CHAPTER 18 Hematologic/Oncologic Emergencies
I. GENERAL STRATEGY
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC HEMATOLOGIC/ONCOLOGIC EMERGENCIES
A. Disseminated Intravascular Coagulation
Disseminated intravascular coagulation (DIC) is a complex, consumptive, systemic, thrombohemorrhagic disorder involving the inappropriate and accelerated activation of the coagulation cascade that results in thrombosis and subsequent hemorrhage. It is manifested by microvascular coagulation, depletion of clotting factors, and impaired hemostasis. Normal hemostasis is maintained through a balanced system of fibrin production (clot formation) and fibrinolysis (clot breakdown) (Fig. 18-1). The process of thrombosis (abnormal clotting within a blood vessel) is initiated through disruption of the endothelial membrane and/or tissue. Fibrinolysis is the process that breaks down stable fibrin clots. As clots are rapidly lysed, fibrin degradation (split) products (FDP) are released and act as anticoagulants. During this time, the blood’s clotting factors are depleted causing abnormal bleeding. DIC occurs as a complication of, or in association with, other conditions such as sepsis. The overall management goal is to locate and treat the underlying disorder.
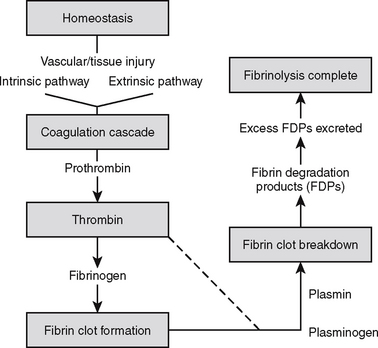
FIGURE 18-1 Normal hemostasis.
(From Itano, J., & Taoka, K. [Eds.]. Core curriculum for oncology nursing [4th ed.]. Philadelphia: Elsevier Saunders in collaboration with Oncology Nursing Society.)
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
B. Hemophilia
Hemophilia is an inherited, sex-linked disorder that occurs most frequently in boys and men. Female family members carry the gene and pass it to their children. There are four types of hemophilia: hemophilia A, hemophilia B, hemophilia C, and von Willebrand’s disease. Hemophilia A (classic hemophilia) is a coagulation disorder caused by a variant form of factor VIII. Severity of the disease is directly related to activity level of factor VIII. Activity level less than 1% is severe and accompanied by spontaneous bleeding. Activity level of 1% to 5% is moderately severe; there is rare spontaneous bleeding but difficulty during surgery or with trauma. Patients with 5% to 10% or greater activity of factor VIII have mild disease with little risk of spontaneous bleeding, but the PTT is prolonged. Bleeding may occur anywhere but characteristically affects joints, deep muscles, urinary tract, and cranial vault (Table 18-1). Immediately following injury, bleeding is usually absent because the initial coagulation step of platelet-plug formation is not affected by hemophilia. Hemophilia B (Christmas disease) results from absence or deficiency of Factor IX. The condition is relatively rare, occurring in 1 in 100,000 persons in the United States, and is clinically indistinguishable from type A, except for treatment. Hemophilia C (Rosenthal’s syndrome) is caused by a deficiency of factor XI. Clinically, it is similar to hemophilia A, but usually has less severe bleeding. Von Willebrand’s disease (angiohemophilia) occurs in male and female patients and is less acute than hemophilia A or B. This type of hemophilia is characterized by defective platelet adherence and decreased factor VIII levels.
Table 18-1 COMMON BLEEDING MANIFESTATIONS IN PATIENTS WITH HEMOPHILIA
| Site | Examples |
|---|---|
| Central nervous system | Intracranial bleeding, most common cause of hemorrhagic death; subdural hematomas occur spontaneously or with minimal trauma |
| Hemarthroses | Joints, leading to chronic atrophy if not treated aggressively |
| Hematomas | Soft tissue or muscles, most serious near the neck (airway compromise), extremities (massive blood loss) |
| Hematuria | Common, but not serious, and source is usually not located |
| Mucocutaneous tissues | Uncommon, but can be spontaneous from oropharynx, gastrointestinal, epistaxis, or hemoptysis; delayed bleeding after dental extraction can be common |
| Pseudotumor | Bone cysts that result from unresolved hematomas; usually surgically removed |
Modified from Tintinalli, J. E., Kelen, G. D., & Stapczynski, J. S. (2004). Emergency medicine: A comprehensive study guide (6th ed., p 1331). New York: McGraw-Hill.
2. Analysis: differential nursing diagnoses/collaborative problems
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


