Incremental Changes in Culture, Workforce, and Products Reduce Hospital-Acquired Pressure Ulcers in the Intensive Care Setting
Barbara Twombly BSN, RN, WOCN1
Amy Stuck MSN, RN2
Kathleen Blechertas PT, WCC3
Kathleen Reilly BSN, RN4
Nathan Dollick BSN, RN, CCRN5
1Intensive Care Wound Care Nurse
Twombly.Barbara@scrippshealth.org
2Intensive Care Unit Advanced Practice Nurse
3Manager, Physical Therapy
4Project Manager, Performance Improvement
5Patient Care Manager, SICU
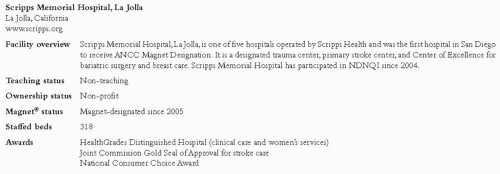
Scripps Memorial Hospital, La Jolla La Jolla, California
www.scripps.org
Case Study Highlights
Structural changes (e.g., unit redesign, fewer agency nurses) preceded numerous practice changes focused on creating a culture of prevention. With persistent incremental interventions targeting unit culture, workforce, products, and staff education, annual hospital-acquired pressure ulcer (HAPU) rates fell from over 20% to under 7% on the surgical intensive care unit.
Overview of Pressure Ulcer Prevention Efforts
HAPU rates in the intensive care units at Scripps Memorial Hospital, La Jolla (SMH-LJ), were near the 90th percentile for NDNQI® and the Collaborative Alliance for Nursing Outcomes (CalNOC) in 2005 and 2006. The Chief Nurse Executive, Chief Financial Officer, and Performance Improvement Director worked to develop a strategic plan to address the unit
structure and workforce issues that were contributing to high HAPU rates. Subsequently, a series of changes in daily practice were used to promote a culture of HAPU prevention. With continual practice and workforce and product improvements, HAPU rates have successfully been reduced. (See Figure 1.)
structure and workforce issues that were contributing to high HAPU rates. Subsequently, a series of changes in daily practice were used to promote a culture of HAPU prevention. With continual practice and workforce and product improvements, HAPU rates have successfully been reduced. (See Figure 1.)
Structural Changes Pave the Way for Improvement
Before April 2007, the intensive care units at SMH-LJ were considered one unit, led by one manager who oversaw 41 beds and more than 120 employees. The manager’s effectiveness was limited by a large span of control covering multiple, geographically separate units. This management structure did not allow for clear communication of expectations or realistic monitoring for accountability. Even though data on hospital-acquired pressure ulcers were available and communicated to staff, several factors contributed to the challenge of reducing pressure ulcers in the units. First, 30% of the intensive care unit (ICU) nurses were contracted travelers who had little organizational understanding, buy-in, or accountability. Second, experienced core nurses were taxed with frequently orienting the incoming traveler staff. Additionally, expert wound nurse resources were limited. Finally, the staff in the ICU did not consider skin integrity a priority in the critically ill patient and often perceived pressure ulcers as unavoidable.
Despite several approaches taken to decrease the rate of pressure ulcers in the ICU, the rates were not improving. Hospital administration reviewed the HAPU data, met with the manager and staff, who together developed a strategic plan to make improvements in the ICU. Four key areas were targeted for change.
Unit Design:
The intensive care unit was separated into three specialty units in the spring of 2007 and two additional managers were hired. This improved managerial effectiveness and increased staff expertise for a specific patient population.
Workforce:
In order to eliminate the use of travelers, administration made a commitment to hire Student Nurse Externs (SNEs) with the expectation that a majority of these students would remain with SMH-LJ after graduation. SNEs are baccalaureate senior nursing students
who participate in a work study program under the guidance and preceptorship of a critical care RN. Additionally, managers in the medical-surgical areas were instructed to over-hire RNs by 20% with the understanding that they would be “feeder” units for the ICU intern training program. The intern training program, previously offered annually, was increased to quarterly and the number of RNs accepted for each training session was doubled. To assist staff nurses with reducing pressure ulcers, an ICU Wound Care Nurse was hired two days per week. The Wound Care Nurse initiated “Wound Wednesdays” to evaluate and update skin care plans with each patient’s primary RN.
who participate in a work study program under the guidance and preceptorship of a critical care RN. Additionally, managers in the medical-surgical areas were instructed to over-hire RNs by 20% with the understanding that they would be “feeder” units for the ICU intern training program. The intern training program, previously offered annually, was increased to quarterly and the number of RNs accepted for each training session was doubled. To assist staff nurses with reducing pressure ulcers, an ICU Wound Care Nurse was hired two days per week. The Wound Care Nurse initiated “Wound Wednesdays” to evaluate and update skin care plans with each patient’s primary RN.
Education:
Wound care guidelines were formulated and reviewed with each nurse and placed in every bedside chart. Mandatory basic wound care classes were instituted for all new nursing employees.
Products:
Pressure redistribution mattresses were purchased for all ICU beds.
Causes of HAPU Further Explored
Despite the changes initiated prior to 2007, the annual HAPU rate only decreased from 21.6% to 19.7%, still above the NDNQI mean for comparable hospitals. It was determined that a more focused, in-depth analysis was needed. Over the next two years, the Critical Care Advanced Practice Nurse, ICU Wound Care Nurse, and a representative from Performance Improvement compared HAPU rates to national and state benchmarks, scrutinized data about the locations and stages of wounds, and looked for patterns in wounds associated with medical devices, long procedure times, or inadequate nutrition. In addition, a root cause analysis was conducted on two complex cases. From this analysis, several root causes were uncovered:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree