Care of Aging Skin and Mucous Membranes
Objectives
1. Discuss changes related to aging that have an effect on skin and mucous membranes.
3. Describe interventions that assist older adults in maintaining intact skin and mucous membranes.
Key Terms
alopecia (ăl-ō-PĒ-shē-ă) (p. 271)
aseptic (ā-SĔP-tĭk) (p. 277)
caries (KĂR-ēz) (p. 279))
exudate (ĔKS-ū-dāt) (p. 274)
gingivitis (j n-j
n-j –
– I-tĭs) (p. 279)
I-tĭs) (p. 279)
halitosis (hăl- -TŌ-sĭs) (p. 279)
-TŌ-sĭs) (p. 279)
hyperkeratosis ( l-pĕr-kĕr-ă-TŌ-sĭs) (p. 273)
l-pĕr-kĕr-ă-TŌ-sĭs) (p. 273)
leukoplakia (lū-kō-PLĀ-kē-ă) (p. 280)
pigmentation (p g-mĕn-TĀ-shŭn) (p. 268)
g-mĕn-TĀ-shŭn) (p. 268)
pressure ulcers (p. 266)
pruritus (prū- I-tŭs) (p. 266)
I-tŭs) (p. 266)
scabies (SKĀ-bēz) (p. 268)
xerostomia (zēr-ō-STŌ-mē-ă) (p. 280)
 http://evolve.elsevier.com/Wold/geriatric
http://evolve.elsevier.com/Wold/geriatric
The skin undergoes several changes with aging that make it more susceptible to damage. Over time, the epidermal layer becomes thinner and subcutaneous padding diminishes, increasing the risk for traumatic injuries such as skin tears or pressure ulcers. Bruises are more common because capillary walls are more fragile. Medications used to treat various health problems can cause problems. Corticosteroids make the skin more fragile, and anticoagulants increase the risk for bleeding with even minor trauma. Decreased sebaceous secretions and circulatory changes contribute to the dry skin and scaliness of the lower extremities common with aging. Aging skin is more susceptible to inflammation, infection, and rashes. Pruritus, which is a common complaint in older adults, may be caused by dryness, irritation, or infection but can be related to diseases such as diabetes mellitus, kidney disease, malignancy, or anemia. Changes in the function of dermal receptor cells result in a decrease in the ability of the older person to perceive sensations such as touch and pressure, increasing the risk for pressure-related disorders. Although skin problems usually are not life threatening, they are significant because they can distress the older person and lead to decreased quality of life. Skin problems should be prevented whenever possible; in situations in which the problems are not preventable, they should be recognized, treated, and resolved in a timely manner.
Age-Related Changes in Skin, Hair, and Nails
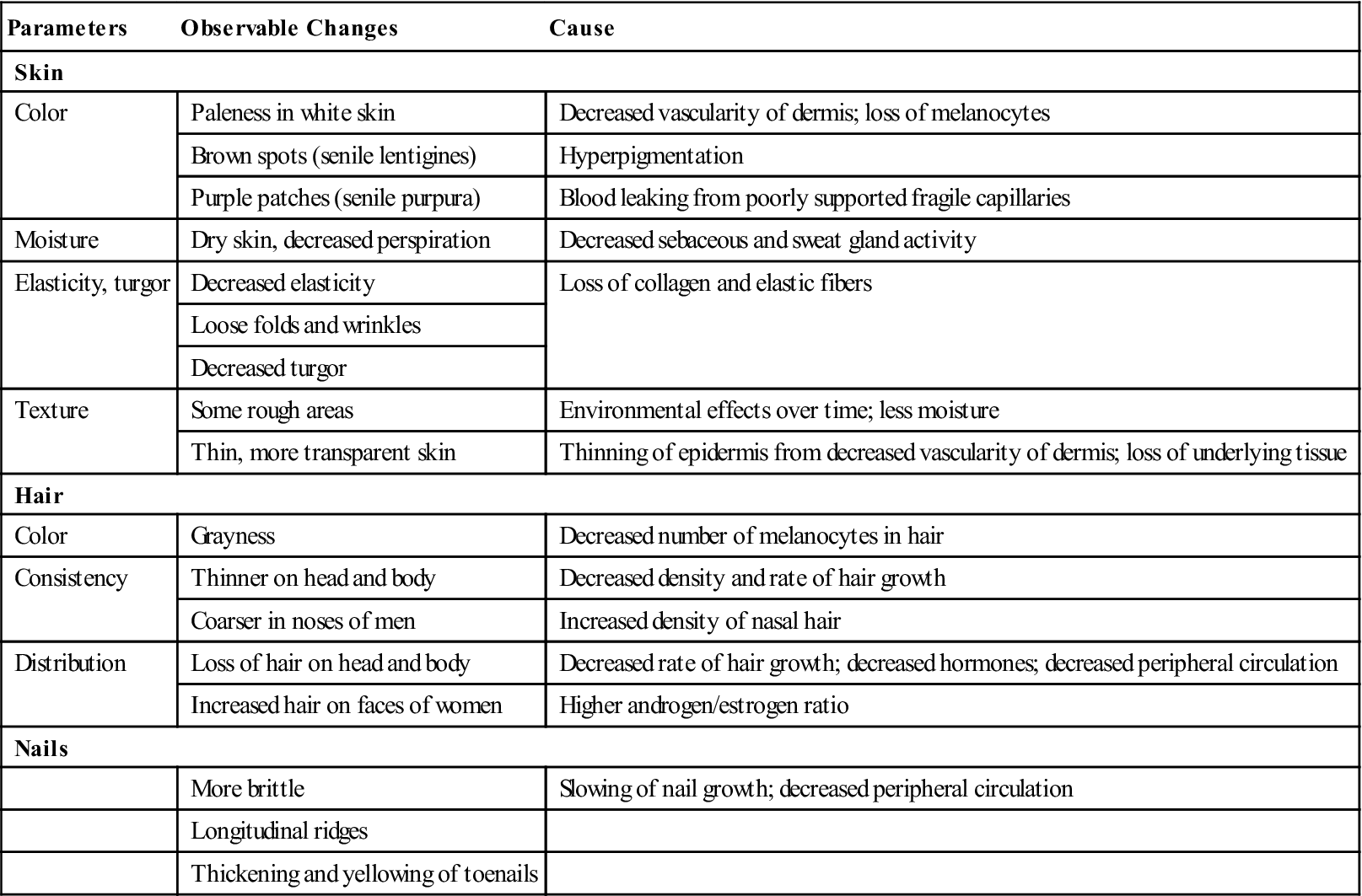
Changes in the skin, hair, and nails may indicate a variety of problems related to nutritional and circulatory adequacy. Because these structures are the ones most easily observed, they can provide a great deal of information about the metabolic health of the entire body (Table 17-1).
Table 17-1
Age-Related Changes in Skin, Hair, and Nails
| Parameters | Observable Changes | Cause |
| Skin | ||
| Color | Paleness in white skin | Decreased vascularity of dermis; loss of melanocytes |
| Brown spots (senile lentigines) | Hyperpigmentation | |
| Purple patches (senile purpura) | Blood leaking from poorly supported fragile capillaries | |
| Moisture | Dry skin, decreased perspiration | Decreased sebaceous and sweat gland activity |
| Elasticity, turgor | Decreased elasticity | Loss of collagen and elastic fibers |
| Loose folds and wrinkles | ||
| Decreased turgor | ||
| Texture | Some rough areas | Environmental effects over time; less moisture |
| Thin, more transparent skin | Thinning of epidermis from decreased vascularity of dermis; loss of underlying tissue | |
| Hair | ||
| Color | Grayness | Decreased number of melanocytes in hair |
| Consistency | Thinner on head and body | Decreased density and rate of hair growth |
| Coarser in noses of men | Increased density of nasal hair | |
| Distribution | Loss of hair on head and body | Decreased rate of hair growth; decreased hormones; decreased peripheral circulation |
| Increased hair on faces of women | Higher androgen/estrogen ratio | |
| Nails | ||
| More brittle | Slowing of nail growth; decreased peripheral circulation | |
| Longitudinal ridges | ||
| Thickening and yellowing of toenails | ||
From Phipps WJ, et al: Medical-surgical nursing: concepts and clinical practice, ed 4, St Louis, 1991, Mosby.
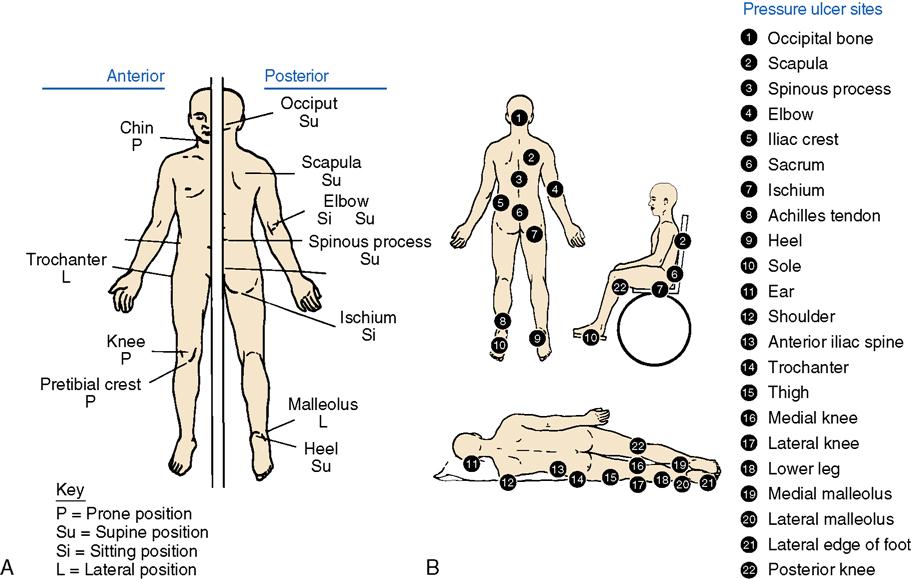
Complete assessment of skin, hair, and nails is best done when the person is undressed so that all skin surfaces can be inspected. Skin assessment can be performed during a bath, during daily personal hygiene, at bedtime, or at any other convenient time for the older person. Independent older persons should be aware of what is normal for themselves, and they should bring any changes to the attention of the physician. In a hospital or extended-care setting, privacy must be maintained and modesty protected during the skin inspection. Assessment of the skin and ancillary structures is an important responsibility of nurses. Nursing assistants and attendant health care workers who assist with bathing or other care should be instructed to report any unusual or questionable observations promptly to a nurse for further investigation. Inspection should follow a logical order so that no pertinent observations are missed. Most nurses find that a head-to-toe progression is the most helpful, as is a body diagram on which observations are indicated (Figure 17-1).
Skin Color
Skin color changes can indicate a variety of disorders. When assessing skin for color, it is important to be aware of the differences in skin pigments among ethnic groups. Examination of the skin should take place in good, preferably natural, light; one side of the body should be compared with the other; and touch should be used to determine skin temperature or the presence of rashes or irritation. Stretching the skin slightly may also help in determining the underlying tones. Color changes, including pallor, cyanosis, jaundice, or erythema, can indicate a variety of problems. The extent and location of any color changes should be recorded and reported promptly.
Dry Skin
Dry skin is one of the most common problems of aging. Various studies have shown that 75% to 85% of people older than 65 years of age experience some degree of problem with dry skin. Physiologic changes, excessive bathing, the use of harsh soaps, and a dry environment all contribute to problems with dry skin.
Dry skin can result in itching (pruritus), burning, and cracking of the skin (Figure 17-2). Many older people develop a habit of scratching or picking at dry or cracked skin, increasing their risk for further tissue damage and infection. Skin irritation can be severe and can cause intense discomfort to older adults. In fact, it may be so distracting that affected individuals cease to participate in social activities.

Rashes and Irritation
Rashes and skin irritation can be caused by factors other than dryness. Medications, communicable diseases, and contact with chemical substances are common causes of skin rashes and pruritus (Figure 17-3).
Allergic response to medications can manifest as diffuse rashes over the body. Whenever a rash develops soon after administration of new medication, an allergy should be suspected. It is appropriate to withhold that particular medication and contact the physician to report the symptom.
One communicable source of skin irritation and severe pruritus is scabies. Scabies is a superficial infection caused by a parasitic mite (Sarcoptes scabiei var. hominis) that burrows under the skin (Figure 17-4). Older adults, especially individuals who suffer from chronic illness, dementia, or a depressed immune system, are particularly vulnerable to scabies infections. Signs of scabies include intense itching and fine, dark, wavy lines at the flexor surface of the wrist or elbow, the webbed area of the fingers, the axilla, and the genitals. Recognition of scabies may be difficult in older adults because it has an asymptomatic incubation period of 4 to 6 weeks and because atypical presentations are common. When infestation is suspected, skin scrapings should be examined to determine the presence of ova or mites.
