CHAPTER 18 Intervention in a situation of elder abuse and neglect
FRAMEWORK
Elder abuse is another of the taboo topics that is challenging health professionals from all disciplines. Current debate is around the question of mandatory reporting. For health professionals recognition of abuse is difficult and, if suspected, there are few guidelines to assist action. Responses need to be sensitive, ethical and legal. This chapter takes a practical approach to raising awareness of the key issues. [RN, SG]
Definition and overview of elder abuse
Abuse of older people is any behaviour that causes physical, psychological, financial, or social harm to an older person (WHO 2002b). Abuse can occur within any relationship where there is an expectation of trust between the older person and the person who becomes the abuser. Abuse may involve a single act, repeated behaviour, or a lack of appropriate action. It may occur when a vulnerable older person is persuaded to enter into a financial or sexual transaction to which he or she has not consented, or cannot consent. Many forms of abuse of older people are crimes (Australian and New Zealand Association of Geriatric Medicine 2003; NSW Office for Ageing 2007).
Identification of elder abuse
One of the major problems in dealing with abuse is difficulty in recognition. It is necessary to be on the alert and be vigilant, because symptoms and signs of abuse are often subtle, and can be wrongly attributed to the ageing process itself (Choi & Mayer 2000).
There are many symptoms and signs that may be suggestive of abuse, and these are outlined below. However, it is also important to remember that the presence of one or more of the signs listed does not necessarily establish that abuse is occurring, as many of these symptoms are seen in frail older people with chronic disease. Ageing skin may bruise more readily, bones may fracture more easily due to osteoporosis and falls may occur more often due to degenerative changes or disease in the central nervous system. It is important to differentiate between those symptoms and signs that are due to physiological changes and those due to abuse (Carney et al 2003).
Types of abuse and recognisable signs and symptoms include:
Vulnerability to abuse
Some older people may be particularly vulnerable to risk of abuse because they may be:
Prevalence of elder abuse
Estimates of the prevalence of abuse vary between 2.5–6% of the population aged 65 and over, however Australia lacks reliable national data in this regard (Boldy et al 2002).
Reasons for the emergence of elder abuse as a contemporary social issue
There are several key reasons for the emergence of elder abuse as a contemporary social issue. Firstly, the ageing of the Australian population means that more individuals are now surviving into late life, often with increasing frailty and with increasing incidence of conditions like dementia and stroke. Abuse can occur both within the community and in the residential setting, and may be perpetrated by family members, other carers, or outside individuals. With more older people now entering residential care, as well as living on their own in the community, the opportunity for abuse has increased. There is also considerable pressure on care resources in ageing societies when families may live at some distance from elderly relatives and may not be able to provide or monitor appropriate care because of their own work commitments; even if providing care, family members may experience the burden and stresses of care as overwhelming. Older generations today possess considerable wealth and substantial housing assets which makes them vulnerable to financial manipulation both by family members and other external parties, such as unscrupulous solicitors or financial advisors. Financial abuse is reported as one of the most significant forms of contemporary abuse in families partly because many adult children wrongly assume that their parents’ assets are their assets (Bonnie & Wallace 2003; Lachs & Pillemer 2004).
General principles for assessment
It is necessary to gain the consent of the person who has been abused for any assessment and whilst they may be happy to be interviewed and examined, there are often situations where they do not want any further action taken. Older people may be reluctant to report abuse by a family member or caregiver on whom they rely for their basic needs. There may be shame where a close family member is the abuser, or there may be fear of retaliation or fear of institutionalisation. If the person does not give consent to further action and is competent to make that decision then that decision must be respected (Anetzberger 2005; Dyer et al 2003; Kurrle et al 1997).
It is important to take a non-judgmental approach to cases of abuse and often it is most appropriate to look at the situation as one in which there are two victims, rather than a victim and an abuser. Attention must be paid to resolving the unmet needs of both victim and abuser rather than simply identifying abuse and punishing the guilty party (Kinnear & Graycar 1999).
There are a number of ethical principles to be observed in relation to intervention in situations of elder abuse. Beneficence is the principle of doing good and ensuring that the best interests of the person are promoted. Harming or destroying a fragile family relationship that is important to the older person in the process of dealing with an abusive situation is not observing this principle. This may be averted by taking the non-judgmental approach described above. Autonomy is the principle of freedom of choice, the right of an individual to make decisions for themselves that are independent and made without coercion or undue influence. There are often major dilemmas involving our duty of care associated with the principle of beneficence, and the victim’s freedom of choice, when we have a victim in a situation of abuse and clearly at risk who wishes to stay in that situation. If that person is competent to make that decision then that is their right (Kosberg et al 1996; Kosberg et al 2005).
Confidentiality is a basic tenet of health care, but there are times when health care professionals have to disclose information and so the principle of confidentiality is overridden. This occurs where there is a subpoena, or where the practitioner believes that a crime has been committed, or where it is in the individual’s interest; for example, if the individual is suicidal. Here the principle of beneficence might take precedence over confidentiality (James & Graycar 2000).
It is absolutely imperative to know whether a person has mental capacity; that is, whether they are competent to make decisions. This is relevant from the taking of a history through to arranging appropriate interventions. If a person is incapable of giving an accurate history due to dementia or psychiatric illness, then involvement of others (family members, friends, service providers) is essential. It is important to remember that capacity is task specific, and a person with dementia may be quite able to make reasonable decisions about what they wish to wear, or eat for dinner, but may not be able to consent to a major surgical procedure or make financial decisions. Whilst it is ultimately a legal decision as to whether a person is competent or not, the assessment of the health care professional is very important. To the degree possible, the person suffering the abuse should be involved in decision making (Setterlund et al 1999).
Decision making in relation to elder abuse
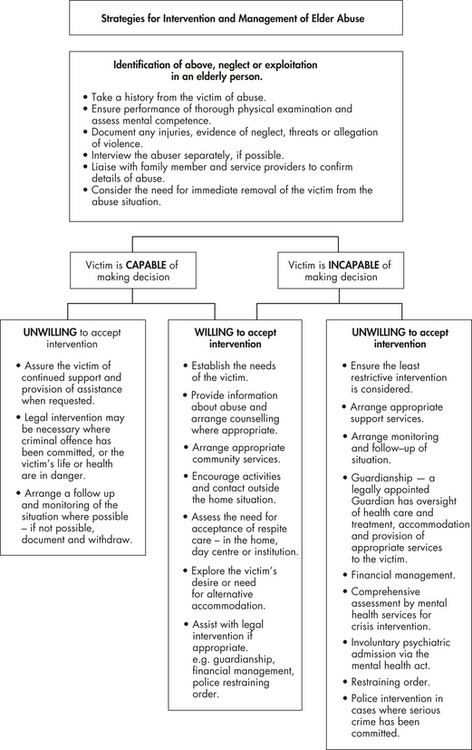
Several decision trees exist in relation to the identification of, and intervention in, situations of elder abuse. These frameworks are useful as guides, though may need supplementation by local protocols, or expert input of particular professionals. A typical protocol is presented in Figure 18.1.

 One of the major problems in dealing with abuse is difficulty in recognition.
One of the major problems in dealing with abuse is difficulty in recognition. Some older people may be particularly vulnerable to risk of abuse.
Some older people may be particularly vulnerable to risk of abuse. There are several key reasons for the emergence of elder abuse as a contemporary social issue.
There are several key reasons for the emergence of elder abuse as a contemporary social issue. There are a number of ethical principles to be observed in relation to intervention in situations of elder abuse.
There are a number of ethical principles to be observed in relation to intervention in situations of elder abuse.