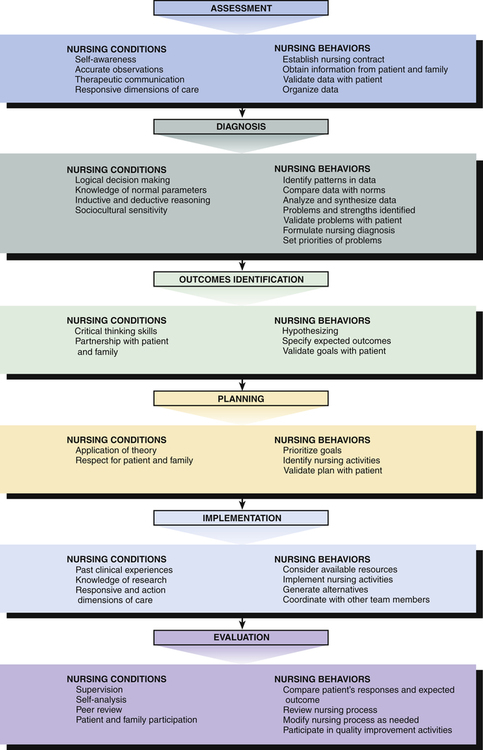
1. Describe the nursing process and the challenges it presents for those working with psychiatric patients. 2. Analyze the conditions and behaviors of the psychiatric nurse for each of the Standards of Practice. 3. Describe how accountability and autonomy relate to the psychiatric nurse’s professional role responsibilities. 4. Analyze the conditions and behaviors of the psychiatric nurse for each of the Standards of Professional Performance. By establishing a therapeutic nurse–patient relationship and using the nursing process, the nurse promotes the patient’s mental health and well-being. This chapter discusses the Standards of Practice and the Standards of Professional Performance as described in Psychiatric–Mental Health Nursing: Scope and Standards of Practice (ANA, 2007). • The Standards of Practice describe what the psychiatric nurse does. • The Standards of Professional Performance describe the context in which the psychiatric nurse performs these activities. The phases of the nursing process as described by the Standards of Practice in Psychiatric–Mental Health Nursing: Scope and Standards of Practice are assessment, diagnosis, outcomes identification, planning, implementation, and evaluation. Validation is part of each step, and all phases may overlap or occur simultaneously. The nursing conditions and nursing behaviors related to each of these phases are shown in Figure 11-1. Each of these phases, as it applies to psychiatric nursing practice, is now described. Identify the patient’s reason for seeking help. Assess for risk factors related to the patient’s safety, including potential for the following: Complete a biopsychosocial assessment of patient needs related to this treatment encounter, including the following: Patient and family appraisal of health and illness Previous episodes of psychiatric care in self and family Physiological coping responses Coping resources, including motivation for treatment and functional supportive relationships Adaptive and maladaptive coping mechanisms Psychosocial and environmental problems Global assessment of functioning In the assessment phase, information is obtained from the patient in a direct and structured manner through observations, interviews, and examinations. An assessment tool or nursing history form can provide a systematic format that becomes part of the patient’s written record. It should include the mental status examination (see Chapter 6). The patient data identified in Standard 1 relate to all parts of the Stuart Stress Adaptation Model used in this text: predisposing factors, precipitating stressors, appraisal of stressors, coping resources, coping mechanisms, and coping responses as described in Chapter 3. The baseline data should include both content and process, and the patient is the ideal source of validation. The nurse should select a private place, free from noise and distraction, in which to interview the patient. Diagnoses should reflect adaptive and maladaptive coping responses based on nursing frameworks such as those of NANDA International (NANDA-I). Diagnoses should incorporate health problems or disease states such as those identified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (American Psychiatric Association [APA], 2000) and the International Classification of Diseases and Related Health Problems (World Health Organization [WHO], 1992). Diagnoses should focus on the phenomena of concern to psychiatric–mental health nurses as described in Box 11-1. After collecting all data, the nurse compares the information with documented norms of health and adaptation. Because standards of behavior are culturally determined, the nurse should consider both the patient’s individual characteristics and the characteristics of the larger social group to which the patient belongs. The nurse then analyzes the data and derives a nursing diagnosis. A nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes (NANDA, 2009). The subject of nursing diagnoses is the patient’s behavioral response to stress. This response may lie anywhere on the coping continuum from adaptive to maladaptive. Phenomena of concern to psychiatric nurses are listed in Box 11-1. A medical diagnosis is the health problem or disease state of the patient. In the medical model of psychiatry the health problems are mental disorders or mental illnesses that are classified in the DSM-IV-TR, which describes the symptoms of mental disorders (APA, 2000). Specific diagnostic criteria are provided for each mental disorder but causes of the disorders are not discussed. Outcomes should be mutually identified with the patient. Outcomes should be identified as clearly and objectively as possible. Well-written outcomes help nurses determine the effectiveness and efficiency of their interventions. Before defining expected outcomes, the nurse must realize that patients often seek treatment with goals of their own. • The patient may view a personal problem as someone else’s behavior. This may be the case of a father who brings his adolescent son in for counseling. The father may view the son as the problem, whereas the adolescent may feel his only problem is his father. One approach to this situation is to focus help on the person who brought the problem into treatment because he “owns” the problem at that moment. The nurse might suggest, “Let’s talk about how I could help you deal with your son. A change in your response might lead to a change in his behavior also.” • The patient may express a problem as a feeling, such as “I’m lonely” or “I’m so unhappy.” Besides trying to help the patient clarify the feeling, the nurse might ask, “What could you do to make yourself feel less alone and more loved by others?” This helps patients see the connection among their actions, thoughts, and feelings and increase their sense of responsibility for themselves. • The patient’s problem may be one of lacking a goal or an idea of exactly what is desired from life. In this case it might be helpful for the nurse to point out that values and goals are not magically discovered but must be created by people for themselves. The patient can then actively explore ways to construct goals or adopt the objectives of a social, service, religious, or political group with whom the patient identifies. • The patient’s problem may be a choice conflict. This is especially common if all the choices are unpleasant, unacceptable, or unrealistic. An example is a couple who wants to divorce but does not want to see their child hurt or suffer the financial hardship that would result. Although undesirable choices cannot be made desirable, the nurse can help patients use the problem-solving process to identify the full range of alternatives available to them. Once overall goals are agreed on, the nurse must state them explicitly. Expected outcomes are derived from diagnoses, guide later nursing actions, and enhance the evaluation of care. Each goal is stated as an observable behavior and includes the period of time in which it is to be accomplished and any other conditions. Expected outcomes can be documented using standardized classification systems, such as the Nursing Outcomes Classification (NOC) (Moorhead et al, 2008). Long- and short-term goals should contribute to the expected outcomes. Following is a sample expected outcome and long- and short-term goals: Expected outcome: Patient will be socially engaged in the community. Long-term goal: The patient will travel about the community independently within 2 months. • At the end of 1 week, the patient will sit on the front steps at home. • At the end of 2 weeks, the patient will walk to the corner and back home. • At the end of 3 weeks, the patient, accompanied by the nurse, will walk in the neighborhood. • At the end of 4 weeks, the patient will walk in the neighborhood alone. • At the end of 6 weeks, the patient will drive her car in the neighborhood. • At the end of 8 weeks, the patient will drive to the mall and meet a friend for dinner. The plan of nursing care must always be individualized for the patient. Planned interventions should be based on current evidence in the field and contemporary clinical psychiatric–mental health nursing practice. Planning is done in collaboration with the patient, the family, and the health care team. Documentation of the plan of care is an essential nursing activity. The psychiatric–mental health registered nurse implements the identified plan. Nursing interventions should reflect a holistic, biopsychosocial approach to patient care. Nursing interventions are implemented in a safe, efficient, and caring manner. The level at which a nurse functions and the interventions implemented are based on the nursing practice acts in one’s state, the nurse’s qualifications (including education, experience, and certification), the caregiving setting, and the nurse’s initiative.
Implementing the Nursing Process
Standards of Practice and Professional Performance
Standards of Practice
Assessment
Standard 1: Assessment
Key Elements
Diagnosis
Standard 2: Diagnosis
Key Elements
Outcomes Identification
Standard 3: Outcomes Identification
Key Elements
Planning
Standard 4: Planning
Key Elements
Implementation
Standard 5: Implementation
Key Elements
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Implementing the Nursing Process: Standards of Practice and Professional Performance
Get Clinical Tree app for offline access