After studying this chapter, the reader will be able to: 1. Describe key attributes of electronic health record systems and their influence on patient safety and quality care. 2. Explain “meaningful use” criteria as applicable to electronic health records. 3. Critique various types of point-of-care technology and their use in the clinical setting. 4. Assess how future trends in technology will affect health care delivery. 5. Use established criteria to evaluate the content of health-related sites found on the Internet. Software programs that process data to produce or recommend decisions by linking with an electronic knowledge base controlled by established rules for combining data elements; the knowledge base and rules mimic the knowledge and reasoning an expert health professional would apply to data and information to solve a problem. EHR(electronic health record) interoperability EHR systems that have ability to share and transfer patient data seamlessly across health care systems and settings in a standardized manner that protects the reliability, confidentiality, privacy, and security of the information. A defined set of EHR capabilities and standards that EHR systems must meet to ensure that their full capacity is realized and for the users (hospitals and physician practices) to qualify for financial incentives from Medicare. Electronic health record (EHR) The longitudinal electronic record of patient health information generated by one or more encounters in any care delivery setting; has the ability to support other care-related activity such as evidence-based decision support, quality management, and outcomes reporting (American Health Information Management Association [AHIMA], 2012). The use of various forms of technology to improve the quality of health services to individuals and communities. The hardware and software that enable information to be stored, retrieved, communicated, and managed. Technologies that allow real-time data retrieval, documentation, and decision support at the bedside or where direct care is provided. Additional resources are available online at: http://evolve.elsevier.com/Cherry/ VIGNETTE Questions to Consider While Reading This Chapter 1. What are the potential benefits of electronic health records to nurses, other health care providers, and patients? 2. What are the barriers to a universal U.S. health information technology infrastructure? 3. What is meant by “meaningful use” of EHRs? 4. How might advanced point-of-care technology influence health care at the bedside? 5. How does health information technology impact consumer health? Thanks to Leslie H. Nicoll, PhD, MBA, RN, and Cynthia K. Russell, PhD, APN, for their contributions to this chapter in previous editions. Today’s clinical setting is undergoing an explosion in technology used by all health care providers. Yesteryear’s clinical settings used telephones, fax and copy machines, and slow computers that primarily stored patients’ contact and billing information. Today you are likely to see voice communication systems, handheld computers or tablets, smartphones, robotic pharmacy dispensaries, and fast computers that contain patients’ electronic health records (EHRs). These records present data in graphs, tables, and charts that may reveal a different story than words and numbers alone. Transforming patient data into meaningful bits of information is merely one advantage of health information technology (HIT). These data can also be shared with other facilities, creating a comprehensive patient record, which can reduce duplicate services and tests and create continuity in care. In this chapter, you will explore the important role of HIT in today’s clinical environment, the adoption rate of this technology in select countries, barriers and opportunities with advanced HIT, and ways to educate consumers about health information on the Internet. Health information technology (HIT), or technology used to promote the health and well being of patients and the community, has rapidly increased as technology has advanced. These advancements have led to a new era, the information age. People living in the information age demand more sharing of, and access to, knowledge that was once held only by those in positions of authority. Technology advancements have influenced all sectors of civilization across the globe including health care, even in developing countries that have limited access to health care. For example, the United States National Library of Medicine (NLM) provides access to many resources, which are sometimes free. These resources are not limited to the United States, and therefore all countries, including developing countries, have access to information. In 2009, the NLM was accessed daily between 1 and 1,000 times by individuals in sub-Saharan Africa (Royall and Lyon, 2011). Expansion of the Internet is also responsible for promoting access to health resources such as health care websites, medical videos, health promotion games, and images. Advancements in the widespread use of HIT first occurred in European countries. Germany initiated a universal HIT process in 1993, followed by Norway in 1997 and the United Kingdom in 2002. Around the same time, Canada and Australia both initiated efforts to standardize electronic documentation procedures. Denmark achieved 100% EHR adoption by primary care doctors in 2009 (Protti and Johansen, 2010). Clearly, the United States is watching and learning from the progression and transformation of health care in countries that have universally adopted HIT throughout their health care systems. For more than a decade, it has been known that HIT in the United States—specifically EHRs—can reduce costs and improve patient care quality and safety (Chaudhry et al, 2006; Walker et al, 2005). The United States is currently challenged to universally implement EHRs across all settings from hospitals to ambulatory care settings to home health agencies and nursing homes. For EHR systems to have the greatest impact on cost and quality, they must also be interoperable with the ability to exchange information across systems and settings in a standardized manner that protects the reliability, confidentiality, privacy, and security of the information. Within the United States, there are two major influences on the adoption of EHRs, the federal government and America’s health insurance plans (Association of Health Insurance Plans [AHIP], 2005). According to President George W. Bush, “by computerizing health records, we can avoid dangerous medical mistakes, reduce costs, and improve care” (State of the Union Address, January 20, 2004). To this end, President Bush established a goal to have universal EHR adoption in the United States by 2014. President Barack Obama supported this initiative and allocated $25.9 billion of the American Recovery and Reinvestment Act funds to EHR adoption (U.S. Department of Health & Human Services [DHHS], 2012a, para. 2). As a result, a modest growth in adoption of EHRs has occurred. In 2009, 11.9% of acute care hospitals reported using EHRs compared with 8.9% in 2008 (Jha et al, 2010). The Institute of Medicine (IOM) (2003) recommends that EHR systems offer the following eight functionalities: 1) health information and data capture; 2) results/data management; 3) provider order entry management; 4) clinical decision support; 5) electronic communication and connectivity between providers, the health care team, and patients; 6) patient support; 7) administrative process support; and 8) reporting and population health management. Table 14-1 provides more detailed information about these core functionalities. TABLE 14-1 CORE FUNCTIONALITIES FOR EHR SYSTEMS AS RECOMMENDED BY THE INSTITUTE OF MEDICINE (2003) Two specific functionalities recommended by the IOM—clinical decision support and computerized provider order entry (CPOE)—are frequently mentioned in the literature as essential to improve the quality and safety of health care (IOM, 2003; Smith, 2004). Clinical decision support contributes to safety and quality by providing automatic reminders about preventive practices, such as immunizations, drug alerts for dosing and interactions, and electronic resources for data interpretation and clinical decision making. CPOE is defined as the “process by which the physician or another health care provider, such as a nurse practitioner, physician’s assistant, or physical or occupational therapist, directly enters orders for client care into a hospital information system” (Hebda and Czar, 2009, p. 23). CPOE contributes to safety and quality by eliminating lost orders and illegible handwriting; generating related orders automatically (e.g., a laboratory test needed to monitor a specific medication); monitoring for duplicate or contradictory orders; and reducing time to fill orders (Hebda and Czar, 2009; IOM, 2003). CPOE functions also contribute to medical error prevention through the following (Bates and Gawande, 2003): • More readily accessible knowledge • Requirement for key pieces of information (such as the dose of a drug) • Assistance with calculations • Checks performed in real time • Assistance with medication monitoring In addition to providing the core functions as noted earlier, the EHR must be efficient and offer additional support that is dependent on each institution or facility and the type of services that are provided (i.e., ambulatory or inpatient services). For example, an inpatient facility EHR needs to integrate with nursing services, pharmacy, operating room management systems, and laboratory information systems, to name a few. The most commonly accessed functions of an EHR are the laboratory, diagnostics, and radiology reports (Robert Wood Johnson Foundation, 2010). To view sample screens from an EHR, see Figures 14-1 and 14-2. A fully functional EHR is a complex system. Consider a single data element (datum), such as a person’s weight. The system must be able to capture, or record, the weight, then store it, process it, communicate it to others, and present it in a different format, such as a bar graph or chart. All of this must be done in a secure environment that protects the patient’s confidentiality and privacy. The complexity of these issues and the development of the necessary systems help explain why few fully functional EHR systems are in place today. In fact, according to a Robert Wood Johnson Foundation report, only 6.3% of physician offices had fully functioning EHRs in 2009 (DesRoches and Painter, 2010). • Privacy refers to the right of an individual to keep information about himself or herself from being disclosed to anyone else. If a patient has had an abortion and chooses not to tell a health care provider this fact, the patient would be keeping that information private. • Confidentiality refers to the act of limiting disclosure of private matters. Once a patient has disclosed private information to a health care provider, that provider has a responsibility to maintain the confidentiality of that information and not reveal the information to others who do not have a legitimate need to know. • Security refers to the means to control access and protect information from accidental or intentional disclosure to unauthorized persons and from alteration, destruction, or loss. When private information is placed in a confidential EHR, the system must have controls in place to maintain the security of the system and not allow unauthorized persons access to the data (Computer-Based Patient Record Institute [CPRI], 1995). The American Recovery and Reinvestment Act of 2009 directed the “meaningful use” of EHR systems for hospital and physician practice settings and provided for financial incentives from the CMS to providers who adopt and use EHRs that meet the meaningful use standards. “Meaningful use” refers to a complex set of capabilities and standards to be met by EHR use in a series of three stages over several years. The first stage, year 2011-2012, forms the foundation for electronic data capture and information sharing and includes 5 priorities (U.S. DHHS, 2012b):
Information Technology in the Clinical Setting
Chapter Overview
Health Information Technology Across The Globe
Health Information Technology in the United States
Electronic Health Records
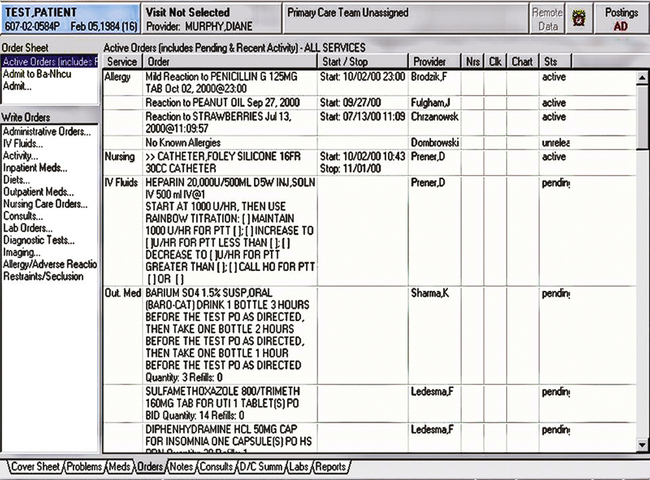
Key Functions of the EHR
Health information and data
Information to make sound clinical decisions, such as past medical history, laboratory tests, allergies, current medications, and consent forms
Results management
Electronic reports of laboratory results and radiology procedures with automated display of previous results; electronic consultation reports
Order entry and order management
Computerized provider order entry with or without decision support to eliminate lost orders and illegible handwriting, generate related orders automatically, monitor for duplicate or contradictory orders, and reduce time to fill orders
Decision support
Enhance clinical performance by providing reminders about preventive practices, such as immunizations, drug alerts for dosing and interactions, and clinical decision making
Electronic communication and connectivity
Electronic communication between health care team members and other care partners, such as radiology and laboratory personnel, and connectivity to the patient record across multiple care settings
Patient support
Computer-based patient education and home monitoring where applicable
Administrative processes
Scheduling systems, billing and claims management, insurance eligibility, and inventory management
Reporting and population health management
Meet public and private sector reporting requirements at the federal, state, and local levels; address internal quality improvement initiatives
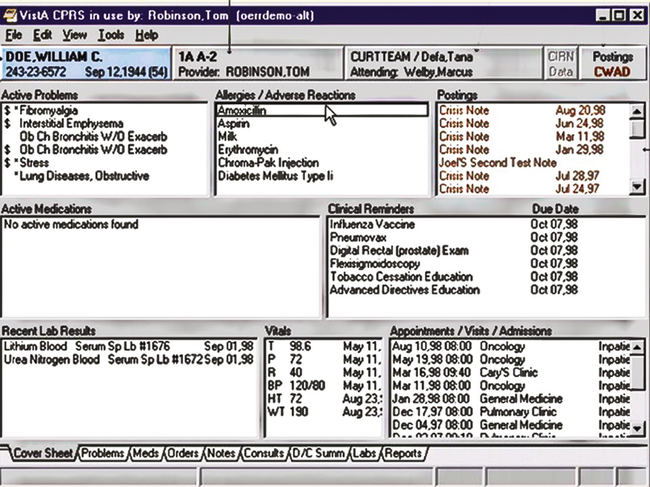
EHR Data Management
Security
EHRs and “Meaningful Use”
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Information Technology in the Clinical Setting
Get Clinical Tree app for offline access