Health Promotion, Health Maintenance, and Home Health Considerations
Objectives
1. Describe recommended health-maintenance practices, and explain how they change with aging.
2. Discuss the relationship of culture and religion to health practices.
3. Identify how perceptions of aging affect health practices.
4. Describe how health maintenance is affected by cognitive and sensory changes.
5. Discuss the impact of decreased accessibility on health-maintenance practices.
6. Describe methods of assessing health-maintenance practices.
7. Identify older adults who are most at risk for experiencing health-maintenance problems.
8. Identify selected nursing diagnoses related to health-maintenance problems.
11. Differentiate between unpaid and paid home health care providers.
12. Identify the factors to consider when seeking home health care assistance.
Key Terms
health maintenance (p. 75)
health promotion (p. 75)
noncompliance (p. 85)
prophylactic (prō-f -LĂK-t
-LĂK-t k) (p. 77)
k) (p. 77)
 http://evolve.elsevier.com/Wold/geriatric
http://evolve.elsevier.com/Wold/geriatric
As people live longer and the percentage of older adults in the population increases, society faces several major challenges. One of the most significant of these challenges involves meeting the health care needs of the aging population.
Today’s older adults are generally healthier than were the older adults of previous generations. Improvements in sanitation, public health, and occupational safety implemented during the twentieth century have helped raise the age at which a person can expect to experience a life-threatening disease.
Older adults can and do experience acute, life-threatening medical conditions just as younger persons do, but acute episodes in older adults are more likely to be associated with chronic conditions. Either an acute condition is caused by a chronic problem, or a chronic problem persists after an acute episode. It is estimated that 80% of older adults live with chronic conditions such as arthritis, hypertension, diabetes, heart disease, and vision or hearing disorders. Most of those with a chronic illness are able to meet their own needs; only approximately 25% require any special type of care. Both acute health care and chronic health care are expensive.
Although older adults make up only approximately 12% of today’s population, they account for more than one-third of all health care expenditures. For the most part, today’s older adult population has benefited from improvements in medical care. Advances in surgery, technology, and pharmacology have enabled us to prolong life in situations that even a few years ago would have been impossible.
This level of care is not without substantial cost. Because a significant portion of older adults’ health care expenses is covered by Medicare and Medicaid, the burden on the younger members of society is becoming overwhelming. Despite steady increases in payroll taxes on the working population, Medicare has operated at a deficit since the start of the twenty-first century. Because there is a limit to how much taxpayer money is available, society must identify appropriate and acceptable ways to control health care costs.
One way of dealing with a steady increase in demand for health care services involves rationing the type and amount of care provided to older adults. This approach would prohibit or severely limit the type of care provided, particularly in cases in which the potential for significant improvement in health status is limited. For example, some of the more costly treatments and procedures (e.g., renal dialysis and bypass surgery) could be refused if the person were older than a predetermined age. This method has been adopted in some countries but is unpopular in the United States. To avoid rationing health care, we must find ways to maximize the effectiveness of our health care expenditures. In 2009 a health care reform legislation was passed, but it is very complex and the legality of some proposed changes is being challenged. Time will tell whether this is truly an effective reform or not.
Most studies reveal that it is more cost-effective to prevent problems than it is to attempt to cure or treat them. Therefore, more health care providers and the public (including older adults) are beginning to recognize the need to devote more attention to health promotion and health maintenance.
Health promotion is not a new concept. For decades, health care providers have stressed the importance of good nutrition, exercise, and regular medical care. Although most of this information was directed toward younger people, many older people who desired to live longer, healthier lives also paid attention. As the benefits of healthy lifestyle choices became obvious, television, radio, and other media joined health care providers in promoting health awareness. Awareness of the importance of good health-maintenance practices increased. Many individuals have modified their lifestyle and health care practices to improve their overall health and quality of life (Box 4-1). Those who are unaware or are unwilling to heed this advice persist in risky, health-threatening behavior. Nurses need to be aware of the health promotion and maintenance practices that will most benefit older adults. Nurses also need to understand why some older adults choose to adopt positive health behaviors, whereas others persist in seemingly self-destructive behavior.
Recommended health practices for older adults
Diet
Older adults should consume a well-balanced diet based on the food pyramid and recommended daily allowances of nutrients. Some changes in caloric intake and protein and vitamin needs appear to be desirable with aging (see Chapter 6).
When special diets are indicated, older adults need to learn how to read and interpret the information provided on packaging labels. This is particularly important with sodium-restricted diets because sodium is common in foods that do not necessarily taste salty. Because food labels are often printed in very small type, older adults should be sure to bring their eyeglasses or a magnifying glass when they shop. If someone else shops for them, that individual needs to know how to shop wisely.
Exercise
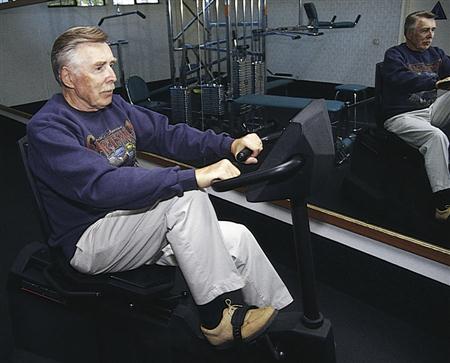
Regular exercise should be a part of any daily plan for older adults (Figure 4-1). Exercise can help keep the joints flexible, maintain muscle mass, control blood glucose levels and weight, and promote a sense of well-being. Exercise does not need to be aerobic to benefit older adults. Walking, swimming, golfing, housekeeping, and active lawn work or gardening are all considered exercise. To be of most benefit, exercise should consist of at least 30 minutes of continuous activity. The type, level, and amount of exercise that is most beneficial differ for each person and should be based on physician recommendations.
Tobacco and Alcohol
It is never too late to stop smoking. Even the body of an older person can repair damage once smoking is discontinued. Cessation may be difficult when smoking has been a long-standing habit, but various aids are now available to help smokers quit. Before using any of these aids, older adults should seek guidance from their physicians because they may need to follow some special precautions related to existing health problems.
Excessive consumption of alcoholic beverages is never recommended. Alcoholism is an all too common problem in the older adult population—both men and women—because alcohol may be used as a means of coping with depression, sleep disorders, or other problems. Occasional or moderate alcohol consumption by older adults usually is not prohibited or restricted unless some medical condition or medication precludes its use. Some physicians even recommend a glass of wine or beer as an appetite enhancer in certain situations.
Physical Examinations and Preventive Overall Care
Older adults should be examined at least once a year by their physicians—more often if known health problems exist. Some older adults resist this because of the cost or fear about what the physician may find. Cost is a real concern to many older adults, but inadequate health maintenance should be of more concern. A delay in the recognition of problems may make them more difficult and more costly to treat. Physical examinations provide an opportunity for the physician to detect problems before they become more serious, to monitor and treat chronic conditions, and to prevent some health problems.
Physical examinations in older adults should include evaluations of height and weight, blood pressure, and blood cholesterol levels if this has been a concern, as well as a rectal examination. In addition, women should have a pelvic examination, mammogram, and Papanicolaou (Pap) test to rule out cervical cancer. Older men need a prostate examination and blood tests to rule out prostate cancer. Persons with identified risk factors for colon cancer require occult blood screening and, possibly, a colonoscopy.
Evaluation of joints, feet, and gait should be part of the physical examination. Problems with the knees and shoulder joints can cause pain, limitation of activity, poor sleep, and decreased overall function. Some problems require surgical correction, whereas others can be treated more simply using analgesics, antiinflammatory medications, or physical therapy. Inspection of the feet often reveals problems. Many older adults have difficulty caring for their toenails because of poor vision, an inability to reach the feet, or hypertrophic nail changes. Bunions, calluses, and corns also cause problems for older adults. Neglecting the feet can lead to discomfort, restricted mobility, and a poorer quality of life. If the feet are not properly cared for, the risks for infection and even amputation increase, particularly in older individuals with compromised circulation. Older adults should be encouraged to wear properly fitted shoes that provide good support. Regular visits to a podiatrist can significantly reduce foot problems. Joint or foot problems, illness, pain, and other conditions commonly seen with aging can contribute to gait changes that are likely to result in imbalance or falls. When gait problems are identified, physical therapy for gait retraining and strengthening exercises, use of assistive devices, and environmental modification are appropriate (see Chapter 9).
Vision should be checked yearly to monitor for glaucoma or other eye problems. Refractive examinations can detect the need for a change in eyeglass prescription. Hearing examinations need not be done on a yearly basis unless a problem is suspected. When signs of diminished hearing are present, audiometric testing is appropriate.
Blood tests for hypothyroidism, diabetes, or cholesterol levels; electrocardiograms; and other diagnostic tests are not routinely part of the physical examination. Older adults should be aware of the need to communicate any symptoms they experience so that their physicians can determine the need for additional testing.
In addition to regular physical examinations, older adults should be sure to obtain immunization against diseases such as pneumonia and influenza that are more common in older adults than in younger adults. Because the immune system is less responsive than that of younger persons, it is important that they receive vaccinations in a timely manner.
The pneumonia vaccine is given starting at 65 or 70 years of age; repeating the vaccination every 10 years is recommended. The influenza vaccine must be obtained on a yearly basis, usually in the fall, because the strain of the virus changes frequently. Flu shots can be obtained from private physicians or from clinics that are available in most communities. Even with immunization a larger percentage of elderly contract influenza.
Although tetanus infection is rare in the United States, approximately half of the cases of tetanus affect the elderly. Persons who were never immunized against tetanus should receive a three-dose series of injections. Those who have been immunized at an earlier age should receive a tetanus booster every 10 years after age 65. Specific injuries may require a booster even if 10 years have not elapsed.
The risk of developing shingles, a herpes zoster infection that causes a classic rash and painful neuralgia, increases with age. The shingles vaccine has been available since 2006. This vaccination is recommended for people over age 60, provided they have a normal immune system. Benefits of this vaccine should be determined based on individual risks, preferences, and the physician’s recommendations. It is very expensive and is effective approximately 50% of the time.
The need for the hepatitis B immunization is based on individual risk factors and should be discussed with a physician.
Prophylactic use of medications such as aspirin (to prevent cardiovascular disease) and vitamin E (thought to decrease risk for stroke, heart attack, and Alzheimer’s disease) is gaining increased acceptance in the medical community. Older adults should be encouraged to discuss the possible benefits of this type of therapy with their physicians and then follow the recommendations.
Use of prescription and over-the-counter medications is common in the aging population. Older people with medical conditions must understand the reasons for and the importance of their treatment plans. They should keep a record card listing all of their medications and the names of the physicians who prescribed them. This card should be shown to all licensed professionals they see so that serious drug interactions are prevented. Older adults must know how and when to take prescribed medications, how to use over-the-counter medications safely, how to store their medications, and when to report side effects. Sharing prescription medications with friends or neighbors is dangerous and should be avoided. Medications can be confusing and even overwhelming to many people. Additional precautions regarding medications are discussed in Chapter 7.
To keep track of medical appointments, older adults should have a calendar or datebook where they can record all appointments or reminders for things such as immunizations. They also should be aware of signs and symptoms that indicate a need to seek medical attention that exceeds routine yearly examinations. Signs and symptoms indicating the need for prompt medical attention are listed in Box 4-2.
Older adults who have health problems or allergies, those taking medications such as heparin, and those with implanted medical devices such as pacemakers are advised to wear a Medic Alert bracelet or necklace. If they do not wish to wear such a warning device, these individuals should at least carry a card in their wallets or purses to provide the necessary health information.
Dental Examinations and Preventive Oral Care
Dental examinations should be obtained and an inspection of the oral cavity performed on a regular basis (at least once a year). Today’s older adults are keeping their natural teeth longer than previous generations were able to, probably because of better nutrition and improved prophylactic dental care. Gum disease and tooth decay are major causes of tooth loss. To prevent or slow the progress of these dental problems, older adults should brush their natural teeth at least daily using a fluoride toothpaste and should floss carefully between the teeth. Mouthwash may help refresh the breath, but it cannot replace regular brushing.
It is recommended that older adults use soft-bristle brushes to clean all tooth surfaces, particularly those individuals suffering from arthritis, because they may have difficulty holding and brushing with a standard toothbrush. Enlarging the brush handle using tape, wide rubber bands, sponges, or polystyrene or lengthening the brush by attaching a wood or plastic strip may make it easier to hold. Some older adults prefer an electric toothbrush that provides the proper movement.
Circular or short back-and-forth brushing works best to clean the teeth. Close attention should be paid to removing all plaque from along the gumline. Red, swollen, or bleeding gums indicate the need to see a dentist. People should have their teeth professionally cleaned at least once a year to remove stains and other debris missed by routine brushing.
Older adults who wear dentures still need regular oral examinations because people older than 65 years of age account for more than half of the new cases of oral cancer each year. Good oral hygiene is also necessary. Dentures must be brushed or cleaned at least once a day to remove food debris, bacteria, and stains and to prevent gum irritation or bad breath. Some denture wearers prefer to brush the dentures using a special dentifrice, whereas others prefer to use a soaking solution that works overnight. Either cleansing method is appropriate, but the chemicals should be rinsed thoroughly from the dentures before they are put back into the mouth.
An older person wearing dentures for the first time needs to become adept at inserting and removing them. Eating with dentures is often awkward, necessitating some relearning so that the wearer can chew effectively. Taking smaller pieces of soft, nonsticky foods and chewing more slowly are recommended. Because dentures make the mouth less sensitive to heat, cold, and foreign objects such as bone fragments, special care is required when eating.
Poor fit is a major reason that some older adults fail to wear their dentures regularly. This contributes to problems with nutrition and digestion. A few extra appointments with the dentist are often necessary to help fit the dentures properly. These adjustments are important because poorly fitting dentures can cause irritation to the gums or mucous membranes of the mouth. Additional adjustments may be needed if the denture wearer gains or loses weight.
Other changes in the oral cavity (e.g., dryness) are also common with aging. Although saliva production does not decrease in all older adults, a variety of medical conditions, medications, and treatments can cause or contribute to dry mouth. Dry mouth can best be relieved by drinking more water. Excessive use of hard candy, caffeine beverages, alcohol, or tobacco increases dryness of the mouth.
Maintaining Healthy Attitudes
Strong connections exist between the mind and body. Older adults who maintain a positive outlook on life tend to follow good health practices and remain healthier longer.
Regular interaction with other people of all age groups helps maintain a positive attitude toward life. It is recommended that older adults get out of the house as often as possible, even if only for shopping or dinner. Keeping in touch with family and friends is important. When spouses or friends are lost through death or relocation, older adults benefit from attempting to establish new relationships by joining church or community social groups. Volunteering in hospitals, schools, literacy centers, or other community agencies is a popular and desirable activity because it helps promote a sense of value and self-worth (Figure 4-2). As noted earlier in this text, many elderly continue to remain active in the workforce. This may be out of financial necessity or as a way to remain a productive, contributing member of society. A decrease in social interaction can contribute to the deterioration of cognitive and adaptive skills. Nurses cannot force an individual to participate beyond his or her wishes, but a little encouragement and information about options can help stimulate the older person’s interests.
Factors that affect health promotion and maintenance
The actions taken to promote, maintain, or improve health are based on that individual’s perception of his or her health. Health perceptions influence day-to-day choices regarding hygiene practices; nutrition; exercise; use of alcohol, drugs, and tobacco; accessing health care; and many other activities. Health-maintenance practices include safety precautions taken to prevent injury from automobile accidents, falls, poisoning, and other hazards. Health perceptions and health-maintenance practices in older adults are influenced by personal beliefs, religious and cultural beliefs, socioeconomic status, education, and life experiences.
As people mature, they establish a set of beliefs, perceptions, and values related to health. These perceptions include basic ideas regarding what health is and how to best maintain it. These beliefs form the foundation for each person’s health practices. Based on their unique beliefs, most people perform activities that they perceive to be helpful in maintaining their health and avoid activities they perceive as harmful. It is difficult to change a person’s lifetime health practices. Only those who are highly motivated to change are likely to be successful.
Religious Beliefs
Religious beliefs contribute to an individual’s perceptions. These beliefs can promote health maintenance or interfere with good health practices and result in increased health risks. For example, some religions teach that the body is a temple, stressing the importance of avoiding alcohol, tobacco, and other behaviors that are harmful to health. Individuals with these religious beliefs tend to live longer, healthier lives than do people who do not share these values. Other persons, whose religions teach that illness is a punishment for sins, may feel that they are not worthy of health and must endure illness as atonement for things they have done wrong in their lives.
Cultural Beliefs
Cultural beliefs and practices also play a significant role in health perception and health maintenance. For example, reliance on home health remedies is common in many cultures. Some home remedies are harmless, whereas others are quite dangerous. Problems can occur when home remedies are used in place of conventional medical care or when their use results in delayed care, which can be serious or even fatal if the illness is a serious one. Culture also plays a significant role in the selection of food and the methods used for food preparation. These preferences and practices play a significant role in health promotion and maintenance. Diets that consist mainly of fruit, vegetables, and grains are common in some cultures, whereas diets high in fat and sodium are prevalent in others. These variations can contribute to the good health of some ethnic populations or to the health problems seen in others.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree