Infection Prevention and Control
Objectives
• Explain the relationship between the chain and transmission of infection.
• Give an example of preventing infection for each element of the infection chain.
• Identify the normal defenses of the body against infection.
• Discuss the events in the inflammatory response.
• Identify patients most at risk for infection.
• Describe the signs/symptoms of a localized infection and those of a systemic infection.
• Explain conditions that promote the transmission of health care–associated infection.
• Explain the difference between medical and surgical asepsis.
• Explain the rationale for standard precautions.
• Perform proper procedures for hand hygiene.
• Explain how infection control measures differ in the home versus the hospital.
• Properly don a surgical mask, sterile gown, and sterile gloves.
• Explain procedures for each isolation category.
• Understand the definition of occupational exposure.
Key Terms
Aerobic, p. 399
Anaerobic, p. 399
Asepsis, p. 410
Asymptomatic, p. 399
Bactericidal, p. 400
Bacteriostasis, p. 400
Broad-spectrum antibiotics, p. 402
Colonization, p. 399
Communicable disease, p. 399
Cough etiquette, p. 413
Disinfection, p. 412
Edema, p. 403
Endogenous infection, p. 403
Epidemiology, p. 421
Exogenous infection, p. 403
Exudates, p. 403
Granulation tissue, p. 403
Hand hygiene, p. 410
Handwashing, p. 410
Health care–associated infections (HAIs), p. 403
Iatrogenic infections, p. 403
Immunocompromised, p. 399
Infection, p. 399
Infectious, p. 399
Invasive, p. 398
Leukocytosis, p. 403
Localized, p. 401
Medical asepsis, p. 410
Microorganisms, p. 399
Necrotic, p. 402
Normal floras, p. 402
Pathogens, p. 399
Phagocytosis, p. 403
Purulent, p. 403
Reservoir, p. 399
Sanguineous, p. 403
Serous, p. 403
Standard precautions, p. 410
Sterile field, p. 423
Sterilization, p. 412
Suprainfection, p. 402
Surgical asepsis, p. 421
Susceptibility, p. 401
Suppurative, p. 407
Symptomatic, p. 399
Systemic, p. 401
Vector, p. 401
Virulence, p. 399
![]()
The incidence of patients developing infections as the direct result of contact during health care is increasing. Current trends, public awareness, and rising costs of health care have increased the importance of infection prevention and control. The Joint Commission (TJC) (2011) views this as a patient safety issue. Infection prevention and control are essential for creating a safe health care environment for patients, families, and staff. Nurses play a primary role in infection prevention and control. Patients in all health care settings are at risk for acquiring infections because of lower resistance to pathogens; increased exposure to pathogens, some of which may be resistant to most antibiotics; and invasive procedures. Health care workers are at risk for exposure to infections as a result of contact with patient blood, body fluids, and contaminated equipment and surfaces. By practicing basic infection prevention and control techniques, you avoid spreading pathogens to patients and sustaining an exposure when providing direct care.
Patients and their families need to be able to recognize sources of infection and understand measures used to protect themselves. Patient teaching must include basic information about infection, the various modes of transmission, and appropriate methods of prevention.
Health care workers protect themselves from contact with infectious material, sharps injury, and/or exposure to a communicable disease by applying knowledge of the infectious process and using appropriate personal protective equipment (PPE). Diseases such as hepatitis B and C, human immunodeficiency virus (HIV) infection, acquired immunodeficiency syndrome (AIDS), tuberculosis (TB), and multidrug-resistant organisms require a greater emphasis on infection prevention and control techniques (Centers for Disease Control and Prevention [CDC], 2004, 2006).
Scientific Knowledge Base
Nature of Infection
An infection is the invasion of a susceptible host by pathogens or microorganisms, resulting in disease. It is important to know the difference between an infection and colonization. Colonization is the presence and growth of microorganisms within a host but without tissue invasion or damage (Tweeten, 2009). Disease or infection results only if the pathogens multiply and alter normal tissue function. Some infectious diseases such as viral meningitis and pneumonia have a low or no risk for transmission. Although these illnesses can be serious for the patient, they do not pose a risk to others, including caregivers.
If an infectious disease can be transmitted directly from one person to another, it is termed a communicable disease (Tweeten, 2009). If the pathogens multiply and cause clinical signs and symptoms, the infection is symptomatic. If clinical signs and symptoms are not present, the illness is termed asymptomatic. Hepatitis C is an example of a communicable disease that can be asymptomatic. It is most efficiently transmitted through the direct passage of blood into the skin from a percutaneous exposure, even if the source patient is asymptomatic (CDC, 2010c).
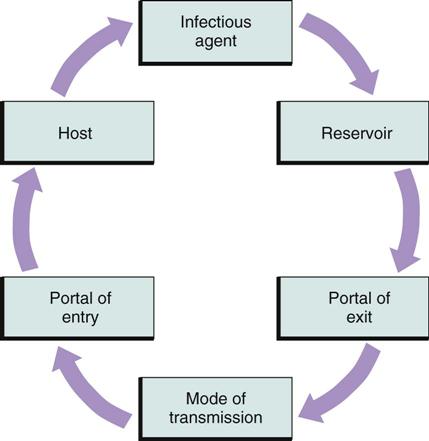
Chain of Infection
The presence of a pathogen does not mean that an infection will occur. Infection occurs in a cycle that depends on the presence of all of the following elements:
• An infectious agent or pathogen
• A reservoir or source for pathogen growth
• A port of exit from the reservoir
Infection can develop if this chain remains uninterrupted (Fig. 28-1). Preventing infections involves breaking the chain of infection.
Infectious Agent.
Microorganisms include bacteria, viruses, fungi, and protozoa (Table 28-1). Microorganisms on the skin are either resident or transient flora. Resident organisms (normal flora) are permanent residents of the skin, where they survive and multiply without causing illness (CDC, 2002; WHO, 2009). The potential for microorganisms or parasites to cause disease depends on the number of microorganisms present; their virulence, or ability to produce disease; their ability to enter and survive in the host; and the susceptibility of the host. Resident skin microorganisms are not virulent. However, they sometimes cause serious infection when surgery or other invasive procedures allow them to enter deep tissues or when a patient is severely immunocompromised (has an impaired immune system).
TABLE 28-1
Common Pathogens and Some Infections or Diseases They Produce
| ORGANISM | MAJOR RESERVOIR(S) | MAJOR INFECTIONS/DISEASES |
| Bacteria | ||
| Escherichia coli | Colon | Gastroenteritis, urinary tract infection |
| Staphylococcus aureus | Skin, hair, anterior nares, mouth | Wound infection, pneumonia, food poisoning, cellulitis |
| Streptococcus (beta-hemolytic group A) organisms | Oropharynx, skin, perianal area | “Strep throat,” rheumatic fever, scarlet fever, impetigo, wound infection |
| Streptococcus (beta-hemolytic group B) organisms | Adult genitalia | Urinary tract infection, wound infection, postpartum sepsis, neonatal sepsis |
| Mycobacterium tuberculosis | Droplet nuclei from lungs, larynx | Tuberculosis |
| Neisseria gonorrhoeae | Genitourinary tract, rectum, mouth | Gonorrhea, pelvic inflammatory disease, infectious arthritis, conjunctivitis |
| Rickettsia rickettsii | Wood tick | Rocky Mountain spotted fever |
| Staphylococcus epidermidis | Skin | Wound infection, bacteremia |
| Viruses | ||
| Hepatitis A virus | Feces | Hepatitis A |
| Hepatitis B virus | Blood and certain body fluids, sexual contact | Hepatitis B |
| Hepatitis C virus | Blood, certain body fluids, sexual contact | Hepatitis C |
| Herpes simplex virus (type 1) | Lesions of mouth or skin, saliva, genitalia | Cold sores, aseptic meningitis, sexually transmitted disease, herpetic whitlow |
| Human immunodeficiency virus (HIV) | Blood, semen, vaginal secretions via sexual contact | Acquired immunodeficiency syndrome (AIDS) |
| Fungi | ||
| Aspergillus organisms | Soil, dust, mouth, skin, colon, genital tract | Aspergillosis, pneumonia, sepsis |
| Candida albicans | Mouth, skin, colon, genital tract | Candidiasis, pneumonia, sepsis |
| Protozoa | ||
| Plasmodium falciparum | Blood | Malaria |
Modified from Moore V: Microbiology basics. In Carrico R, editor: APIC text of infection control and epidemiology, Washington, DC, 2009, Association for Professionals in Infection Control and Epidemiology.
Transient microorganisms attach to the skin when a person has contact with another person or object during normal activities. For example, when you touch a contaminated gauze dressing, transient bacteria adhere to your skin. These organisms may be readily transmitted unless removed using hand hygiene (Larson, 2005). If hands are visibly soiled with proteinaceous material, washing with soap and water is the preferred practice. If hands are not visibly soiled, use of an alcohol-based hand product or handwashing with soap and water is acceptable for disinfecting hands of health care workers (CDC, 2002; WHO, 2009).
Reservoir.
A reservoir is a place where microorganisms survive, multiply, and await transfer to a susceptible host. Common reservoirs are humans and animals (hosts), insects, food, water, and organic matter on inanimate surfaces (fomites). Frequent reservoirs for health care–associated infections (HAIs) include health care workers, especially their hands; patients; equipment; and the environment. Human reservoirs are divided into two types: those with acute or symptomatic disease and those who show no signs of disease but are carriers of it. Humans can transmit microorganisms in either case. Animals, food, water, insects, and inanimate objects can also be reservoirs for infectious organisms. To thrive, organisms require a proper environment, including appropriate food, oxygen, water, temperature, pH, and light.
Food.
Microorganisms require nourishment. Some such as Clostridium perfringens, the microbe that causes gas gangrene, thrive on organic matter. Others such as Escherichia coli consume undigested foodstuff in the bowel. Carbon dioxide and inorganic material such as soil provide nourishment for other organisms.
Oxygen.
Aerobic bacteria require oxygen for survival and for multiplication sufficient to cause disease. Aerobic organisms cause more infections in humans than anaerobic organisms. An example of an aerobic organism is Staphylococcus aureus. Anaerobic bacteria thrive where little or no free oxygen is available. Infections deep within the pleural cavity, in a joint, or in a deep sinus tract are typically caused by anaerobes. An example of an anaerobic organism is Clostridium difficile, an organism that causes antibiotic-induced diarrhea.
Water.
Most organisms require water or moisture for survival. For example, a frequent place for microorganisms is the moist drainage from a surgical wound. Some bacteria assume a form, called a spore, which is resistant to drying. A common spore-forming bacterium is C. difficile, an organism that causes antibiotic-induced diarrhea.
Temperature.
Microorganisms can live only in certain temperature ranges. Each species of bacteria has a specific temperature at which it grows best. The ideal temperature for most human pathogens is 20° to 43° C (68° to 109° F). For example, Legionella pneumophila grows best in water at 25° to 42° C (77° to 108° F) (Moore, 2009; Ritter, 2005). Cold temperatures tend to prevent growth and reproduction of bacteria (bacteriostasis). A temperature or chemical that destroys bacteria is bactericidal.
pH.
The acidity of an environment determines the viability of microorganisms. Most microorganisms prefer an environment within a pH range of 5.0 to 7.0. Bacteria in particular thrive in urine with an alkaline pH.
Light.
Microorganisms thrive in dark environments such as those under dressings and within body cavities.
Port of Exit.
After microorganisms find a site to grow and multiply, they need to find a port of exit if they are to enter another host and cause disease. Ports of exit include sites such as blood, skin and mucous membranes, respiratory tract, genitourinary tract, gastrointestinal tract, and transplacental (mother to fetus).
Skin and Mucous Membranes.
The skin is considered a port of exit because any break in the integrity of the skin and mucous membranes allows pathogens to exit the body. This may be exhibited by the creation of purulent drainage. The presence of purulent drainage is a potential port of exit.
Respiratory Tract.
Pathogens that infect the respiratory tract such as the influenza virus are released from the body when an infected person sneezes or coughs.
Urinary Tract.
Normally urine is sterile. However, when a patient has a urinary tract infection (UTI), microorganisms exit during urination.
Gastrointestinal Tract.