Scabies is spread from person to person by direct contact. Because recognition is difficult, treatment may be delayed, allowing the parasite to infect other people. To reduce outbreaks of scabies infection within an institution, all new residents in extended-care settings should be assessed carefully on admission. All cases must be identified and treated promptly to prevent spread or reinfestation with the parasite.
Pigmentation
Changes in skin pigmentation are common with aging. These changes are discussed in Chapter 3. Many of the changes are cosmetic and do not cause problems unless they are located on the face or arms, where they may be distressing to the affected person. Common conditions such as acne rosacea can be treated with topical medications, which help heal the skin and reduce redness, whereas others can be concealed by appropriate use of cosmetics. Changes in the size or pigmentation of moles are of greater significance because these changes may indicate the presence of a precancerous or cancerous condition that needs immediate medical attention.
Tissue Integrity
Breaks in tissue integrity increase the older person’s risk for infection and often result in the need for costly, time-consuming treatments. These breaks can cause disfigurement and are frightening to older adults. Skin tears, abrasions, lacerations, and ulcers most often result from friction, shearing force, moisture, and pressure. Even simple incidents such as contact with furniture, sliding across bed linens, a grip during a transfer, or the removal of tape may result in significant skin trauma to the older person.
Pressure Ulcers
Pressure ulcers are a particular risk to older adults who suffer from compromised circulation, restricted mobility, altered level of consciousness, fecal or urinary incontinence, or nutritional problems (Table 17-2). Studies estimating the occurrence of pressure ulcers vary widely, but one consistent point is that they occur in all settings. Although most studies show that the incidence of pressure ulcers has declined, there is still much work to be done. Pressure ulcers have negative effects on the overall health of an elderly person. They can lead to infection, pain, loss of function, and even death. Furthermore, incidence of pressure ulcers can leave care facilities and nurses vulnerable to lawsuits for negligence. They strain the health care system with treatment costs estimated at $11 billion per year. New Medicare rules specify that a hospital will not be reimbursed for the care of a patient who develops a pressure ulcer after being admitted to a hospital. This should be a great motivator for hospitals to institute pressure ulcer prevention programs.
Table 17-2
Quick Guide to Prevention of Pressure Ulcers
| Risk Factor | Nursing Interventions |
| Immobility | Establish individualized turning schedule; reduce shear and friction by using trapeze and/or turning sheet; elevate HOB <30 degrees; provide pressure-relief surface |
| Inactivity | Provide assistive devices to increase activity |
| Incontinence | Assess the need for incontinence management; clean and dry skin after soiling |
| Malnutrition | Provide adequate nutritional and fluid intake; assist with snacks and meals, monitor intake and output (I & O); consult the dietitian for nutritional evaluation |
| Diminished sensation, decreased mental status | Assess the patient’s and family’s ability to provide care; educate caregivers regarding pressure ulcer prevention |
| Impaired skin integrity | Avoid pressure; do not use donut-shaped cushions or sheepskin; lubricate skin; apply barrier ointments to protect skin from moisture; do not massage red areas; Do not use heat lamps, heating pads, or hot water. |
Modified from Catania K, et al; PUPPI—The pressure ulcer prevention protocol interventions, Am J Nurs, 107(4): 44–52, 2007.
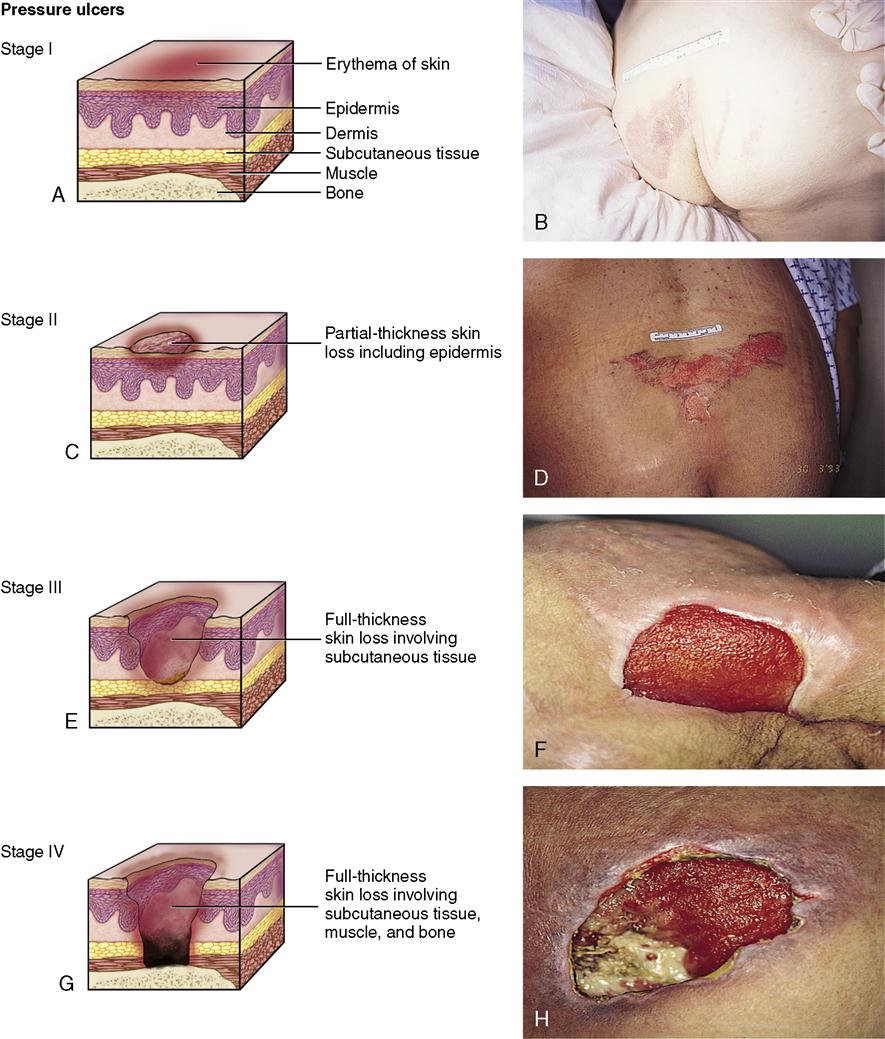
Excessive pressure on tissues, particularly over bony prominences, can quickly lead to skin breakdown (Figure 17-5). Ulcer development depends on the amount of pressure, the length of time pressure is exerted, and the underlying status of the tissues involved. Tissue that is subjected to excessive pressure does not receive adequate oxygen or nutrients. This can result in ischemia and increased susceptibility to breakdown. When tissue is deprived of necessary nutrients for a longer period, necrosis and tissue destruction result. Tissue that is fragile because of poor nutrition or circulation is most susceptible to breakdown. Early danger signs indicating a risk for breakdown include pale or reddened tissue. Pressure ulcers are categorized or staged based on their appearance and the depth of tissue penetration (Figure 17-6).
Individuals who have had one pressure ulcer are at greater risk for future development of additional ulcers. Additional factors that contribute to development of pressure ulcers include the following:
• Multiple coexisting diseases
• History of alcohol and tobacco use
• Bladder and/or bowel incontinence
Rather than wait for skin breakdown to occur, most health care agencies perform a formal risk assessment at the time of admission and then at regular intervals. The most common tools used for this assessment are the Braden and Norton Scales (see Tables 17-3 and 17-4). Nurses use the information from this assessment to develop a plan of care that minimizes risk factors and promotes skin integrity.
Table 17-3
Braden Scale for Predicting Pressure Sore Risk
| Assessment Tool | 1 Point | 2 Points | 3 Points | 4 Points |
| Sensory Perception | ||||
| Ability to respond meaningfully to pressure-related discomfort | Completely limited: Unresponsive (does not moan, flinch, or grasp) to painful stimuli because of diminished level of consciousness or sedation or Limited ability to feel pain over most of body surface or discomfort over half of body | Very limited: Responds only to painful stimuli; cannot communicate discomfort except by moaning or restlessness or Has a sensory impairment that limits the ability to feel pain on one or two extremities | Slightly limited: Responds to verbal commands but cannot always communicate discomfort or the need to be turned or Has some sensory impairment, which limits ability to feel pain or discomfort | No impairment: Responds to verbal commands; has no sensory deficit that could limit ability to feel or voice pain or discomfort |
| Moisture | ||||
| Degree to which skin is exposed to moisture | Constantly moist: skin is kept moist almost constantly by perspiration, urine, and the like; dampness is detected every time patient is moved or turned | Very moist: Skin is often, but not always, moist; linens must be changed at least once a shift | Occasionally moist: skin is occasionally moist, requiring an extra linen change approximately once a day | Rarely moist: Skin is usually dry; linen requires changing only at routine intervals |
| Activity | ||||
| Degree of physical activity | Bedridden: Confined to bed | Chairfast: Ability to walk severely limited or nonexistent; cannot bear own weight and/or must be assisted into chair or wheelchair | Walks occasionally: walks occasionally during day, but for very short distances, with or without assistance; spends majority of each shift on bed or chair | Walks frequently: walks outside room at least twice a day and inside room at least once every 2 hours during waking hours |
| Mobility | ||||
| Ability to change and control body position | Completely immobile: does not make even slight light changes in body or extremity position without assistance | Very limited: Makes occasional slight changes in body or extremity position but is unable to make frequent or significant changes independently | Slightly limited: makes frequent although slight changes in body or extremity position independently | No limitations: makes major and frequent body position changes without assistance |
| Nutrition | ||||
| Usual food intake pattern | Very poor: Never eats complete meal; rarely eats more than one third of any food offered; eats two servings or less of protein (meat or dairy products) per day; takes fluids poorly; does not take a liquid dietary supplement or receives nothing by mouth and/or is maintained on clear liquids or intravenous | Probably inadequate: rarely eats a complete meal; generally eats only approximately half of any food offered; protein intake includes only three servings of meat or dairy products per day; occasionally takes a dietary supplement or receives less than optimal amount of liquid diet or tube feeding solutions for more than 5 days | Adequate: Eats more than half of most meals; eats a total of four servings of protein (meat or dairy products) each day; occasionally refuses a meal, but usually takes a supplement if offered or is on a tube feeding or total parenteral nutrition regimen that probably meets most of nutritional needs | Excellent: Eats most of every meal; never refuses meal; usually eats total of four or more servings of meat and dairy products per day; occasionally eats between meals, does not require supplements |
| Friction and shear | ||||
| Problem: Requires moderate to maximal assistance in moving; complete lifting without sliding against sheets is impossible; frequently slides down in bed or chair, requiring frequent repositioning with maximal assistance; spasticity, contractions, or agitation leads to almost constant friction | Potential problem: moves feebly or requires minimal assistance; during a move, skin probably slides to some extent against sheets, chair, restraints, or other devices; maintains relatively good position in chair or bed most of the time but occasionally slides down | No apparent problem: moves in bed and in chair independently and has sufficient muscle strength to sit up completely during move; maintains good position in bed or chair at all times | ||
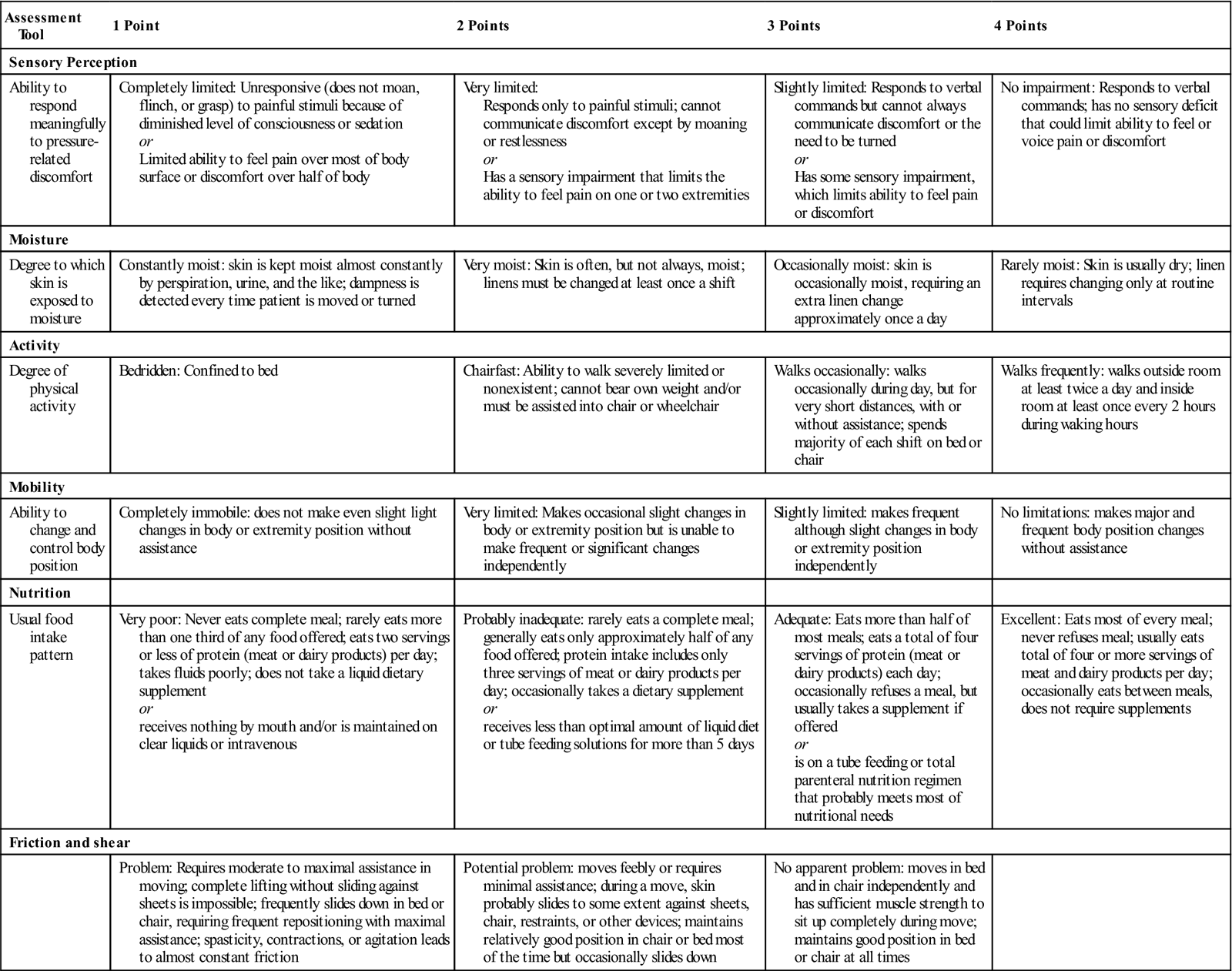
From Bergstrom N, et al: The Braden scale for predicting pressure sore risk, Nurs Res 36(4): 205–210, 1987. Instructions: Score patient in each of the six subscales. The maximum score of 23 has the best prognosis, and the minimum score of 6 has the worst prognosis. A patient is at risk for pressure ulcer if the score is ≤16.
Table 17-4
| Physical Condition | Mental Condition | Activity | Mobility | Incontinent | Total Score | ||||
| Good | 4 | Alert | 4 | Ambulant | 4 | Full | 4 | Not | 4 |
| Fair | 3 | Apathetic | 3 | Walk/help | 3 | Slightly limited | 3 | Occasional | 3 |
| Poor | 2 | Confused | 2 | Chairbound | 2 | Very limited | 2 | Usually/Urine | 2 |
| Very bad | 1 | Stupor | 1 | Bed | 1 | Immobile | 1 | Doubly | 1 |
| Name | |||||||||
| Date |
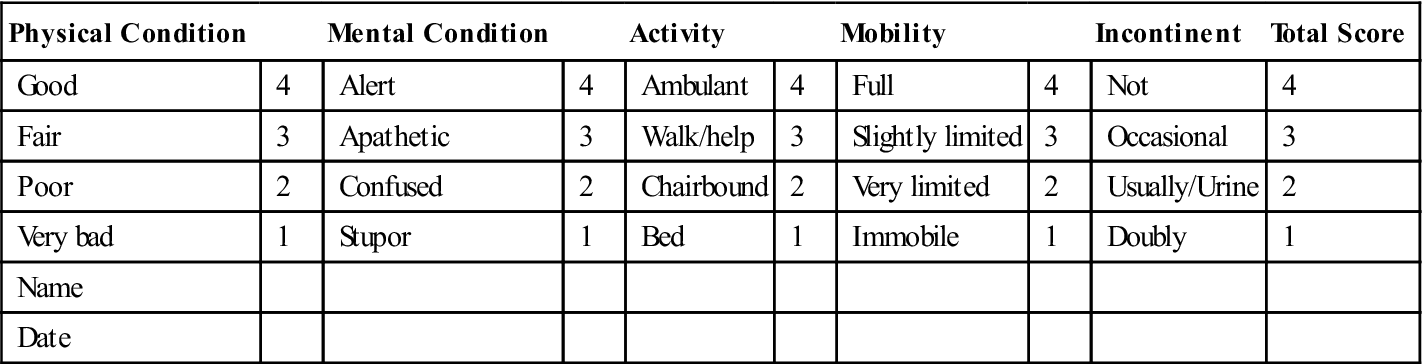
From the Centre for Policy on Ageing, London, England, 1962.
Amount, Distribution, Appearance, and Consistency of Hair
The amount, distribution, appearance, and consistency of the hair change with aging. The hair of both men and women typically becomes thinner and has a finer consistency with advanced age. Heredity and gender play a role in hair loss patterns. Men tend to lose more hair than do women, although some men retain a full head of hair throughout life. Male pattern baldness typically results in progressive loss of hair at the temples and back of the head. Sudden and excessive hair loss (alopecia) or breakage is likely to indicate a systemic problem. Abnormal hair loss can be related to high fevers, medications, nutrition problems, fungal or bacterial infections, endocrine disorders, or stress. Sudden or unusual hair loss should be reported so that the physician can determine the cause.
The amount and distribution of body hair also change with aging. Diminished or absent hair on the lower legs or feet—particularly when combined with excessively dry, scaly, or flaky skin and weak or absent pedal pulses—indicates decreased blood supply to the lower extremities.
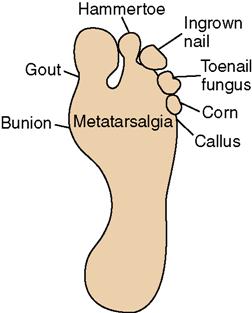
Tissue of the Feet
Inspection of the tissue on the feet warrants special attention in older adults. Because many aging individuals are unable to bend adequately to view the feet, a family member or friend can perform this inspection for independent older adults (Figure 17-7). In an institutional setting, foot inspection should be performed by the nursing staff. Many older adults neglect their feet simply because they cannot see or reach them. Unless foot inspection is done on a regular schedule, severe problems can occur before anyone is aware of them.
Nails
Aging results in hyperkeratosis of the nails, particularly the toenails. Thick, hard nails are difficult to cut using normal foot care equipment. The strength and effort required to cut these nails may exceed the older person’s abilities, resulting in overgrowth. Soaking the feet in warm water before attempting to cut them may help soften the nails and make them easier to cut. Assistance from a family member or health care provider is appropriate when there is no history of circulatory problems or diabetes. When diabetes or circulatory problems are present, care should be provided by a foot care specialist. Special heavy-duty equipment may be needed to accomplish proper nail care. Use of safety glasses is recommended during nail care to prevent eye injuries from flying nail particles.
If proper care is neglected, uncut nails confined in shoes often begin to curl under the toes, resulting in a condition called ram’s horn nails. In this condition, the nail curls over the top of the toe and grows into the flesh on the bottom, causing pain. When the discomfort becomes severe, the older person may stop wearing shoes and decrease ambulation in an attempt to reduce the discomfort. In such severe cases, care from a podiatrist is advisable. Nail fungus is increasingly common with aging. Fungi cause the nails to become thick, brittle, misshapen and discolored. Fungal infections are more likely to affect the feet because the environment in shoes (dark, moist, and warm) supports growth of these microorganisms. Fungal infections are more common in elderly persons with diabetes or other conditions of diminished peripheral circulation. These infections need to be recognized and treated so that they do not cause more widespread problems.
Other Common Foot Problems
Other common foot problems include corns, calluses, blisters, and bunions, which usually result from years of wearing poorly fitted footwear. These conditions often cause discomfort for older adults and lead to some degree of activity restriction. Many independent older adults use commercially available foot remedies or attempt to remove corns or calluses with a knife or scissors. This practice is dangerous and significantly increases the risk for serious foot infections, which may necessitate amputation of a toe, toes, or the entire foot. Older persons with diabetes or impaired peripheral circulation are particularly prone to develop foot ulcers or infections and are at greatest risk for amputation.
Nursing Process for Impaired Skin Integrity
Assessment/Data Collection
• What is the general appearance of the person’s skin?
• Are any sores evident on the scalp?
• Are there any areas of dry skin? If so, where?
• Does the person complain of itching?
• Is there any evidence of scratching?
• Is there any sign of pallor or erythema over bony prominences?
• Are there any breaks in the skin integrity? If so, where? What do they look like?
• Are any abrasions (friction burns) or skin tears evident?
• Is there any change in the amount, distribution, or appearance of the hair?
• What is the appearance of the toenails? Are they thickened? Difficult to cut? Discolored?
• Are any sores or lesions evident on the feet or ankles?
• What is the person’s nutritional status? Is the person overweight or underweight?
• Is the person alert and able to move freely? If not, what is the level of immobility?
• Is the person incontinent of bladder or bowel?
• Are there pedal pulses? Are these pulses easy or difficult to detect?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree