to regulate FHR include the:
The balance among forces that increase and those that slow the heart rate result in the characteristic fluctuations in FHR during late pregnancy.
Autonomic Nervous System
The sympathetic and parasympathetic branches of the autonomic nervous system are balanced forces that regulate FHR. Sympathetic stimulation increases the heart rate and strengthens myocardial contractions through release of epinephrine and norepinephrine. The net result of sympathetic stimulation is an increase in cardiac output.
The parasympathetic nervous system, through stimulation of the vagus nerve, reduces FHR and maintains variability. The parasympathetic branch gradually exerts greater influence as the fetus matures, beginning between 28 and 32 weeks of gestation. Therefore the average FHR in the term fetus is slightly lower than in the preterm fetus. However, variability of FHR near full term is often more dramatic than a fetus just a few weeks younger than full term.
Baroreceptors
Cells in the carotid arch and major arteries respond to stretching when the fetal blood pressure increases. These baroreceptors stimulate the vagus nerve to slow FHR and decrease the blood pressure, thus lowering cardiac output. As fetal blood pressure falls, the heart rate accelerates to maintain normal cardiac output.
Chemoreceptors
Cells that respond to changes in oxygen, carbon dioxide, and pH are chemoreceptors found in the medulla oblongata and in the aortic and carotid bodies. Decreased oxygen content, increased carbon dioxide content, or a lower pH in the blood or cerebrospinal fluid triggers an increase in the heart rate. However, prolonged hypoxia (low oxygen), hypercapnia (excess carbon dioxide in blood [elevated carbon dioxide partial pressure {PCO2}]), and acidosis (low pH from accumulation of acid [hydrogen ions] or depletion of base [bicarbonate ions]) depress FHR.
Adrenal Glands
The adrenal medulla secretes epinephrine and norepinephrine in response to stress, causing a response from the sympathetic nervous system that accelerates FHR. The adrenal cortex responds to a decrease in the fetal blood pressure with release of aldosterone and retention of sodium and water, resulting in an increase in the circulating fetal blood volume.
Central Nervous System
The fetal cerebral cortex causes the heart rate to increase during fetal movement and to decrease when the fetus sleeps. The hypothalamus coordinates the two branches of the autonomic nervous system. The medulla oblongata maintains the balance between stimuli that speed and stimuli that slow the heart rate.
Pathologic Influences on Fetal Oxygenation
Fetal oxygenation may be compromised by alterations in any of the placental or fetal factors or those of the pregnant woman.
Maternal Cardiopulmonary Alterations
Actual or relative reductions in the mother’s circulating blood volume reduce perfusion of the intervillous spaces with oxygenated maternal blood. Hemorrhage causes an actual decrease in her blood volume. Relative reductions in maternal circulating volume result from altered distribution of the blood volume without blood loss. For example, epidural block analgesia may result in vasodilation, which increases the capacity of the maternal vascular bed. However, the amount of blood available to fill the vessels is unchanged. Hypotension can result, reducing placental blood flow.
Maternal hypertension may reduce blood flow to the placenta because of vasospasm and narrowing of the spiral arteries.
A lowered oxygen level in the mother’s blood reduces the amount available to the fetus. Maternal acid-base alterations, which often accompany respiratory abnormalities or diabetic ketoacidosis, may also compromise exchange in the placenta. A lower maternal oxygen tension may result from respiratory disorders, such as asthma or acute pulmonary infections, or from smoking.
Uterine Activity
Hypertonic contractions that are too long (≥90 to 120 seconds), too frequent (closer than every 2 minutes, or have an inadequate relaxation period (less than 30 seconds of complete relaxation) will not allow optimal uteroplacental exchange. Additional criteria may be specified when internal EFM is used. The uterus may never fully relax between contractions, applying continuous compression to the spiral arteries and reducing maternal-fetal exchange in the intervillous spaces. Excess uterine activity may occur with prostaglandin or oxytocin administration, but it may also occur with no external stimulation. A fetus with good oxygen reserve may never show signs of compromise, even with excessive contractions. Likewise, the fetus with little reserve may show compromise, even with weak uterine activity.
Placental Disruptions
Conditions such as abruptio placentae (separation of the placenta before birth) and infarcts (necrosis of varying amounts of placental tissue) reduce the placental surface area available for exchange. The amount and location of placental disruption relate to the degree of impairment in uteroplacental exchange.
Interruptions in Umbilical Flow
The usual cause of interrupted blood flow through the umbilical cord is compression. Blood flow through the umbilical cord may be reduced by compression between the fetal presenting part and the pelvis, a nuchal cord (around the fetal neck), one that is wrapped around the fetal body, or a knot in the cord. It may occur with oligohydramnios, because the amount of amniotic fluid is inadequate to cushion the cord. The umbilical cord may become tangled around fetal body parts. The fetus may compress the cord by grasping with the hand.
The thin-walled umbilical vein is compressed initially, reducing flow of more highly oxygenated blood into the fetus. This results in initial hypoxia with hypotension. Baroreceptors and chemoreceptors respond by accelerating FHR. Flow from the fetus to the placenta through the firmer-walled umbilical arteries falls as cord compression continues, resulting in hypertension from increased fetal blood volume. Baroreceptors respond to hypertension by stimulating the vagus nerve, thus reducing fetal blood pressure and slowing the fetal heart. The FHR again accelerates as pressure on the arteries, and then the vein, is relieved.
Fetal Alterations
Fetal tissues may be hypoxic despite an adequate oxygen supply from the mother and adequate exchange within the placenta. A low circulating fetal blood volume, fetal hypotension, or fetal anemia reduces the ability of fetal erythrocytes to deliver oxygen to body cells. Central nervous system or cardiac abnormalities may cause an abnormal rate or rhythm. For example, a fetus with complete heart block may not respond to stimuli that would normally cause a rate increase.
Prolonged fetal bradycardia may be both a response to hypoxia and a contributing factor to hypoxia because fetal oxygenation is rate dependent. Prolonged tachycardia also can decrease cardiac output because the ventricles have less time to fill with oxygenated blood during diastole.
Risk Factors for Fetal Compromise
When conditions associated with reduced fetal oxygenation exist (Box 17-1), surveillance by either IA and palpation or EFM should be done more often. No difference in perinatal outcome has been demonstrated between properly performed IA and EFM. However EFM is used for most births in the United States (American Academy of Pediatrics [AAP] & American College of Obstetricians and Gynecologists [ACOG], 2007; American College of Nurse-Midwives [ACNM], 2010; ACOG, 2009, 2010).
Auscultation and Palpation
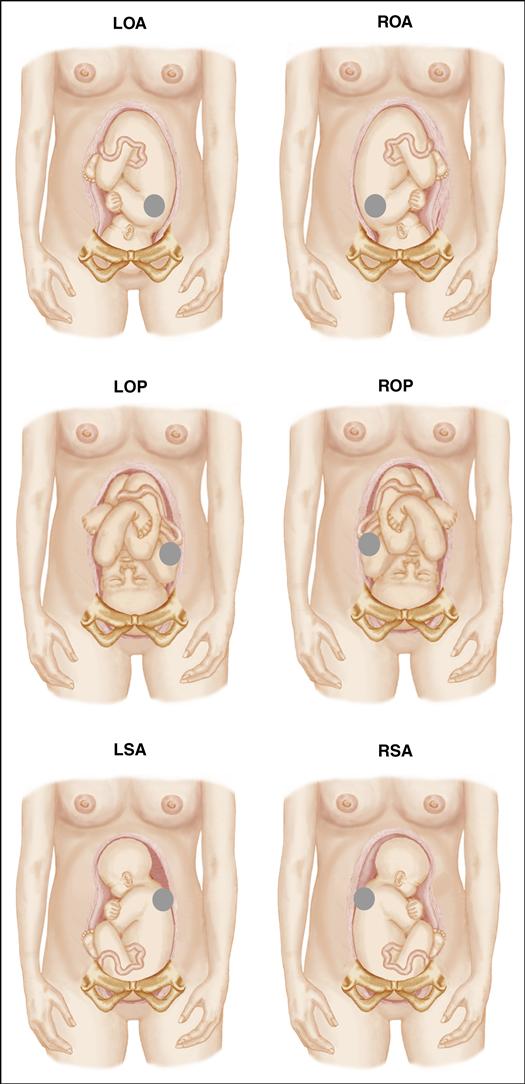
The nurse may use IA of FHR and palpation of uterine activity for intrapartum fetal surveillance (Procedure: Auscultating the Fetal Heart Rate, p. 368). IA can be done using either the fetoscope or Doppler ultrasound (Figure 17-1). Doppler auscultation is most common because of its ease of use, ability to adjust the volume, and compact size. Many Doppler devices have a digital or paper display of the rate, and some may be used under water. The Doppler creates an electronic sound based on movements of the fetal heart and may be the only way to use auscultation if a woman has a thick abdominal fat pad. However, the nonelectronic fetoscope is useful in cases of fetal cardiac dysrhythmias because its sound is that of actual opening and closing of heart valves, similar to the amplified sounds one hears with a stethoscope.
Advantages
Mobility is the primary advantage of auscultation and palpation for intrapartum fetal monitoring of the fetus at low risk. The woman is free to change position and walk, which is especially helpful during early labor or with a fetal occiput posterior position (see Chapter 16). She can use water-based methods of pain management, such as whirlpool baths or showers. The atmosphere is more natural than technologic, which is important to some families during their birth experience.
Limitations
One disadvantage of IA and palpation as the primary method of fetal assessment is that FHR and uterine activity are assessed for a small part of the total labor. Labor contractions place stress on the fetus because of the normal reduction of blood flow to the placenta at that time. Although FHR is assessed during some contractions, it is not recorded during every contraction. Continuous electronic or paper recording is not available on every Doppler to show the fetal response throughout labor or to identify subtle trends in the response.
Some women find that interruptions for auscultation are distracting. The pressure of the instrument on the abdomen is uncomfortable for some, and it may require several moves to locate the best place for auscultation with each assessment.
IA is staff intensive. Auscultation may not be a realistic option as the primary method of intrapartum fetal surveillance if the nurse-to-patient ratio must be greater than 1:1 for patients in normal labor. ACOG recommends continuous fetal monitoring if high-risk conditions exist in the woman or fetus, such as diabetes or fetal growth restriction (ACNM, 2010; ACOG, 2009; Feinstein, Sprague, & Trépanier, 2008).
Evaluating Auscultated Fetal Heart Rate Data
Both the fetoscope and Doppler transducer, a device that translates one physical quantity into another, can be used to identify FHR baseline, rhythm, and changes from the baseline (see Table 17-1, page 378). Because the fetoscope is detecting actual fetal heart sounds, it is reliable for detecting fetal dysrhythmias. The Doppler transducer (and external fetal monitor if it is being used for IA) also can be used to detect baseline, rhythm, and changes in the baseline. However, the Doppler transducer or external fetal monitor cannot be used to reliably detect fetal dysrhythmias. The fetoscope is rarely used in the United States despite its reliability in evaluation of fetal dysrhythmias.
Electronic Fetal Monitoring
EFM may be continuous, starting shortly after the woman is admitted, or intermittent, with a short recording made at regular intervals during labor, similar to auscultation.
Subjectivity of interpretation and use of varying descriptive terminology have made outcomes of research difficult to evaluate. A 2008 workshop was held to review and update definitions to describe EFM patterns and to make recommendations about a classification system for use in the United States. The most recent definitions are for visual interpretation of patterns, but the 2008 group recognized that computer programs for interpretation are being developed. Three categories, rather than the previous two categories, describe the fetus at that point in time and are not predictive of disorders such as cerebral palsy. Interventions may result in a change of the interpretation category
(Macones, Hankins, Spong, et al., 2008). Guidelines from the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN)’s Fetal Heart Monitoring: Principles and Practices (Lyndon & Usher, 2009) and terminology from the National Institute of Child Health and Human Development (NICHD) workshops (1997, 2008) are used in a simplified form here.
Advantages
The electronic monitor supplies more data about the fetus than auscultation, and provides a permanent record that may be printed or stored electronically. Gradual trends in FHR and uterine activity are more apparent because the strip provides a graphic record for review. Continuous EFM shows the fetal response before, during, and after every contraction while it is in use rather than providing a sampling of fetal responses to contractions and between them. However the many studies of IA versus EFM have found the two techniques equally valid for the low-risk fetus (ACOG, 2009; Bashore & Koos, 2010; Harmon, 2009).
EFM is prevalent in U.S. births that occur in hospitals. Most women entering the hospital for birth expect electronic monitoring, even if their pregnancy has been low risk. The woman and support person may find the constant sound of the fetal heartbeat comforting. The coach can use the tracing of contractions on the monitor strip to help the woman anticipate the beginning and end of each contraction.
Electronic monitoring allows one nurse to observe two laboring women, primarily during uncomplicated early labor. A 1:1 nurse-to-patient ratio is needed during the second stage of labor or if high-risk conditions exist, regardless of the monitoring method used. Electronic monitoring gives the nurse more time for teaching and supporting the laboring woman with breathing and relaxation techniques if the nurse maintains the primary focus on the woman, not on the technology.
Limitations
Reduced mobility is the major limitation of electronic fetal monitoring. Frequent maternal position changes or an active fetus may require constant adjustment of equipment to maintain a near-continuous trace. In addition, repositioning the equipment is necessary as the baby moves downward in the pelvis during labor. The belts or stockinette used to keep sensors positioned properly for external monitoring are uncomfortable for some women, and obtaining a good trace is often difficult for the woman with a thick abdominal fat pad. A woman may concentrate on maintaining a good tracing rather than making herself comfortable or using a position to enhance fetal rotation and descent.
EFM and other procedures impart a technical air to the birth process and may be objectionable to a woman and her partner.
Electronic Fetal Monitoring Equipment
EFM equipment consists of the bedside monitor unit and sensors for FHR and uterine activity. Sensors for each function may be either internal or external. Computer interfaces allow addition of chart annotations and admission and birth information and provide electronic storage of information. Models with telemetry (wireless transmission of data to the base for observation and storage), allow ambulation while monitoring.
Fetal monitor clocks should be synchronized throughout the unit, often by connection to an atomic clock. Using the fetal monitor clock to determine the birth time allows the most accurate reconstruction of the events of labor. In legal proceedings, the amount of time required to accomplish corrective interventions can make a difference in the defense of a lawsuit.
Bedside Monitor Unit
The bedside fetal monitor unit uses the information from FHR and uterine activity sensors to provide a visual output in the form of a numeric display and a graphic strip. The strip may be printed by the monitor itself, similar to an electrocardiogram (ECG) strip, or viewed on a computer screen. The strip can be printed if electronic storage is not available in facilities that use a computer interface with the bedside monitor. Simultaneous monitoring of twins is possible for most fetal monitors.
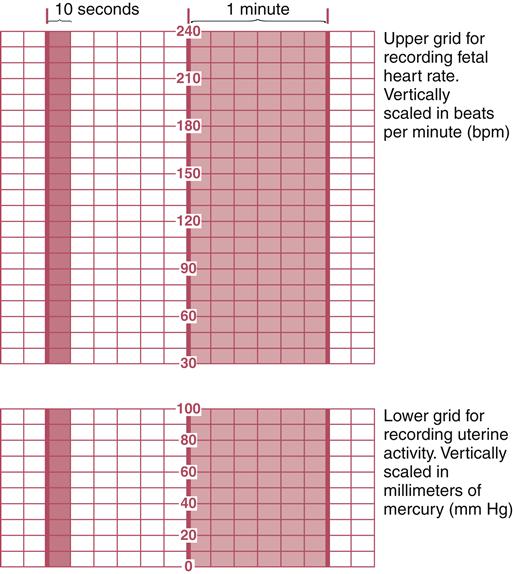
Paper Strip
Data about FHR and uterine activity may be displayed on paper using two horizontal grids—one for FHR and another for the uterine activity (Figure 17-2). Each segment of paper between folds is numbered for identification and reassembly of a multipart strip. Time and date markers provide sequencing. Strips on computer screens have the same pattern.
FHR is recorded on the upper grid. The range of recorded rates is from 30 to 240 beats per minute (bpm).
Uterine activity is recorded on the lower grid as bell-shaped curves with continuous smaller rises and falls that represent maternal breathing superimposed on the larger curve. Fetal movements, maternal coughing, vomiting, or position changes cause erratic curves or spikes on the uterine activity line. Contraction intensity and the degree of uterine muscle tension, or uterine resting tone (from 0 to 100 mm Hg), are recorded on the lower grid.
Vertical lines on both upper and lower grids are time divisions. At a paper speed of 3 cm per minute, dark vertical lines are 1 minute apart. Lighter lines subdivide the 1-minute divisions into six 10-second segments. The vertical lines are used to time the frequency and duration of contractions and to identify the fetal response to the contractions. The scroll speed of a screen display uses similar time divisions as a printed strip.
Remote Surveillance
Many facilities have a display for each woman at central locations to allow surveillance when the nurse is not at the bedside. These units display the tracing on a screen and have settings for audible and visual alerts, such as an abnormal FHR or maternal blood pressure.
Devices for External Fetal Monitoring
Both FHR and uterine activity can be monitored by external sensors (device that translates one physical quantity into another), or transducers. Transducers are secured on the mother’s abdomen by elastic straps, a tube of wide stockinette, or an adhesive ring (Figure 17-3). External devices are less accurate than internal ones but are noninvasive and are suitable for most women in labor. Procedure: External Fetal Monitor contains instructions for using the external electronic fetal monitor.
Fetal Heart Rate Monitoring with an Ultrasound Transducer
A Doppler ultrasound transducer detects fetal heart movement for rate calculation. It is similar to the hand-held Doppler unit. The transducer sends high-frequency sound waves into the uterus. The sound waves are reflected, and the monitor’s computer continuously calculates FHR based on the movement sensed as the heart beats.
Fetal heart motion does not always correlate with electrical heart activity. Other movements, such as fetal or maternal activity or blood flow through the umbilical cord and the woman’s aorta, also can be detected. Modern monitors ignore most of these extraneous sounds to provide a clean tracing.
The Doppler transducer produces a two-part sound with each heartbeat. Fetal or maternal activity produces a rough, erratic sound rather than the crisp, rhythmic sound characteristic of fetal heart motion. Fetal hiccups cause a “th-thump” sound at regular intervals that is superimposed on sounds created by heart activity. Volume can be adjusted or turned off.
Uterine Activity Monitoring with a Tocotransducer
A tocotransducer (“toco”) with a pressure-sensitive area detects changes in abdominal contour to measure uterine activity. The uterus pushes outward against the mother’s anterior abdominal wall with each contraction. The monitor calculates changes in this signal and prints them as bell shapes on the lower grid of the strip.
Movement other than uterine activity also registers on the monitor. For example, maternal respirations superimpose a zigzag appearance on the uterine activity line. Other fetal or maternal movements appear as spikes on the uterine activity tracing.
Because uterine activity is sensed through the woman’s abdomen, a tocotransducer is useful for observing the frequency and duration of contractions. It does not reliably measure internal contraction intensity and uterine resting tone. Factors that affect apparent intensity as printed on the strip include:
Devices for Internal Fetal Monitoring
Accuracy is the main advantage of using internal devices for EFM, but they are invasive, slightly increasing the risk for infection. Their use requires ruptured membranes and about 2 cm of cervical dilation.
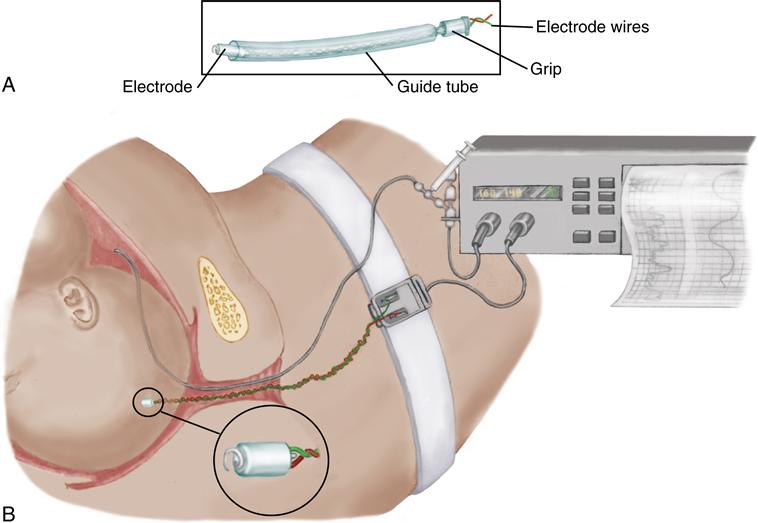
Fetal Heart Rate Monitoring with a Scalp Electrode
The fetal scalp electrode (FSE) detects electrical signals from the fetal heart (Figure 17-4). Fetal or maternal movement interferes less with accuracy because the rate is calculated from electrical events in the fetal heart. The monitor unit generates a beeping sound with each fetal heartbeat, but the volume of the sound can be adjusted.
Areas to avoid for electrode application are the fetal face, fontanels, and genitals. The wire from the electrode protrudes from the mother’s vagina and is attached to a leg plate to provide electrical grounding.
Because it barely penetrates the fetal skin (about 1 mm), the electrode is easily displaced. The tracing then becomes erratic or stops if the electrode is fully detached. Secure attachment of the electrode is often difficult if the fetus has thick hair. The electrode is removed by turning it counterclockwise about one and one half turns until it detaches.
Uterine Activity Monitoring with an Intrauterine Pressure Catheter
Two kinds of intrauterine pressure catheters (IUPCs) can be used to measure uterine activity, including contraction intensity and resting tone. These are:
1. A solid catheter with a pressure transducer in its tip (Figure 17-5). This catheter usually has an additional lumen for amnioinfusion, or infusion of sterile solution into the uterus (see p. 380).
2. A hollow, fluid-filled catheter that connects to a pressure transducer on the bedside monitor unit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree