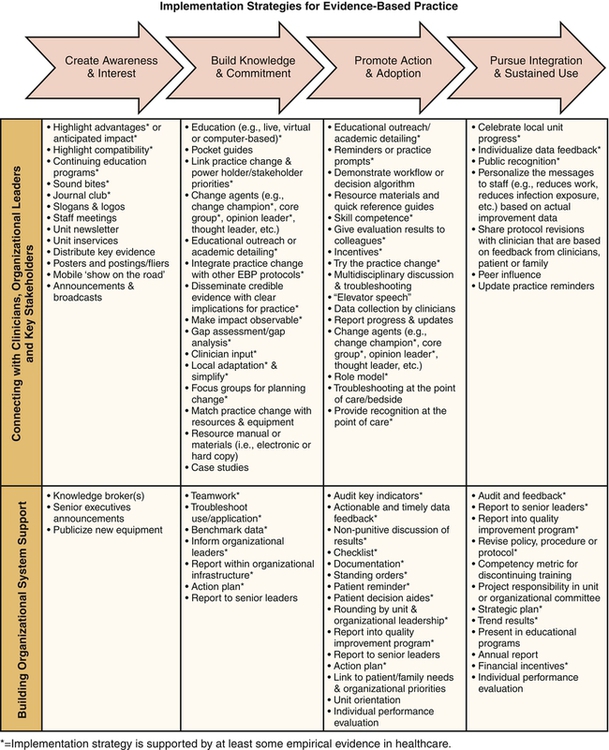
Laura Cullen, Cindy J. Dawson, Kirsten Hanrahan and Nancy Dole Nursing has a long history of using research to improve practice, beginning with Florence Nightingale’s work, reemphasized with research utilization efforts beginning in the 1980s, and progressing to the current trend in using best evidence in guiding patient care. There is now a rising expectation by consumers as well as in regulatory standards that evidence-based knowledge be used in health care. Despite national and international policy and research agendas, provision of evidence-based care does not meet expectations (Burns, 2012; Jablonski & Ersek, 2009; Randall et al., 2010; Revello & Fields, 2012; Scales et al., 2011; Schmaltz et al., 2011; Williams et al., 2005), and a continuing gap exists between the conduct and application of research findings. Using the evidence-based practice process to answer clinical and operational questions can be challenging. An understanding of evidence-based practice and related concepts requires requisite knowledge of a variety of terms. Evidence-based practice is a process of shared decision making in a partnership between patients and providers that involves the integration of research and other best evidence with clinical expertise and patient values and preferences in making health care decisions (Sigma Theta Tau International Research and Scholarship Advisory Committee, 2008). Evidence-based practice involves a process similar to research utilization. Research utilization encompasses critique of research studies, synthesis of findings, a determination of the applicability of findings, review for application with implementation of scientific findings in practice, an evaluation of the practice change, and dissemination of results to expand scientific knowledge. The shift from research utilization to evidence-based practice reflects the realization that not all clinical questions have been answered through research; thus other forms of evidence (e.g., lower rigor research, case studies, expert opinion) may be required to guide practice. An emphasis on use of evidence-based practice includes the application of the best available evidence and also represents a desire to improve patient outcomes with a consideration for patient values and preferences when making patient care decisions. Evidence-based practice is a broader, scientific process for improving health care quality and safety by building on what is learned from quality improvement, research utilization, and the conduct of research. Other terms are related to evidence-based practice yet are distinctly different. Best practice is popular term, but the definition remains elusive. Common use of the term describes innovative practices that are recognized by peer organizations and that contribute to meeting quality or fiscal goals (e.g., American Society for Quality; Australian Government Department of Veteran Affairs, Guideline for the Provision of Community Nursing Care). Although “best practice” and “evidence-based practice” are sometimes used interchangeably, the extent that best practices are evidence-based is often unclear. To promote understanding when using scientific evidence as guidance, evidence-based practice is the clear term to use. A clinical practice guideline is a statement designed to assist providers and clients in making decisions about appropriate health care for specific clinical circumstances (Sackett et al., 2000). Guidelines are systematically developed, they link the evidence with health outcomes (benefits and harms), and they continue to require subjective judgments when making decisions for use (Institute of Medicine, 2011a; Woolf & Atkins, 2001). Guidelines are developed with the intent to influence clinical behavior by making clear practice recommendations. A rigorous scientific process used to combine findings from research (usually randomized controlled trials) into a powerful and clinically useful report to guide practice is known as a systematic review. Standard components of a systematic review to consider are (1) process for initiating, (2) process for finding and assessing individual studies, (3) process for synthesizing the body of evidence; and (4) standard reporting format (Institute of Medicine, 2011b). Rigor used in development varies considerably among reports. Translational research includes testing the effect of interventions aimed at promoting the rate and extent of adoption of evidence-based practices by nurses, physicians, and other health care providers and describing organizational, unit, and individual variables that affect the use of evidence in clinical and operational decision making (Titler, 2004; Titler & Everett, 2001). Translational research has provided guidance about effective strategies for implementing evidence-based practice. Translational research is often used interchangeably with implementation science.Implementation science includes scientific investigations that support movement of evidence-based, effective health care approaches from clinical knowledge into routine use; testing strategies to promote uptake and use of innovations; and explaining factors that promote and hinder use of scientific knowledge in health care delivery (Eccles & Mittman, 2006; Greenhalgh et al., 2005; Rubenstein & Pugh, 2006; Titler, 2007). After initial pilot implementation and evaluation, the process used to promote integration of evidence-based practice is called reinfusion. Organizational context refers to the health system environment in which the proposed evidence-based practice is to be implemented. The core elements that help describe the organizational context include the prevailing culture of the system (e.g., patient-centered); the nature of human relationships in the system, including the leadership styles that are operational (e.g., team work, clear role delineation); and the organization’s approach to routine monitoring of performance of systems and services within the organization (Kitson et al., 2008; Spyridonidis & Calnan, 2011; Stetler et al., 2009; VanDeusen et al., 2010). Translational research has provided guidance about effective strategies for implementing evidence-based practice. Academic detailing or educational outreach is the use of a marketing strategy that uses presentations by a trained person who meets one-on-one with practitioners in their setting to provide information about the evidence-based practice. This may include feedback on the provider’s performance. The detailer may be from inside or outside the provider’s organization, and the information may be tailored to address site-specific barriers (Avorn & Soumerai, 1983; Davies et al., 1995; O’Brien et al., 2007; Sohn et al., 2004; Titler et al., 2002). The terms academic detailing and educational outreach are used interchangeably (Box 16-1). Informal leaders who influence peers by evaluating innovations for use in certain settings and promoting clinicians’ use of evidence in clinical decision making are referred to as opinion leaders. Opinion leaders are likeable, trustworthy, informative, and influential (Doumit et al., 2007; Majumdar et al., 2007). Performance gap assessment is a strategy of demonstrating an opportunity for improvement at baseline and outlining current practice related to specific indicators (Bullock-Palmer et al., 2008; Oxman et al., 1995). This data-driven strategy is used early in the implementation to garner commitment for practice changes. Work in nursing has led to the development of several evidence-based practice process models to guide nursing practice (Boyer et al., 2006; Goode et al., 2011; Logan et al., 1999; Rycroft-Malone & Bucknall, 2010; Rycroft-Malone et al., 2002; Stetler, 2001; Stevens, 2004; Titler et al., 2001). Evidence-based practice models have been used successfully to improve adoption of evidence-based practice recommendations (Block et al., 2012; Cullen et al., 2005; Dolezal et al., 2011; Hogan & Logan, 2004; Logan, et al., 1999) (Table 16-1). The Iowa Model (Titler et al., 2001) is one example used to guide clinician decision making in a variety of settings and is widely used. TABLE 16-1 Select Evidence-Based Practice Process Models Source: Cullen, L., Tucker, S., Hanrahan, K., Rempel, G., & Jordan, K. (2012). Evidence-based practice building blocks: Comprehensive strategies, tools, and tips (1st ed.). Iowa City: Department of Nursing Services and Patient Care, University of Iowa Hospitals and Clinics. The challenge for clinicians is to identify a model that guides practice and also promotes successful translation and implementation of evidence-based practice (Block et al., 2012; Cullen et al., 2012; Dolezal et al., 2011). Adoption of one evidence-based practice model across the organization and multidisciplinary initiatives (Gawlinski & Rutledge, 2008) is one strategy for promoting coordination of efforts. Evidence-based practice models tend to follow a basic problem-solving process and can be used parallel to other quality improvement processes (e.g., Six Sigma). Senior leadership support for evidence-based practice can be leveraged by outlining the similarities between evidence-based practice and existing quality improvement processes and structures and then synergistically blending them. Implementation of evidence-based practice changes can be challenging in complex health care settings. Despite the research supporting the use of effective strategies for implementing evidence-based practice changes, the use of ineffective implementation strategies persists (Bloom, 2005). In fact, Bloom (2005) stated that use of these ineffective implementation strategies results in “reduced patient care quality and raises costs for all, the worst of both worlds” (p. 380). Education is an essential first step to develop an understanding of why and how the evidence-based practice is done, but education alone does little to change practice (Farmer et al., 2008; Forsetlund et al., 2009; Jablonski & Ersek, 2009; Nicol et al., 2009; Pipe et al., 2009; Prior et al., 2008). In addition to education, multifaceted interactive interventions are needed to communicate the practice change to clinicians (Greenhalgh et al., 2005; Titler, 2008). The Diffusion of Innovations Model (Rogers, 2003) provides a theoretical framework that supports the hard work of implementing