Nadinia Davis By the end of this chapter, the student should be able to: 1. Identify and describe the major medical specialties. 2. Distinguish among nursing occupations. 3. Identify and describe the major allied health professions and their principal occupational settings. 4. Distinguish between inpatients and outpatients. 5. Describe the differences among health care facilities. 6. Describe government involvement in health care. 9. List four major accrediting organizations and the facilities they accredit. accreditation activities of daily living (ADL) acute care facility admission allied health professionals ambulatory care facility American Health Information Management Association (AHIMA) assisted living bed count behavioral health facility Centers for Medicare and Medicaid Services children’s hospital Commission on Accreditation for Health Informatics and Information Management (CAHIIM) Conditions of Participation (COP) consultation continuity of care continuum of care credentials deemed status Department of Health and Human Services (DHHS) diagnosis discharge dual governance ethics health information management (HIM) health information technology (HIT) home health care hospice hospital hospitalist inpatients integrated delivery systems (IDS) licensed beds licensure long-term care (LTC) facility Medicaid medical specialty Medicare medication mental health facility National Integrated Accreditation for Healthcare Organizations (NIAHO) nurse occupancy outpatient palliative care patient care plan physician physician’s orders primary care physician (PCP) procedure psychiatrist referral rehabilitation facility resident The Joint Commission (TJC) The purpose of this chapter is to help you understand the basic structure and terminology of the health care industry. Most people have experienced the need for health care at one time, either at birth or for treatment of a particular illness or injury. In fact, some people know a lot about certain types of health care because of their own illness or the illness of a family member or friend. While reading this chapter, you may find it helpful to try to recall such personal experiences, to link what is presented here to your previous experiences and understanding of the health care industry. The health care industry includes professionals in many disciplines. These professionals vary from physicians and nurses to therapists and technicians to administrative and financial personnel. Each of these professionals plays a vital role in the delivery of health care. Physicians generally direct the delivery of care. They make decisions about the patient’s condition and advise treatment. Physicians are vital to the health care team, because typically they are the individuals who direct the treatment plan, through physician orders. Nurses and therapists often work on teams with physicians, helping to make those decisions and carrying out the recommended treatments. Technical and administrative personnel support the teams by administering and evaluating tests, organizing data, and evaluating processes and procedures. A physician is a person who is licensed to practice medicine. The practice of medicine is regulated by the individual state, which issues the license. To become licensed, a physician attends college and medical school and then serves a residency in his or her specialty. A physician earns a degree as a Doctor of Medicine (MD) or a Doctor of Osteopathy (DO). The schools that train MDs and DOs focus on different philosophies of medical treatment and diagnosis. A resident performs professional duties under the supervision of a fully qualified physician. Residency can last from 4 to 8 years, depending on the specialty. The medical licensing examination can be taken after the first year of residency. MDs take the United States Medical Licensing Examination (USMLE), which is developed and administered by the Federation of State Medical Boards (FSMB) in collaboration with the National Board of Medical Examiners (NBME). The USMLE is a three-step examination process that tests both the knowledge of the candidate and the ability of the candidate to apply that knowledge in the clinical setting. Examination results are provided to the individual state medical boards for licensing purposes (United States Medical Licensing Examination, 2012). Historically, DOs relied on physical manipulation of the patient, particularly the spine, to alleviate symptoms of disease. MDs, on the other hand, used drugs and surgery, also called conventional medicine, to treat patients. The term allopathic is sometimes used in reference to the conventional approach. In the United States, DOs take a whole-body approach and are likely to use both manipulation (osteopathic manipulative treatment) and conventional methods. However, in other countries, the historical differences remain. All states in the United States license both MDs and DOs (American Osteopathic Association, 2012). Physicians are generally categorized by medical specialty. They can treat patients according to the area of the body, according to specific diseases, or by assisting with diagnosis. For example, an oncologist is a physician who diagnoses and treats cancers. A gastroenterologist specializes in diseases of the digestive system. Treatments range from diet and exercise, to oral medications, to procedures, such as surgical removal of diseased tissue. Some specialties may focus more narrowly on the patient’s age group; a pediatric oncologist deals with children’s cancers. Table 1-1 lists some common medical specialties. TABLE 1-1 Several of the tasks that physicians perform are considered specialties, even though many physicians may perform those tasks to a certain extent. For instance, a radiologist is a specialist who interprets radiographs and images from other types of examinations of internal organs. A gastroenterologist knows how to read a radiograph, but it is not his or her specialty. A growing practice is physicians who specialize in treating hospitalized patients. So, although many physicians admit patients into hospitals and care for them there, hospitalists care only for patients in that environment. Medicine typically requires a minimum 10 years of study after high school. A physician who intends to specialize in family practice attends college for 4 years and medical school for another 3 years. He or she then applies for a residency of 3 years in family practice, studying internal medicine, pediatrics, obstetrics and gynecology, psychiatry, and geriatrics. An additional year of residency is required if the physician wants to further specialize in geriatrics, adolescent, or sports medicine (American Association of Medical Colleges, 2011). Beyond licensing and completing the residency, physicians pursue additional training and take an examination to become board certified. Board certification is developed and administered by the specialty board that sets standards of education for the physician’s specialty. The American Board of Medical Specialties is an umbrella group representing the 24 medical specialty boards (American Board of Medical Specialties, 2011). Among the 24 medical specialties, there are additional subspecialties. As noted previously, geriatrics is a subspecialty of family medicine. A board-certified family practitioner is referred to as a Diplomate of the American Board of Family Medicine. See Box 1-1 for a list of medical specialty boards. Most individuals have a relationship with a family practitioner. This physician is trained to identify and treat a wide variety of conditions. However, the family practitioner also seeks guidance from other specialists as needed. For example, the family practitioner may identify a suspicious skin problem and send the patient to a dermatologist for evaluation. The process of sending a patient to another physician in this manner is called a referral. Alternatively, the family practitioner may ask the dermatologist to evaluate the patient’s condition and confirm the family practitioner’s ideas or give recommendations for treating the patient. The latter process is further called a consultation. A physician who coordinates the care of a patient, through referrals and consultations, is called a primary care physician (PCP). A family practitioner is most often the PCP for his or her patients. However, not all PCPs are family practitioners. For example, some women choose to use their gynecologists as their PCPs. A pediatrician is frequently the PCP for a child. A nurse is a clinical professional who has received post-secondary school training in caring for patients in a variety of health care settings. There are several levels of nursing education, each qualifying the nurse for different positions. Historically, most nurses graduated from a hospital-based certificate program. Another large percentage received their training through associate degree programs. A growing number of nurses have a bachelor’s or master’s of science degree in nursing, and today, almost all nurses are college educated at some level. Nurses, like doctors, take licensing examinations. Table 1-2 lists the various levels of nursing and their educational requirements. TABLE 1-2 From American Nurses Association: http://www.nursecredentialing.org/Certification.aspx; All Nursing Schools: http://www.allnursingschools.com/faqs/lpn.php. Published 2012. Accessed July 10, 2012. A licensed practical nurse (LPN), sometimes referred to as a vocational nurse, receives training at a hospital-based, technical, or vocational school. The training consists of learning to care for patients’ personal needs and other types of routine care. LPNs work under the direction of physicians or registered nurses, or both. The extent of their practice depends on the rules of the state in which they are licensed. It may include providing treatments and administering medications. In addition to caring for patients’ personal needs, a registered nurse (RN) administers medication and renders other care at the order of a physician. RNs particularly focus on assessing and meeting the patients’ need for education regarding their illness. RNs may specialize in caring for different types of patients. For example, a nurse may assist in the operating room or care for children or and older adult, each of which requires special skills and training. RNs who want to move into management-level or teaching positions generally pursue a master’s degree, a doctoral degree, a specialty certification, or some combination of these qualifications. In response to physician shortages and nurses’ desire for greater independence, several advanced specialties in nursing practice have developed under the general title advanced practice registered nurse (APRN). Examples of these specialties are