Gastrointestinal problems
 Just the facts
Just the factsIn this chapter, you’ll learn:
anatomy and physiology of the GI system
diagnostic tests for children with GI disorders
treatments and procedures used for children with GI disorders
GI disorders that affect infants and children.
Anatomy and physiology
The functions of the gastrointestinal (GI) tract enable ingestion and propulsion of food, digestion and absorption of food and nutrients needed by the body, and elimination of waste products.
Structures of the GI system
The GI system consists of two major components:
It’s alimentary, my dear Watson
The alimentary canal of the GI tract consists of a hollow, muscular tube that begins in the mouth and ends at the anus. It includes the:
oral cavity
pharynx
esophagus
stomach
small intestine
large intestine.
|
Accessories make the system
Accessory glands and organs that aid GI function include the:
salivary glands
liver
biliary duct system (gallbladder and bile ducts)
pancreas.
Digestion
Digestion starts in the oral cavity, where chewing (mastication), salivation (the beginning of starch digestion), and swallowing (deglutition) take place. (See The growing GI system.)
 Growing pains
Growing painsThe growing GI system
Here are some highlights of the developing GI system during the first few years of life.
Salivary assistance
Saliva production begins at age 4 months and aids in the process of digestion. Saliva contains mucus to protect oral mucosa and to coat food. Food breakdown begins in the mouth with the enzymes ptyalin and amylase.
The sucking and extrusion reflex (a reflex that protects the infant from food substances his system is too immature to digest) persists until ages 3 to 4 months.
Stomach
The stomach capacity of the neonate is 30 to 60 ml and gradually increases to 200 to 300 ml by age 12 months and to 1,500 ml in the adolescent.
Up until ages 4 to 8 weeks, the neonatal abdomen is larger than the chest and the musculature is poorly developed.
Spit-ups are frequent in the neonate because of the immature muscle tone of the lower esophageal sphincter and the low volume capacity of the stomach.
Peristalsis occurs within 2½ to 3 hours in the neonate and extends to 3 to 6 hours in older infants and children.
Digestive enzymes are deficient until at least ages 4 to 6 months; gas, diarrhea, sensitization for food allergies, and microscopic hemorrhages can develop if solid foods are introduced before this time.
Intestinal
From ages 1 to 3 years, the composition of intestinal flora becomes more adultlike and stomach acidity increases, reducing the number of GI infections.
Exposure to breast milk increases intestinal flora early on and provides some protection against viruses and pathologic flora.
Increased myelination of nerves to the anal sphincter allows for physiologic control of bowel function, usually at about age 2; psychological readiness for toilet training may occur at a later age.
Liver
The liver is immature at birth, resulting in inefficient detoxifying of substances and medications. Medication dosages may need to be adjusted.
The liver’s slow development of glycogen storage capacity makes the infant prone to hypoglycemia.
Infants are more prone to dehydration and fluid and electrolyte imbalances due to greater body surface area, high rate of metabolism, and immature kidney function.
The rise and fall of hormones
Hunger is controlled by the lateral hypothalamus in the brain. A fall in blood nutrients, a rise or fall in hormones governing metabolism, hunger contractions from the stomach, and emotional input signal the hypothalamus to stimulate hunger. Fullness of the stomach, blood levels of nutrients and hormones, and emotions or habits stimulate the satiety center in the ventromedial area of the hypothalamus to decrease hunger.
The tasteful tongue
The tongue provides the sense of taste and is the strongest muscle in the body. Saliva secreted from the salivary glands moistens the mouth and lubricates the food bolus to ease swallowing.
 It’s all relative
It’s all relativeChoking hazards
Foods that are round and less than 1¼” (3.2 cm) in diameter can obstruct the airway of a child when swallowed whole.
Teach parents to cut foods into small pieces to prevent obstruction of the airway. Common foods that may cause choking include:
hot dogs
Vienna sausages
nuts
popcorn
marshmallows
grapes
hard candy
fruits with pits
dried beans.
Look out stomach, here it comes!
When a person swallows a food bolus:
 As food moves through the esophagus, glands in the esophageal mucosal layer secrete mucus, which lubricates the food and protects the esophageal mucosal layer from being damaged by poorly chewed foods. (See Choking hazards.)
As food moves through the esophagus, glands in the esophageal mucosal layer secrete mucus, which lubricates the food and protects the esophageal mucosal layer from being damaged by poorly chewed foods. (See Choking hazards.) Lower esophageal contractions (called peristalsis) gradually push the food down the esophagus and through the lower esophageal sphincter into the stomach.
Lower esophageal contractions (called peristalsis) gradually push the food down the esophagus and through the lower esophageal sphincter into the stomach.Stomach
Until the child is approximately age 2 years, the stomach is round. It will gradually elongate and take the adult shape and position in the abdomen by age 7 years.
The stomach lies in the left upper quadrant of the abdomen and is made up of three parts:
 The fundus is an enlarged portion above and to the left of the esophageal opening in the stomach; the cardiac sphincter is at the opening of the esophagus to the stomach.
The fundus is an enlarged portion above and to the left of the esophageal opening in the stomach; the cardiac sphincter is at the opening of the esophagus to the stomach.A gastric response
The secretory cells in the lining of the stomach are believed to be functional at birth. The lining of the stomach secretes gastrin in response to stomach wall distention. In turn, gastrin stimulates the release of highly acidic digestive secretions consisting mainly of pepsinogen, which is converted to pepsin, hydrochloric acid, intrinsic factor, and proteolytic enzymes. Limited amounts of water, alcohol, and some drugs are absorbed in the stomach. Intrinsic factor is necessary for vitamin B12 absorption.
|
Triple overtime
The stomach’s three functions are to store food, mix food with gastric juices via peristaltic contractions, and slowly distribute this food (now called chyme) into the small intestine through the pyloric opening for further digestion and absorption.
Contractions and secretions
Peristaltic contractions and various digestive secretions break down carbohydrates, proteins, and fats, enabling the intestinal mucosa to absorb these nutrients, along with water and electrolytes. Secretin and cholecystokinin are the hormones that affect intestinal secretions and gastric motility.
Distribution center
The surface area of the small intestine is increased by millions of villi in the mucous membrane lining. Digested food is absorbed through the mucosal walls and into the blood for distribution throughout the body. Failure to feed, malnutrition, ischemia, and infections affect the small intestine’s ability to absorb nutrients, resulting in growth delays.
Large intestine
The ileocecal valve is the sphincter between the ileum of the small intestine and the cecum of the large intestine. It prevents secretions from returning to the ileum. By the time chyme passes
through the small intestine and enters the ascending colon of the large intestine, it has been reduced to mostly indigestible substances.
through the small intestine and enters the ascending colon of the large intestine, it has been reduced to mostly indigestible substances.
Downward spiral
From the ascending colon, chyme passes through the transverse colon and descending colon to the rectum, and finally into the anal canal, where it’s expelled. The anal sphincter voluntarily controls defecation except in infants and patients with spinal cord injuries.
A large job description
The large intestine doesn’t produce hormones or digestive enzymes; it is, however, the site of water and sodium and potassium absorption. The mucosa produces alkaline secretions that lubricate the intestinal wall as chyme pushes through and protect the mucosa from acidic bacterial actions. The large intestine also harbors bacteria, such as Escherichia coli and Enterobacter aerogenes, which help to break down cellulose into usable carbohydrates and synthesize vitamin K. Vitamin K is needed by humans for blood clotting. Older children and adults get most of their vitamin K from bacteria in the gut, and some from their diet. Babies have very little vitamin K in their bodies at birth. Vitamin K does not cross the placenta to the developing baby, and the gut does not have any bacteria to make vitamin K before birth. After birth, there is little vitamin K in breast milk and breast-fed babies can be low in vitamin K for several weeks until the normal gut bacteria start making it. Infant formula has added vitamin K, but even formula-fed babies have very low levels of vitamin K for several days. With low levels of vitamin K, some babies can have very severe bleeding—sometimes into the brain, causing significant brain damage. This bleeding is called hemorrhagic disease of the newborn (HDN). As a preventive measure, babies are routinely given vitamin K injections at birth.
|
Accessory glands and organs
Allied with the GI tract are the liver, biliary duct system, and pancreas, which contribute the hormones, enzymes, and bile that are vital to digestion.
Liver
The liver is located in the right upper quadrant (RUQ) of the abdomen and is the body’s largest gland. It plays an important role in carbohydrate metabolism, detoxifies various endogenous and exogenous toxins in plasma, and synthesizes plasma proteins, nonessential amino acids, and vitamin A.
Essential storage
The liver also stores essential nutrients, such as iron and vitamins K, D, and B12. It secretes bile and removes ammonia from body fluids, converting it to urea for excretion in urine.
Biliary duct system
Bile is a greenish fluid that aids the small intestine to emulsify and absorb fats and fat-soluble vitamins and also neutralizes stomach acids. Bile exits through bile ducts that merge into the right and left hepatic ducts to form the common hepatic duct. This common duct joins the cystic duct from the gallbladder to form the common bile duct to the duodenum.
|
Gallbladder
The gallbladder, located beneath the liver, stores and concentrates bile produced by the liver. Secretion of the hormone cholecystokinin causes the gallbladder to contract and relax the ampulla of Vater, releasing bile into the common bile duct for delivery to the duodenum.
Pancreas
The pancreas is a large gland located behind the stomach and attached to the duodenum. The pancreas performs exocrine and endocrine functions. Its exocrine function involves cells that secrete digestive enzymes, bicarbonate, and hormones into the small intestine to aid in digestion.
Alpha beta Langerhans
The endocrine function of the pancreas involves the islets of Langerhans, which house alpha and beta cells. Alpha cells secrete glucagon, which stimulates glycogenolysis in the liver. Beta cells secrete insulin to promote carbohydrate metabolism.
Diagnostic tests
Tests used to diagnose GI disorders include barium enema, barium swallow, endoscopic retrograde cholangiopancreatography (ERCP), endoscopy, and stool specimen testing.
Barium enema
A barium enema, also called a lower GI series, allows X-ray visualization of the colon. Barium is dripped into the rectum by gravity, and a series of X-rays is taken as the barium passes through the lower GI tract.
Nursing considerations
Explain the procedure to the child and his parents. Prepare the child for insertion of the barium, and explain that he may be slightly uncomfortable as he changes positions on the X-ray table. Also explain that the child will have to wait until the test is over to go to the bathroom and that his bowel movements may look whitish until the barium has passed through his system.
Usually, the child will be on a liquid diet for 24 hours before the test.
An interesting way to start the day
Bowel preparations are administered before the examination; an enema the night before the test, the morning of the test, or both may be used for children and infants. (Prepare the child for the enema and provide as much privacy as possible.)
Tell the child that X-rays will be taken on a test table and that he must hold still (even though he’ll feel like he has to go to the bathroom).
Cover the genital area with a lead apron during the X-rays.
Exit the barium
Hydrate the child well with electrolyte-containing fluids after the procedure to prevent dehydration and to help expel the barium to prevent barium impaction.
Barium swallow
A barium or diatrizoate meglumine (Gastrografin) swallow, also called an upper GI series, provides imaging of the upper GI tract. It’s used primarily to examine the esophagus.
Follow the swallow
A series of X-rays is taken while the swallowed barium or Gastrografin moves into the esophagus, stomach, and duodenum to reveal abnormalities. The barium outlines the stomach walls and delineates ulcer craters and filling defects. Gastrografin and barium facilitate imaging through X-rays, but Gastrografin is less toxic if it escapes from the GI tract.
Seeking the ileocecal valve
A small bowel series is an extension of the upper GI series; additional imaging is done as the barium or Gastrografin flows farther down the GI tract through the small intestine to the ileocecal valve.
|
Nursing considerations
Explain the procedure to the child and his parents. Tell the child that he’ll need to take big swallows of a thick drink that looks like a milkshake (but doesn’t taste as good). Explain
that pictures will be taken while he’s drinking and afterward, and that he’ll need to hold still during the X-rays.
Maintain the child on a nothing-by-mouth (NPO) status beginning at midnight before the test.
After the test, monitor bowel movements for excretion of barium and monitor GI function.
Endoscopic retrograde cholangiopancreatography
In ERCP, a contrast medium is injected into the duodenal papilla to allow radiographic examination of the pancreatic ducts and hepatobiliary tree.
Nursing considerations
Obtain written, informed consent after explaining the procedure to the child and his parents. In addition:
Check the child’s history for allergies to cholinergics and iodine.
Administer a sedative and monitor the child for the drug’s effect.
It’s all over
After the procedure:
Monitor the child’s gag reflex. (The child remains on NPO status until his gag reflex returns.)
Protect the child from aspiration of mucus by positioning him on his side.
Monitor the child for urine retention.
Endoscopy
Endoscopy allows visualization of the GI system (and, when needed, biopsy of tissue) with a fiber-optic scope.
The direct approach
Fiber-optic testing allows direct visualization of the GI tract. Different types of fiber-optic testing are used to examine different portions of the GI tract:
Esophagogastroduodenoscopy allows visual inspection of the esophagus, stomach, and duodenum.
Colonoscopy allows direct visualization of the descending, transverse, and ascending colon.
Proctosigmoidoscopy allows inspection of the anus, rectum, and distal sigmoid colon.
|
Nursing considerations
Explain the procedure to the child and his parents, and make sure that written, informed consent has been obtained.
Oral and tongue piercings must be removed. They may accidently dislodge and enter airway as foreign bodies.
Prepare the child for sedation by explaining that it will make him sleepy and will keep him from hurting during the procedure.
A mild sedative may be administered before the examination; prepare the child for insertion of an intravenous (I.V.) line for sedation during this procedure.
The child may be kept on NPO status beginning at midnight before the test for an upper GI series.
The child may be placed on a liquid diet for 24 hours before the examination or require enemas and laxatives until the bowel is clear for a lower GI series.
After the procedure, assess vital signs for dyspnea and fever with a decrease in blood pressure and an increase in pulse, indicating the possibility of bleeding from perforation.
Stool specimen
Stool specimens are obtained to examine the stool for suspected GI bleeding, infection, or malabsorption. Tests include the guaiac test for occult blood and microscopic tests for ova, parasites, and fat.
Nursing considerations
Nursing interventions focus on proper collection and handling of the specimen.
Obtain the specimen in the correct container (the container may need to be sterile or contain a preservative).
Be aware that the specimen may need to be transported to the laboratory immediately or placed in the refrigerator.
For infants, stool specimens may be obtained from the diaper. However, apply a urine bag to prevent urine from contaminating the stool.
Treatments and procedures
Treatments and procedures for children with GI disorders include alternative feeding methods, total parenteral nutrition (TPN), GI intubation, and ostomy creation.
Alternative feeding methods
Children who are unable to take nutrients by mouth (for example, premature neonates with a poor sucking reflex, children who can’t take in enough calories, or children with disorders of the mouth
and esophagus, such as atresia and fistulas) are fed by alternative feeding methods. These methods include nasogastric (NG) gavage, orogastric (OG) gavage, duodenum and jejunum gavage, gastrostomy feedings, and jejunostomy feedings. These feedings may be administered intermittently or continuously.
and esophagus, such as atresia and fistulas) are fed by alternative feeding methods. These methods include nasogastric (NG) gavage, orogastric (OG) gavage, duodenum and jejunum gavage, gastrostomy feedings, and jejunostomy feedings. These feedings may be administered intermittently or continuously.
Nursing considerations
Explain to the child and his parents why the alternative feeding method is needed, and prepare the child for insertion of the feeding tube.
Nasogastric and orogastric feedings
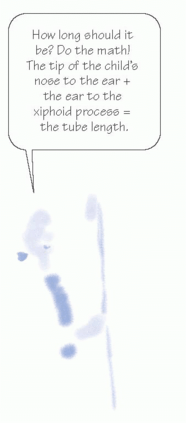
In NG and OG feedings, a tube is inserted into the stomach by way of one of the nares (NG) or the mouth (OG). Follow these steps:
To determine the correct length of the feeding tube, measure from the tip of the child’s nose to his ear and add to that amount the length from his ear to his xiphoid process.
Cold coil in a cup
Lubricate the tube with sterile water or a water-soluble lubricant before administration.
Facilitate insertion of the NG tube by having the child take large swallows of water as the tube is being inserted; allow the child to practice first.
When the feeding tube is secured, check placement immediately, at the start of intermittent feedings, and at least every 4 hours thereafter.
Inject 1 cc of air for infants and 5 cc of air for children into the feeding tube, and auscultate for gurgling sounds in the stomach when the air is injected. Alternate methods of checking placement are to aspirate a small amount of stomach contents and apply pH paper to check acidity level. Measure the tube from the nose or mouth to the end and record in the nurse’s notes every shift. If the tube is to be left in place, an X-ray may be ordered to check placement.
|
Recycle the residual
Check the residual amount of formula by aspirating stomach contents into a syringe. Record the amount of residual formula and the color, odor, and consistency of the gastric contents before refeeding the contents.
Administer feeding by gravity or feeding pump.
Clear the clogs
Irrigate the feeding tube with 10 ml of sterile water after each feeding to prevent stagnant formula from clogging the tube.
Record the total amount of formula administered and describe how well it was tolerated. Observe for signs of aspiration and intolerance, including low oxygen saturation, difficulty breathing, increased crying or discomfort, and vomiting.
Pinch and position
If the feeding tube will be removed after feeding, pinch the tube while withdrawing it to prevent aspirating fluid left in the tube.
Position the child with his head elevated during the feeding and for 1 hour afterward to prevent aspiration.
Sucking for satiation
When feeding infants by NG or OG tube, nonnutritive sucking is essential for oral stimulation. It helps the infant to relate a full stomach with oral sucking and fulfills the developmental need to suck.
Duodenum and jejunum gavage feedings
Duodenum and jejunum gavage feedings are administered with indwelling feeding tubes in the duodenum or jejunum.
Feedings are administered as they are with NG and OG feedings; however, the residual gastric contents and tube placement don’t need to be checked. Duodenum and jejunum feeding tubes aren’t removed after each feeding.
Gastrostomy and jejunostomy feedings
Gastrostomy and jejunostomy feedings are administered with a surgically placed feeding tube. The tube has one exit site on the abdomen but is composed of two separate chambers, each with a unique entry port. One side of the tube ends in the stomach and is typically used for medication administration. The other side of the tube ends in the jejunum and is typically used for formula administration.
|
It wouldn’t work in outer space
In gastrostomy and jejunostomy feedings:
Boluses of formula or water are administered by gravity or by feeding pump.
The feeding tube must be flushed with sterile water after each feeding to prevent clogs.
The child should be positioned with his head elevated at a 30-degree angle after feeding to prevent aspiration and encourage gastric emptying.
Long-term gastrostomy tubes have a button closure that allows for the removal of the gastrostomy tube between feedings.
As with NG or OG tubes, infants fed by gastrostomy tube should engage in nonnutritive sucking for oral stimulation. It helps the infant to relate a full stomach with oral sucking and fulfills the developmental need to suck.
Total parenteral nutrition
TPN provides nutrients intravenously for infants and children who aren’t able to take GI feedings, if GI feedings can’t provide enough nutrition, or if feedings are needed long-term.
Concentrate on TPN
TPN is a highly concentrated solution of protein, glucose, vitamins, and minerals. It’s infused through I.V. tubing with a special filter to remove particulate matter and microorganisms. Lowglucose solutions may be administered through a peripheral I.V. line. High-glucose solutions are administered through central I.V. lines. Some medications, such as heparin and ranitidine (Zantac), may be added to the TPN solution and, therefore, shouldn’t be administered separately.
TPN is typically administered with an intralipid infusion that provides necessary lipids and calories.
Nursing considerations
Prepare the child for insertion of the peripheral or central line. It can be frightening to a child (or his parents) if a line is inserted in the neck or shoulder area. Using a doll to demonstrate may help the child understand what will happen.
In addition, follow these steps:
Monitor the infusion rate via the I.V. pump. Cycling TPN, if ordered, involves tapering the drip rate at the start and end of the infusion, which commonly requires hourly rate changes.
Infection inspection
Assess the insertion site for signs of infection and infiltration because TPN can cause significant tissue damage.
Bags of TPN should be changed every 24 hours; tubing should be changed according to your facility policy. The doctor will order changes to the contents of the TPN solution based on the child’s daily laboratory values. Inspect the bag of TPN; don’t hang it if the solution appears cloudy or if there are precipitates visible (if so, return it to the pharmacy).
Not too much, not too little
Monitor electrolytes for excesses and deficits, particularly hyperkalemia and hypophosphatemia.
Monitor the child’s blood glucose for hyperglycemia and administer insulin as ordered.
Reassure the parents that the TPN will provide all the nutrition the child needs.
|
GI intubation
GI intubation is the insertion of an NG tube for diagnostic and therapeutic purposes. It’s used to:
empty the stomach and intestine
aid in diagnosis and treatment of stomach and upper GI tract disorders
decompress obstructed areas
detect and treat GI bleeding
administer medications or feedings.
Nursing considerations
Prepare the child for insertion of the NG tube with a simple, age-appropriate explanation. Because many children panic at the sight of the tube, it’s important to maintain a calm and reassuring manner and provide emotional support.
In addition, follow these steps:
When inserting the tube, instruct the child to take swallows of water to ease insertion, which also gives the child a job to do and provides a degree of distraction.
What goes in must come out
Maintain accurate intake and output records.
Record the amount, color, odor, and consistency of gastric drainage every 4 hours.
When irrigating the tube, note the amount of normal saline solution instilled and aspirated.
Check for fluid and electrolyte imbalances.
Provide good oral and nasal care. Make sure the tube is secure and doesn’t put pressure on the nostrils.
|
Anchors away
To support the tube’s weight and prevent its accidental removal, anchor the tube to the child’s clothing.
After removing the tube from a child with GI bleeding, watch for signs and symptoms of recurrent bleeding.
Ostomy
An ostomy is an opening in the intestines with the intestinal wall drawn to the abdomen. A stoma is created to allow passage of intestinal contents. An ostomy can be permanent or temporary, depending on the reason for the ostomy and how much of the intestine has been removed.
Correct the defect
An ostomy is created to correct an anatomical defect, relieve an obstruction, or permit treatment of an infection or injury to the intestinal tract. The most common reasons for an ostomy in infants and children are imperforate anus, necrotizing enterocolitis, Hirschsprung’s disease, and inflammatory bowel diseases.
Location, location, location
An ileostomy is placed in the ileum portion of the small intestine. A colostomy is placed in the large intestine and may be ascending, transverse, or descending, depending on where it’s placed.
Nursing considerations
Explain the procedure in simple, age-appropriate terms, preparing the child and his parents for all aspects of the surgery. Prepare the child and his parents for the postoperative period, specifically, what the child will see on his body and feel.
Bad timing
For older children and adolescents who are already concerned with appearance and acceptance by their peers, concerns about body image and, for the adolescent, sexuality are likely. Encourage the child to express these concerns and ask questions. (A same-gender nurse may be easier for the child to talk with.)
|
Been there, done that
If possible, introduce the child to a peer who has had the procedure and is handling it well. Refer the child to other health care professionals who can help him deal with his body image issue. Also note the following:
Mucus secretions begin within 48 hours after surgery.
Fecal drainage begins within 72 hours after surgery.
Edema of the stoma is present for 2 to 3 weeks after placement.
A wash and a pat-dry
When changing the stoma appliance (as needed), record the amount, character, color, and odor of the drainage; wash the stoma with soap and water, rinse, pat dry, apply adhesive material (skin sealant and stoma paste), and reapply the drainage bag.
Instruct the child and his parents in care of the ostomy.
If the skin is irritated, apply a protective ointment before applying the appliance.
An infant’s stoma may be left unpouched with a protective wafer around the stoma.
Pouch protector
In young children, protect the pouch from being pulled off by using one-piece shirt-and-pant outfits.
To control odor in the appliance, use deodorant drops, aspirin, or mouthwash solutions.
A low-residue diet may be required; avoid gas-producing foods or foods with strong odors.
Pass the salt
With an ileostomy, provide a diet high in sodium and potassium; avoid highly seasoned foods.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access