practice change in health care (Dobbins et al., 2002; Greenhalgh et al., 2005; Titler & Everett, 2001). Planning for implementation requires use of effective implementation strategies across phases of adoption. Although strong evidence supports the use of some strategies that promote the integration of evidence-based practice in health care, other strategies need further testing. The Evidence-Based Practice Implementation Guide (Figure 16-1) was developed to assist nurse leaders with planning and use of effective implementation strategies that advance stakeholders (both people and systems) through a process of diffusion: creating awareness and interest, building knowledge and commitment, promoting action and adaptation, and integrating and sustaining use (Cullen & Adams, 2012). The Evidence-Based Practice Implementation Guide can be used with evidence-based practice process models as a planning tool. Multiple interactive and reinforcing strategies, as outlined, promote adoption of evidence-based practice recommendations (Prior et al., 2008). Strategies to capture a busy clinician’s attention are important to include in the project implementation plan. Nurse leaders can identify additional strategies as they work across phases. Strategies are added to create a comprehensive implementation plan and momentum before, during, and after implementation. A number of strategies have good evidence and are particularly effective. Academic detailing or educational outreach is an implementation strategy that is effective in promoting adoption of evidence-based practice recommendations (O’Brien et al., 2007) by increasing knowledge and commitment to the change. Academic detailing involves a multifaceted approach to discussions with practitioners. Use of academic detailing has been shown to be an effective way to communicate with practitioners. Clinicians tend to buy into the need for the practice change when there is a strong evidence base, the topic addresses an identified need, data demonstrate an opportunity for practice improvement within the clinical area, and the practice change offers a relative advantage. Localizing or adapting practice recommendations to fit the local setting and culture is an essential step in the process, often using the role of the opinion leader and team of local experts (Doumit et al., 2007; Titler, 2008). When done by an opinion leader, academic detailing with a performance gap assessment is a highly effective example of using multifaceted interactive strategies in promoting adoption of evidence-based practice. In practice, this approach can be used to increase knowledge and garner consensus from a multidisciplinary team. Once the practice has been adapted and is ready for piloting, additional planning is needed for implementation and evaluation. Development of a fluid action plan can be highly effective in keeping the team on task and collectively moving forward (Cullen & Adams, 2012; Gifford et al., 2011; Schimizu & Shimanouchi, 2006). The following case example demonstrates the effectiveness of a staff nurse–led team, using an evidence-based practice model to address a clinically relevant issue for the patients and organizations. This project addresses blood pressure monitoring for obese patients (Dole & Griffin, 2009). Blood pressure has been described as a powerful, consistent, and independent risk factor for cardiovascular and renal disease (Pickering et al., 2005). One in three U.S. adults has hypertension (Centers for Disease Control and Prevention, 2012b). The prevalence of hypertension in Black Americans in the United States is among the highest in the world (Rosamond et al., 2007). In 2002 over 45 million ambulatory care visits to physician’s offices, hospital outpatient departments, and emergency departments were for essential hypertension (Rosamond et al., 2007). Over 300,000 hospitalizations in 2005 had their first-listed diagnosis of essential hypertension (Pickering et al., 2005; Rosamond et al., 2007). The project was accepted for development through an evidence-based practice staff nurse internship program (Cullen & Titler, 2004), thus garnering organizational support and establishing the project as an organizational priority. The unit culture supports the use of evidence-based practice as exemplified by the involvement of the nurse manager. The nurse manager fostered an environment in which opportunities for change were welcomed. In addition, the nurse manager ensured that non–patient care time was available for the staff nurse project director. The project director relied on the nurse manager for assistance with scheduling meetings, taking minutes, and providing follow-up on issues. The nurse manager was instrumental in the planning of the initiative rollout working with the system. The Iowa Model (Titler et al., 2001) was used to guide the process. A multidisciplinary team was formed with the assistance of the nurse manager. Evidence was needed to define the appropriate size of cuff and procedure for obtaining accurate readings. The literature search did show that with the increase in prevalence of obesity, cuff size has become very important. The National Health and Nutritional Examination Survey showed that the prevalence of obesity has increased in the United States from 22.9% in 1994, to over 30% in 2000, and 35.7% in 2010 (Centers for Disease Control and Prevention, 2012a). It has been shown that the most frequent error in measuring blood pressure in the outpatient population is “miscuffing” (Manning et al., 1983). Using a cuff that is too small accounts for over 80% of measurement errors. The morbidly obese patient often has a very large upper arm circumference with a relatively short upper arm length. This leads to incorrect cuffing when a thigh cuff is used. Studies have shown that using a cuff that is too small can overestimate a blood pressure reading (Zdrojewski et al., 2005). With the rise of obesity, the use of the forearm to measure blood pressure is becoming more prevalent. Several studies have been conducted comparing forearm readings with upper arm readings. Most researchers report that these readings are not interchangeable (Schell et al., 2007; Schell et al., 2010). A new procedure for blood pressure measurement was developed. The basic procedure for obtaining an accurate blood pressure reading is the following (Pickering et al., 2005; Rushing, 2004; Turner et al., 2008): • Measurements should be taken on the upper arm • The cuff bladder length should be at least 80% of arm circumference and the width should be at least 40% of upper arm length • The patient’s arm is supported horizontally at the level of the heart • If the patient is sitting both feet should be flat on the floor • The nurse and the patient should not talk during the procedure • Do not use the arm that has an IV or the side of a mastectomy • The patient should be sitting 3 to 5 minutes before measurement Staff training began when the new cuffs were available for clinic use (Table 16-2). The longer blood pressure cuffs were readily accepted by the staff and patients. No problems occurred once a supply of cuffs was available for the automatic blood pressure equipment. A policy was written on monitoring blood pressure on the obese arm in an outpatient setting and presented to the nursing policy committee. The committee requested that it be presented to the ambulatory nurse managers for their approval and resubmitted to the committee. The only suggestion was to revise the policy for both adult ambulatory and inpatient use. The revised policy was resubmitted and accepted. TABLE 16-2 Implementation Strategies Used From Cullen, L., & Adams, S. (2012). Planning for implementation of evidence-based practice. Journal of Nursing Administration, 42(4), 222-230.
Evidence-Based Practice
Strategies for Nursing Leaders
![]() http://evolve.elsevier.com/Huber/leadership/
http://evolve.elsevier.com/Huber/leadership/
DEFINITIONS
MODELS
Model
Citation
Sample Reports
Iowa Model
Titler, M.G., Kleiber, C., Steelman, V., Rakel, B., Budreau, G., Everett, L.Q., et al. (2001). The Iowa Model of evidence-based practice to promote quality care. Critical Care Nursing Clinics of North America, 13(4), 497-509.
Farrington, M., Lang, S., Cullen, L., & Stewart, S. (2009). Nasogastric tube placement in pediatric and neonatal patients. Pediatric Nursing, 35(1), 17-25.
Ottawa Model
Graham, K., & Logan, J. (2004). Using the Ottawa Model of Research Use to implement a skin care program. Journal of Nursing Care Quality, 19(1), 18-24.
Hogan, D.L., & Logan, J. (2004). The Ottawa Model of research use: A guide to clinical innovation in the NICU. Clinical Nurse Specialist: The Journal for Advanced Nursing Practice, 18(5), 255-261.
Stetler Model
Stetler, C.B. (2001). Updating the Stetler model of research utilization to facilitate evidence-based practice. Nursing Outlook, 49(6), 272-279.
Romp, C.R., & Kiehl, E. (2009). Applying the Stetler model of research utilization in staff development: Revitalizing a preceptor program. Journal for Nurses in Staff Development, 25(6), 278-284, quiz 285-286.
Model for EBP Change
Rosswurm, M.A., & Larrabee, J.H. (1999). A model for change to evidence-based practice. Image: Journal of Nursing Scholarship, 31(4), 317-322.
Boyer, D.R., Steltzer, N., & Larrabee, J.H. (2009). Implementation of an evidence-based bladder scanner protocol. Journal of Nursing Care Quality, 24(1), 10-16.
ARCC Model
Melnyk, B.M., & Fineout-Overholt, E. (2011). Evidence-based practice in nursing & healthcare. A guide to best practice (2nd ed.). Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins.
Wallen, G.R., Mitchell, S.A., Melnyk, B., Fineout-Overholt, E., Miller-Davis, C., Yates, J., & Hastings, C. (2010). Implementing evidence-based practice: Effectiveness of a structured multifaceted mentorship programme. Journal of Advanced Nursing, 66(12), 2761-2771.
IMPLEMENTING EVIDENCE-BASED PRACTICE CHANGES
AN EVIDENCE-BASED PRACTICE EXEMPLAR
Process
Synthesis of the Evidence
The Practice Change
Implementation
PLANNING PHASE
STRATEGIES USED FOR BLOOD PRESSURE MONITORING IN AMBULATORY CLINIC
Creating awareness and interest
Building knowledge and commitment
Promoting action and adoption
Pursuing integration and sustained use

Evidence-Based Practice: Strategies for Nursing Leaders
Get Clinical Tree app for offline access