nurse midwives and nurse anesthetists. A nurse midwife focuses on the care of women during the period surrounding childbirth: pregnancy, labor, delivery, and after delivery. A nurse anesthetist is trained to administer anesthesia and to care for patients during the delivery of anesthesia and recovery from the process. APRNs have a minimum of a master’s degree and additional training and certification beyond the RN certification. The American Nurses Credentialing Center, a subsidiary of the American Nursing Association, offers a variety of advanced practice certifications in subspecialties such as diabetes management and pediatrics (American Nurses Credentialing Center, 2006). Allied health (or health-related) professionals can include both clinical and nonclinical professionals who provide a variety of services to patients. A clinical professional is one who provides health care services to a patient, generally pursuant to orders from a physician or APRN. Clinical professionals include radiology technicians and a variety of therapists. Nonclinical professionals support the clinical staff and provide other types of services to a patient. Nonclinical allied health staff includes health information management professionals. Table 1-3 provides examples of clinical allied health professions, their principal work environments, and their basic educational requirements. TABLE 1-3 EXAMPLES OF CLINICAL HEALTH-RELATED PROFESSIONS Increasing demand for health care workers and the special emphasis on particular groups of patients has led to a proliferation of professional associations and credentials. One of the primary roles of a professional association is to improve the practice of the profession. Therefore professional associations play a critical role in the development of professional standards and improvement in health care delivery. One of the standards of professional practice that can improve health care is mandatory education, both formal education and continuing education. Formal education in the discipline supports consistency of education, research, and growth of the knowledge base of the profession. The outcome of this formal education process is often the qualification to sit for an examination. That examination is designed to measure the competence of the individual. The specific level of competence varies from entry-level (basic) competence to advanced or specialty practice. Satisfaction of the profession’s requirements for competence entitles the individual to certain credentials. Maintenance of a professional credential generally requires continuing education (CE). Continuing professional education supports the currency of professional knowledge among practitioners. The credentialing requirements of professions vary widely. In some cases, no formal education is required. In other cases, no actual professional experience is required. In general, the professional associations themselves, or their credentialing affiliates, dictate the levels of expertise and evidence of competence required for the granting of credentials. For some professionals, such as nurses and physicians, licensure granted by the state or professional association is required in addition to competency examinations. Health information management (HIM) is an example of a category of professionals with multiple professional associations and a variety of credentials. The American Health Information Management Association (AHIMA) supports the health care industry by promoting high-quality information standards through a variety of activities, including but not limited to accreditation of schools, continuing education, professional development and educational publications, and legislative and regulatory advocacy. The American Academy of Professional Coders (AAPC) promotes the accuracy of coding and billing in all health care settings, but particularly outpatient. AAPC offers multiple credentials in coding as well as auditing and training. Coding is discussed in Chapters 5 through 7 as it is an important HIM function. Health information management (HIM) encompasses all the tasks, jobs, titles, and organizations involved in the administration of health information, including collection, storage, retrieval, and reporting of that information. HIM professionals perform or oversee the functions that support these activities and frequently expand their practice to related activities, encompassing the financial and technical operations of a health care practitioner or organization. For example, HIM professionals may assist in the development and implementation of electronic health records (EHRs), oversee the maintenance of those databases, provide support services such as patient registration, retrieve data for reporting and continuing patient care, and participate in the billing process. Literally hundreds of different jobs with many different titles are performed by HIM professionals throughout the world. This text presents specific job descriptions and job titles that can assist in planning a career in HIM. (See Table 1-4.) TABLE 1-4 EXAMPLES OF HEALTH INFORMATION MANAGEMENT PROFESSIONALS HIM professionals work in virtually every area of the health care delivery system, from physician offices and hospitals to insurance companies and government agencies. They are also employed by suppliers, such as computer software vendors, and educational institutions as well as consulting firms. Throughout this text are discussions of historical roles, emerging roles, and the future of the HIM profession. As you review the many opportunities available to HIM professionals, it would be useful to check industry publications and Web sites for information about those specific jobs in your geographical area and around the world. The American Health Information Management Association (AHIMA) offers certification at progressively higher levels of education and experience. According to the AHIMA Web site, the organization offers the following (AHIMA, 2012): Coding credentials (see Chapter 6 for a detailed discussion of coding issues): General HIM credentials include the following: Advanced and specialty practice credentials include the following. Eligibility criteria and testing requirements are posted on the AHIMA Web site (AHIMA, 2012). The examinations for all of the previously mentioned credentials are offered through computer-based testing 6 days per week, year round, at locations nationwide. Additional information, including examination fees and continuing education requirements, may be found at http://www.ahima.org/certification/default.aspx. The American Academy of Professional Coders (AAPC) offers a myriad of credentials, specifically for coders, with an emphasis on outpatient coding. The primary credentials are the CPC (Certified Professional Coder) and the CPC-H (Certified Professional Coder, hospital-based). There are also credentials for coding professionals in the payer community as well as 20 medical specialties. The AAPC also offers certification in auditing and compliance. The eligibility requirements for AAPC credentials consist of membership in AAPC and passing the exam. Chapter 3 of this textbook discusses the impact of the landmark federal legislation passed in the United States in 2009 that set goals and provided funding for the implementation of technology in health care delivery. Some of the funding administered by the Office of the National Coordinator for Health Information Technology (ONC) is dedicated to educating and training the new workforce of health information technology (HIT) professionals that will support health care in the electronic age. As part of these efforts, the ONC has developed a series of competency examinations for an array of short, nondegree programs offered by community colleges across the country. Called HIT PRO Exams, these tests show competency for a number of specialties (Office of the National Coordinator for Health Information Technology, 2012): • Practice workflow and information management redesign specialists • Clinician/practitioner consultants • Implementation support specialists • Trainers Clinical professionals work together to care for the patient. Developing a diagnosis is generally the responsibility of the physician. The physician will also prescribe any medication or therapies. However, the care of the patient involves many different individuals, including the patient. The patient care plan may be as simple as instructions to “take two aspirin and drink plenty of fluids,” or it may be a multiple-page document with delegation of responsibilities. Suppose a patient has been diagnosed with Type I diabetes mellitus, a disease characterized by chronic high blood glucose that can be controlled only with medication (i.e., insulin). The patient care plan might have the following parts:
Health Care Delivery Systems
Chapter Objectives
Vocabulary
Health Care Professionals
Physicians
PHYSICIAN SPECIALTY
DESCRIPTION
Allergist
Diagnoses and treats patients who have strong reactions to pollen, insect bites, food, medication, and other irritants
Anesthesiologist
Administers substances that cause loss of sensation, particularly during surgery
Cardiologist
Diagnoses and treats patients with diseases of the heart and blood vessels
Dermatologist
Diagnoses and treats patients with diseases of the skin
Family practitioner
Delivers primary health care for patients of all ages
Gastroenterologist
Diagnoses and treats patients with diseases of the digestive system
Gynecologist
Diagnoses and treats disorders of, and provides well care related to, the female reproductive system
Hospitalist
Employed by a hospital; medical practice focuses on patient care situations specific to acute care settings
Neonatologist
Diagnoses and treats diseases and abnormal conditions of newborns
Obstetrician
Cares for women before, during, and after delivery
Oncologist
Diagnoses and treats patients with cancer
Ophthalmologist
Diagnoses and treats patients with diseases of the eye
Orthopedist
Diagnoses and treats patients with diseases of the muscles and bones
Pathologist
Studies changes in cells, tissue, and organs in order to diagnose diseases and/or to determine possible treatments
Pediatrician
Delivers primary health care to children
Psychiatrist
Diagnoses and treats patients with disorders of the mind
Radiologist
Uses radiography and other tools to diagnose and treat a variety of diseases
Nurses
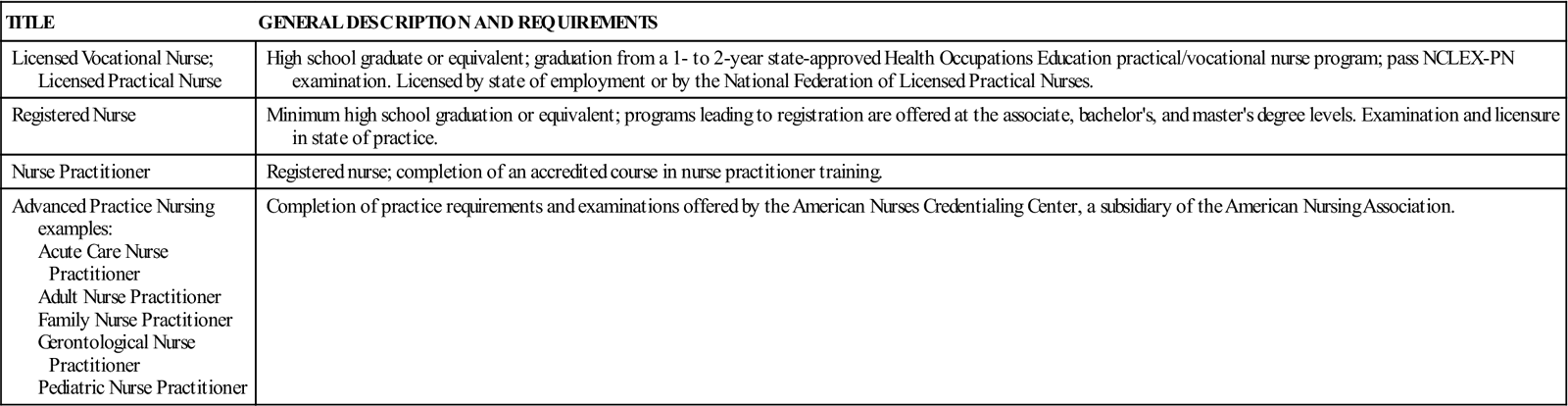
Licensed Practical Nurse
Registered Nurse
Advanced Practice Nursing Specialties
Allied Health Professionals
TITLE
DESCRIPTION
REQUIREMENTS
Occupational Therapist
Focuses on returning patient to maximal functioning in activities of daily living. Primarily employed in rehabilitation facilities but may work in virtually any health care environment.
Bachelor’s degree; licensure required in most states; certification (registration) can be obtained from the American Occupational Therapy Association.
Phlebotomist
Draws blood for donation and testing. Primarily employed in health care facilities and community blood banks.
High school graduate or equivalent. Completion of 10- to 20-hour certification program in a hospital, physician’s office, or laboratory. Completion of a vocational education program as a phlebotomist.
Physical Therapist
Focuses on strength, gait, and range-of-motion training to return patients to maximal functioning in activities of daily living. Primarily employed in rehabilitation facilities but may work in virtually any health care environment.
Master’s or doctoral degree; licensure by state of practice. All accredited programs will be required to offer the doctoral degree by 2015.
Registered Dietitian
Manages food services; evaluates nutritional needs, including planning menus and special diets and educating patients and family. Primarily employed in health care facilities.
Bachelor’s degree; registration can be obtained from American Dietetic Association; licensure, certification, or registration required in many states.
Respiratory Therapist
Delivers therapies related to breathing. Employed primarily in health care facilities.
Associate or bachelor’s degree; licensure or certification required in most states; registration can be obtained from the National Board for Respiratory Care.
Professional Organizations
Health Information Management
TITLE
DESCRIPTION
REQUIREMENTS
Certified Coding Specialist (CCS) or Certified Coding Specialist/Physician-based (CCS-P) or Certified Coding Associate (CCA)
Assigns, collects, and reports codes representing clinical data. Primarily employed in health care facilities.
Certification by examination from the American Health Information Management Association.
Certified in Healthcare Privacy and Security (CHPS)
Specializes in privacy and security aspects of HIM practice.
A combination of education or credentials and health care data experience, ranging from an associate degree and 6 years of experience to a master’s degree and 2 years of experience.
Certified Health Data Analyst (CHDA)
Analyzes health care data
A combination of education or credentials and health care data experience, ranging from an associate degree and 5 years of experience to an advanced degree and 1 year of experience.
Clinical Documentation Improvement Professional (CDIP)
Supports the collection of clinical documentation
An RHIA, RHIT, CCS, CCS-P, RN, MD, or DO and 2 years of experience in clinical documentation improvement, or an associate’s degree or higher and 3 years of experience in the clinical documentation setting.
Health Unit Coordinator
Transcribes physician’s orders, prepares and compiles records during patient hospitalization. Primarily employed in acute care facilities, long-term care facilities, and clinics.
High school graduate or equivalent; community college; hospital training program; completion of a vocational education program in the area of ward clerk, unit secretary, or health unit coordinator.
Certification available from the National Association of Health Unit Coordinators.
Registered Health Information Technician
Provides administrative support targeting the collection, retention, and reporting of health information. Employed primarily in health care facilities but may work in a variety of settings, including insurance and pharmaceutical companies.
Associate degree from accredited Health Information Technology program; registration by examination from the American Health Information Management Association.
Registered Health Information Administrator
Provides administrative support targeting the collection, retention, and reporting of health information, including strategic planning, research, and systems analysis and acquisition. Employed primarily in health care facilities but may work in a variety of settings, including insurance and pharmaceutical companies.
Bachelor’s degree from accredited Health Information Administration program; registration by examination from the American Health Information Management Association.
Health Information Management Credentials
American Health Information Management Association
American Academy of Professional Coders
Office of the National Coordinator for Health Information Technology
Interdisciplinary Collaboration
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Health Care Delivery Systems
Get Clinical Tree app for offline access