The mouth is one of the most bacterially contaminated sites of the human body, but most of the organisms are normal floras. Organisms that are normal floras in one person can be pathogens in another. For example, organisms exit when a person expectorates saliva. In addition, gastrointestinal ports of exit include bowel elimination, drainage of bile via surgical wounds, or drainage tubes.
Reproductive Tract.
Organisms such as Neisseria gonorrhoeae and HIV exit through a man’s urethral meatus or a woman’s vaginal canal during sexual contact.
Blood.
The blood is normally a sterile body fluid; however, in the case of communicable diseases such as hepatitis B or C or HIV, it becomes a reservoir for pathogens.
Modes of Transmission.
Each disease has a specific mode of transmission. Many times you are able to do little about the infectious agent or the susceptible host, but by practicing infection prevention and control techniques such as hand hygiene, you interrupt the mode of transmission (Box 28-1). The same microorganism is sometimes transmitted by more than one route. For example, varicella zoster (chickenpox) is spread by the airborne route in droplet nuclei or by direct contact.
The major route of transmission for pathogens identified in the health care setting is the unwashed hands of the health care worker (CDC, 2002; Cipriano, 2007; WHO, 2009). Equipment used within the environment (e.g., a stethoscope, blood pressure cuff, or bedside commode) often becomes a source for the transmission of pathogens.
Port of Entry.
Organisms enter the body through the same routes they use for exiting. For example, when a needle pierces a patient’s skin, organisms enter the body if proper skin preparation is not performed first. Factors such as a depressed immune system that reduce body defenses enhance the chances of pathogens entering the body.
Susceptible Host.
Susceptibility to an infectious agent depends on the individual’s degree of resistance to pathogens. Although everyone is constantly in contact with large numbers of microorganisms, an infection does not develop until an individual becomes susceptible to the strength and numbers of the microorganisms. A person’s natural defenses against infection and certain risk factors (e.g., age, nutritional status, presence of chronic disease, trauma, and smoking) affect susceptibility (resistance) (Fardo, 2009). Organisms such as S. aureus with resistance to key antibiotics are becoming more common in all health care settings, but especially acute care. The increased resistance is associated with the frequent and sometimes inappropriate use of antibiotics over the years in all settings (i.e., acute care, ambulatory care, clinics, and long-term care) (Arnold, 2009).
The Infectious Process
By understanding the chain of infection, you have knowledge that is vital in preventing infections. When the patient acquires an infection, observe for signs and symptoms of infection and take appropriate actions to prevent its spread. Infections follow a progressive course (Box 28-2).
If an infection is localized (e.g., a wound infection), the patient usually experiences localized symptoms such as pain, tenderness, and redness at the wound site. Use standard precautions, appropriate PPE, and hand hygiene when assessing the wound. The use of these precautions and hand hygiene blocks the spread of infection to other sites or other patients. An infection that affects the entire body instead of just a single organ or part is systemic and can become fatal if undetected and untreated.
The course of an infection influences the level of nursing care provided. The nurse is responsible for properly administering antibiotics, monitoring the response to drug therapy (see Chapter 31), using proper hand hygiene, and standard precautions. Supportive therapy includes providing adequate nutrition and rest to bolster defenses against the infectious process. The course of care for the patient often has additional effects on body systems affected by the infection.
Defenses Against Infection
The body has natural defenses that protect against infection. Normal floras, body system defenses, and inflammation are all nonspecific defenses that protect against microorganisms regardless of prior exposure. If any body defenses fail, an infection usually occurs and leads to a serious health problem.
Normal Floras.
The body normally contains microorganisms that reside on the surface and deep layers of skin, in the saliva and oral mucosa, and in the gastrointestinal and genitourinary tracts. A person normally excretes trillions of microbes daily through the intestines. Normal floras do not usually cause disease when residing in their usual area of the body but instead participate in maintaining health.
Normal floras of the large intestine exist in large numbers without causing illness. They also secrete antibacterial substances within the walls of the intestine. The normal floras of the skin exert a protective, bactericidal action that kills organisms landing on the skin. The mouth and pharynx are also protected by floras that impair growth of invading microbes. Normal floras maintain a sensitive balance with other microorganisms to prevent infection. Any factor that disrupts this balance places a person at increased risk for acquiring a disease. For example, the use of broad-spectrum antibiotics for the treatment of infection can lead to suprainfection. A suprainfection develops when broad-spectrum antibiotics eliminate a wide range of normal flora organisms, not just those causing infection. When normal bacterial floras are eliminated, body defenses are reduced, which allows for disease-producing microorganisms to multiply, causing illness (Arnold, 2009).
Body System Defenses.
A number of body organ systems have unique defenses against infection (Table 28-2). The skin, respiratory tract, and gastrointestinal tract are easily accessible to microorganisms. Pathogenic organisms can adhere to the surface skin, be inhaled into the lungs, or be ingested with food. Each organ system has defense mechanisms physiologically suited to its specific structure and function. For example, the lungs cannot completely control the entrance of microorganisms. However, the airways are lined with moist mucous membranes and hairlike projections, or cilia, that rhythmically beat to move mucus or cellular debris up to the pharynx to be expelled through swallowing.
TABLE 28-2
Normal Defense Mechanisms Against Infection
| DEFENSE MECHANISMS | ACTION | FACTORS THAT MAY ALTER DEFENSE MECHANISMS |
| Skin | ||
| Intact multilayered surface (first line of defense body against infection) | Provides barrier to microorganisms and antibacterial activity | Cuts, abrasions, puncture wounds, areas of maceration |
| Shedding of outer layer of skin cells | Removes organisms that adhere to outer layers of skin | Failure to bathe regularly, improper handwashing technique |
| Sebum | Contains fatty acid that kills some bacteria | Excessive bathing |
| Mouth | ||
| Intact multilayered mucosa | Provides mechanical barrier to microorganisms | Lacerations, trauma, extracted teeth |
| Saliva | Washes away particles containing microorganisms | Poor oral hygiene, dehydration |
| Contains microbial inhibitors (e.g., lysozyme) | ||
| Eye | ||
| Tearing and blinking | Provides mechanisms to reduce entry (blinking) or assist in washing away (tearing) particles containing pathogens, thus reducing dose of organisms | Injury, exposure—splash/splatter of blood or other potentially infectious material into eye |
| Respiratory Tract | ||
| Cilia lining upper airway, coated by mucus | Traps inhaled microbes and sweeps them outward in mucus to be expectorated or swallowed | Smoking, high concentration of oxygen and carbon dioxide, decreased humidity, cold air |
| Macrophages | Engulf and destroy microorganisms that reach alveoli of lung | Smoking |
| Urinary Tract | ||
| Flushing action of urine flow | Washes away microorganisms on lining of bladder and urethra | Obstruction to normal flow by urinary catheter placement, obstruction from growth or tumor, delayed micturition |
| Intact multilayered epithelium | Provides barrier to microorganisms | Introduction of urinary catheter, continual movement of catheter in urethra |
| Gastrointestinal Tract | ||
| Acidity of gastric secretions | Prevents retention of bacterial contents | Administration of antacids |
| Rapid peristalsis in small intestine | Delayed motility resulting from impaction of fecal contents in large bowel or mechanical obstruction by masses | |
| Vagina | ||
| At puberty, normal flora causing vaginal secretions to achieve low pH | Inhibit growth of many microorganisms | Antibiotics and oral contraceptives disrupting normal flora |
Inflammation.
The cellular response of the body to injury, infection, or irritation is termed inflammation. Inflammation is a protective vascular reaction that delivers fluid, blood products, and nutrients to an area of injury. The process neutralizes and eliminates pathogens or dead (necrotic) tissues and establishes a means of repairing body cells and tissues. Signs of localized inflammation include swelling, redness, heat, pain or tenderness, and loss of function in the affected body part. When inflammation becomes systemic, other signs and symptoms develop, including fever, leukocytosis, malaise, anorexia, nausea, vomiting, lymph node enlargement, or organ failure.
Physical agents, chemical agents, or microorganisms trigger the inflammatory response. Mechanical trauma, temperature extremes, and radiation are examples of physical agents. Chemical agents include external and internal irritants such as harsh poisons or gastric acid. Sometimes microorganisms also trigger this response.
After tissues are injured, a series of well-coordinated events occurs. The inflammatory response includes the following:
Vascular and Cellular Responses.
Acute inflammation is an immediate response to cellular injury. Rapid vasodilation occurs, allowing more blood near the location of the injury. The increase in local blood flow causes the redness and localized warmth at the site of inflammation.
Injury causes tissue damage and possibly necrosis. As a result the body releases chemical mediators that increase the permeability of small blood vessels; and fluid, protein, and cells enter interstitial spaces. The accumulation of fluid appears as localized swelling (edema). Another sign of inflammation is pain. The swelling of inflamed tissues increases pressure on nerve endings, causing pain. As a result of physiological changes occurring with inflammation, the involved body part may have a temporary loss of function. For example, a localized infection of the hand causes the fingers to become swollen, painful, and discolored. Joints become stiff as a result of swelling, but function of the fingers returns when inflammation subsides.
The cellular response of inflammation involves white blood cells (WBCs) arriving at the site. WBCs pass through blood vessels and into the tissues. Phagocytosis is a process that involves the destruction and absorption of bacteria. Through the process of phagocytosis, specialized WBCs, called neutrophils and monocytes, ingest and destroy microorganisms or other small particles. If inflammation becomes systemic, other signs and symptoms develop. Leukocytosis, or an increase in the number of circulating WBCs, is the response of the body to WBCs leaving blood vessels. A serum WBC count is normally 5,000 to 10,000/mm3 but typically rise to 15,000 to 20,000/mm3 and higher during inflammation. Fever is caused by phagocytic release of pyrogens from bacterial cells, which causes a rise in the hypothalamic set point (see Chapter 29).
Inflammatory Exudate.
Accumulation of fluid and dead tissue cells and WBCs forms an exudate at the site of inflammation. Exudate may be serous (clear, like plasma), sanguineous (containing red blood cells), or purulent (containing WBCs and bacteria). Usually the exudate is cleared away through lymphatic drainage. Platelets and plasma proteins such as fibrinogen form a meshlike matrix at the site of inflammation to prevent its spread.
Tissue Repair.
When there is injury to tissue cells, healing involves the defensive, reconstructive, and maturative stages (see Chapter 48). Damaged cells are eventually replaced with healthy new cells. The new cells undergo a gradual maturation until they take on the same structural characteristics and appearance as the previous cells. If inflammation is chronic, tissue defects sometimes fill with fragile granulation tissue. Granulation tissue is not as strong as tissue collagen and assumes the form of scar tissue.
Health Care–Associated Infections
Patients in health care settings, especially hospitals and long-term care facilities, have an increased risk of acquiring infections. Health care–associated infections (HAIs), formerly called nosocomial or health care–acquired infections, result from the delivery of health services in a health care facility. They occur as the result of invasive procedures, antibiotic administration, the presence of multidrug-resistant organisms, and breaks in infection prevention and control activities.
Patients who develop HAIs often have multiple illnesses, are older adults, and are poorly nourished; thus they are more susceptible to infections. In addition, many patients have a lowered resistance to infection because of underlying medical conditions (e.g., diabetes mellitus or malignancies) that impair or damage the immune response of the body. Invasive treatment devices such as intravenous (IV) catheters or indwelling urinary catheters impair or bypass the natural defenses of the body against microorganisms. Critical illness increases patients’ susceptibility to infections, especially multidrug-resistant bacteria. Meticulous hand hygiene practices, the use of chlorhexidine washes, and other advances in intensive care unit (ICU) infection prevention help to prevent these infections (Doyle et al., 2011).
Iatrogenic infections are a type of HAI from a diagnostic or therapeutic procedure. For example, procedures such as a bronchoscopy and treatment with broad-spectrum antibiotics increase the risk for certain infections (Arnold, 2009; Stricof, 2009). Use critical thinking when practicing aseptic techniques and follow basic infection prevention and control policies and procedures to reduce the risk of HAIs. Always consider the patient’s risks for infection and anticipate how the approach to care increases or decreases the risk.
Health care–associated infections are exogenous or endogenous. An exogenous infection comes from microorganisms found outside the individual such as Salmonella, Clostridium tetani, and Aspergillus. They do not exist as normal floras. Endogenous infection occurs when part of the patient’s flora becomes altered and an overgrowth results (e.g., staphylococci, enterococci, yeasts, and streptococci). This often happens when a patient receives broad-spectrum antibiotics that alter the normal floras. When sufficient numbers of microorganisms normally found in one body site move to another site, an endogenous infection develops. The number of microorganisms needed to cause a health care–associated infection depends on the virulence of the organism, the susceptibility of the host, and the body site affected.
The number of health care employees having direct contact with a patient, the type and number of invasive procedures, the therapy received, and the length of hospitalization influence the risk of infection. Major sites for HAIs include surgical or traumatic wounds, urinary and respiratory tracts, and the bloodstream (Box 28-3).
Health care–associated infections significantly increase costs of health care. Older adults have increased susceptibility to these infections because of their affinity to chronic disease and the aging process itself (Box 28-4). Extended stays in health care institutions, increased disability, increased costs of antibiotics, and prolonged recovery times add to the expenses both of the patient and the health care institution and funding bodies (e.g., Medicare). Often costs for HAIs are not reimbursed; as a result, prevention has a beneficial financial impact and is an important part of managed care. TJC (2011) lists several national safety goals focusing on the care of older adults (e.g., ensuring that older adults receive influenza and pneumonia vaccine or preventing infection after surgery).
Nursing Knowledge Base
Body substances such as feces, urine, and wound drainage contain potentially infectious microorganisms. Health care workers are at risk for exposure to microorganisms in the hospital and/or home setting (Fauerbach, 2009). They follow specific infection prevention practices to reduce the risk of cross-contamination and transmission to other patients when caring for a patient with a known or suspected infection (CDC, 2007).
The experience of having a serious infection creates feelings of anxiety, frustration, loneliness, and anger in patients and/or their families (Calfree et al., 2008). These feelings worsen when patients are isolated to prevent transmission of a microorganism to other patients or health care staff. Isolation disrupts normal social relationships with visitors and caregivers. Patient safety is usually an additional risk for the patient on isolation precautions (Murphy, 2009). For example, an older patient with dementia is at increased risk for falling when confined in a room with the door closed. When family members fear the possibility of developing the infection, they avoid contact with the patient. Some patients perceive the simple procedures of proper hand hygiene and gown and glove use as evidence of rejection. Help patients and families reduce some of these feelings by discussing the disease process, explaining isolation procedures, and maintaining a friendly, understanding manner.
When establishing a plan of care, it is important for you to know how a patient reacts to an infection or infectious disease. The challenge is to identify and support behaviors that maintain human health or prevent infection.
Factors Influencing Infection Prevention and Control
Multiple factors influence a patient’s susceptibility to infection. It is important to understand how each of these factors alone or in combination increases this risk. When more than one factor is present, the patient’s susceptibility often increases, which affects length of stay, recovery time, and/or overall level of health following an illness. Understanding these factors assists in assessing and caring for a patient who has an infection or is at risk for one.
Age.
Throughout life, susceptibility to infection changes. For example, an infant has immature defenses against infection. Born with only the antibodies provided by the mother, the infant’s immune system is incapable of producing the necessary immunoglobulins and WBCs to adequately fight some infections. However, breastfed infants often have greater immunity than bottle-fed infants because they receive their mother’s antibodies through the breast milk. As the child grows, the immune system matures; but the child is still susceptible to organisms that cause the common cold, intestinal infections, and infectious diseases such as mumps, measles, and chickenpox (if not vaccinated).
The young or middle-age adult has refined defenses against infection. Viruses are the most common cause of communicable illness in young or middle-age adults. Since 2000 there has been a major effort to vaccinate all children against all infectious diseases for which vaccines are available. Vaccine-preventable disease levels are at or near record lows (CDC, 2011). For example; hepatitis B infection in children and adolescents decreased by 89% in 2005 (CDC, 2005b).
Defenses against infection change with aging (Lesser, Paiusi, and Leips, 2006). The immune response, particularly cell-mediated immunity, declines. Older adults also undergo alterations in the structure and function of the skin, urinary tract, and lungs. For example, the skin loses its turgor, and the epithelium thins. As a result it is easier to tear or abrade the skin, which increases the potential for invasion by pathogens. In addition, older adults who are hospitalized or reside in an assisted-living or residential care facility are at risk for airborne infections. Ensuring that health care workers are vaccinated against influenza reduces the transmission of this illness in older adults (Thomas et al., 2010).
Nutritional Status.
A patient’s nutritional health directly influences susceptibility to infection. A reduction in the intake of protein and other nutrients such as carbohydrates and fats reduces body defenses against infection and impairs wound healing (see Chapter 48). Patients with illnesses or problems that increase protein requirements, such as extensive burns and conditions causing fever, are at further risk. Patients who have undergone surgery, for example, require increased protein. A thorough diet history is necessary. Determine a patient’s normal daily nutrient intake and whether preexisting problems such as nausea, impaired swallowing, or oral pain alter food intake. Confer with a dietitian to assist in calculating the calorie count of foods ingested.
Stress.
The body responds to emotional or physical stress by the general adaptation syndrome (see Chapter 37). During the alarm stage the basal metabolic rate increases as the body uses energy stores. Adrenocorticotropic hormone increases serum glucose levels and decreases unnecessary antiinflammatory responses through the release of cortisone. If stress continues or becomes intense, elevated cortisone levels result in decreased resistance to infection. Continued stress leads to exhaustion, which causes depletion in energy stores, and the body has no resistance to invading organisms. The same conditions that increase nutritional requirements such as surgery or trauma also increase physiological stress.
Disease Process.
Patients with diseases of the immune system are at particular risk for infection. Leukemia, AIDS, lymphoma, and aplastic anemia are conditions that compromise a host by weakening defenses against infectious organisms. For example, patients with leukemia are unable to produce enough WBCs to ward off infection. Patients with HIV are often unable to ward off simple infections and are prone to opportunistic infections.
Patients with chronic diseases such as diabetes mellitus and multiple sclerosis are also more susceptible to infection because of general debilitation and nutritional impairment. Diseases that impair body system defenses such as emphysema and bronchitis (which impair ciliary action and thicken mucus), cancer (which alters the immune response), and peripheral vascular disease (which reduces blood flow to injured tissues) increase susceptibility to infection. Patients with burns have a high susceptibility to infection because of the damage to skin surfaces. The greater the depth and extent of the burns, the higher the risk for infection.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process, thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care. Determine how the patient feels about the illness or risk for infection. Assess his or her defense mechanisms, susceptibility, and knowledge of how infections are transmitted (Table 28-3). Conduct a review of systems and travel history with the patient and family to reveal any risks for exposure to a communicable disease. Immunization and vaccination history are also very useful. It is important to be thorough in assessing a patient’s clinical condition. A medication history is necessary to identify medications that increase a patient’s susceptibility to infection. An analysis of laboratory findings provides information about a patient’s defense against infection. The early recognition of infection or risk factors helps you make the correct nursing diagnosis and establish a treatment plan.
TABLE 28-3
Assessing the Risk of Infection in Adults
| RISK FACTOR | CAUSES | OUTCOME |
| Chronic disease | COPD, heart failure, diabetes | Pneumonia, skin breakdown, venous stasis ulcers |
| Lifestyle—high-risk behaviors | Exposure to communicable/infectious diseases, use of IV drugs and other drugs/substances | STIs, HIV, HBV, HCV, opportunistic infections, viral infections, yeast infections, liver failure |
| Occupation | Miner, unemployed, homeless | Black lung disease, pneumonia, TB, poor nutritional intake, lack of access to medical care, stress |
| Diagnostic procedures | Invasive radiology, transplant | Multiple IV lines, immunosuppressive drugs |
| Heredity | Sickle cell disease, diabetes | Anemia, delayed healing |
| Travel history | West Nile virus, SARS, avian flu, Hantavirus | Meningitis, acute respiratory distress |
| Trauma | Fractures, internal bleeding | Sepsis, secondary infection |
| Nutrition | Obesity, anorexia | Impaired immune response |
Modified from Tweeten SM: General principles of epidemiology. In Carrico R, editor: APIC text of infection control and epidemiology, Washington, DC, 2009, Association for Professionals in Infection Control and Epidemiology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


