Evaluation
Objectives
• Discuss the relationship between critical thinking and evaluation.
• Describe the standards of professional nursing practice for evaluation.
• Give examples of evaluation measures for determining a patient’s progress toward outcomes.
• Evaluate the outcomes of care for a patient.
• Describe how evaluation leads to discontinuation, revision, or modification of a plan of care.
Key Terms
Evaluation, p. 265
Evaluative measures, p. 268
Nursing-sensitive outcome, p. 267
Standard of care, p. 271
![]()
When a repairman comes to a home to fix a leaking faucet, he turns the faucet on to determine the problem, changes or adjusts parts, and rechecks the faucet to determine if the leak is fixed. After a patient diagnosed with pneumonia completes a course of antibiotics, the health care provider often has him or her return to the office to have a chest x-ray examination to determine if the pneumonia has cleared. When a nurse provides wound care, including application of a warm compress, several steps are involved. He or she assesses the appearance of the wound, determines its severity, applies the appropriate form of compress, and returns later to determine if the condition of the wound has improved. These three scenarios depict what ultimately occurs during the process of evaluation. The repairman rechecks the faucet, the physician orders a chest x-ray film, and the nurse reinspects the patient’s wound. Evaluation involves two components: an examination of a condition or situation and a judgment as to whether change has occurred. Ideally after an intervention takes place, evaluation reveals an improvement, a desired outcome.
The previous chapters on the nursing process describe how you apply critical thinking to gather patient data, form nursing diagnoses, develop a plan of care, and implement interventions in the care plan. Evaluation, the final step of the nursing process, is crucial to determine whether, after application of the nursing process, the patient’s condition or well-being improves. You apply all that you know about a patient and his or her condition and your experiences with previous patients to evaluate whether nursing care was effective. You conduct evaluative measures to determine if your patients met expected outcomes, not if nursing interventions were completed. The expected outcomes established during planning are the standards against which the nurse judges whether goals have been met and if care is successful.
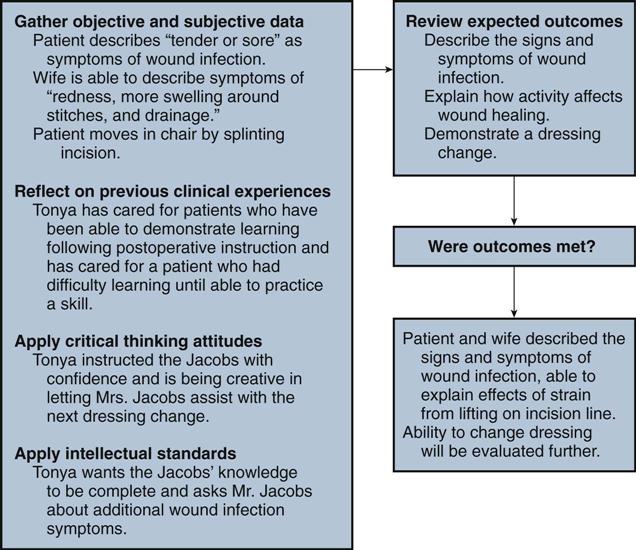
In the continuing case study, Tonya has instructed Mr. Jacobs about necessary wound care. Mrs. Jacobs also participates in the education session. Tonya discusses with the family the importance of wound care in preventing infection and has Mr. and Mrs. Jacobs observe the dressing change. During the dressing change Tonya uses safe and appropriate intervention techniques to protect the integrity of the wound and minimize transmission of infection. She also discusses how physical stress such as bending and lifting strains a suture line; thus Mr. Jacobs needs to limit activity for the first few weeks after surgery. Tonya encourages the Jacobs to ask any questions they have about wound care. Tonya returns to Mr. Jacobs’ room an hour later to evaluate the results of her instruction. For the nursing diagnosis of deficient knowledge, Tonya set the expected outcomes of: “Patient and wife will describe the signs and symptoms of a wound infection, explain how activity affects wound healing, and demonstrate a dressing change correctly.” Mr. Jacobs is resting in bed, and Mrs. Jacobs is reading one of the instruction brochures as Tonya enters the room. Tonya says, “Mrs. Jacobs, I see that you’re reviewing the booklet I gave you. Do you have any questions”? Mrs. Jacobs responds, “I guess I understand what to look for with an infection. I hope I can recognize changes.” Tonya asks, “Tell me the signs of infection.” Mrs. Jacobs replies, “Redness, more swelling around the stitches, and drainage.” Tonya asks Mr. Jacobs, “Are there any other signs of infection?” Mr. Jacobs responds, “You said that my incision would feel more tender or sore and that I might have a fever.” “That’s right,” Tonya remarks. “Tell me why your doctor has limited your lifting for a month.” Mr. Jacobs answers, “So I don’t strain my incision and pull out the stitches.” “Right again,” Tonya affirms,” I think that before you go home tomorrow we should let you watch one more dressing change and even let your wife help me.”
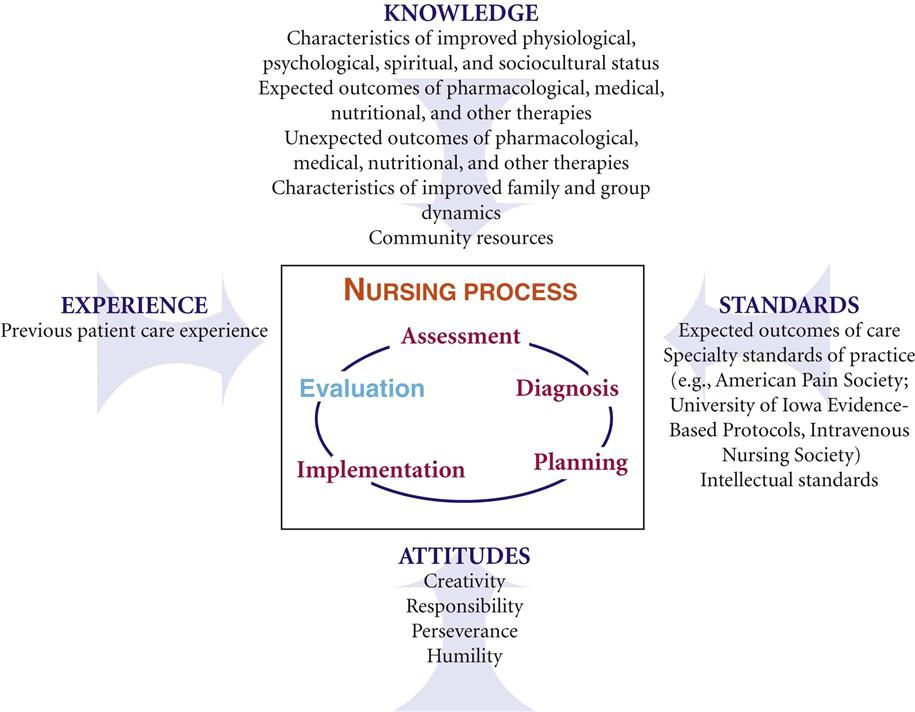
Evaluation is an ongoing process that occurs whenever you have contact with a patient. Once you deliver an intervention, you gather subjective and objective data from the patient, family, and health care team members. You also review knowledge regarding the patient’s current condition, treatment, resources available for recovery, and expected outcomes. By referring to previous experiences caring for similar patients, you are in a better position to know how to evaluate your patient. You can anticipate what to evaluate. Apply critical thinking attitudes and standards to determine whether outcomes of care are achieved (Fig. 20-1). If outcomes are met, the overall goals for the patient also are met. Compare patient behavior and responses that you assessed before delivering nursing interventions with behavior and responses that occur after administering nursing care. Critical thinking directs you to analyze the findings from evaluation (Fig. 20-2). Has the patient’s condition improved? Is the patient able to improve, or are there physical factors preventing recovery? To what degree does this patient’s motivation or willingness to pursue healthier behaviors influence responses to therapies?
During evaluation you make clinical decisions and continually redirect nursing care. For example, when Tonya evaluates the Jacobs’ learning, she applies knowledge of patient education principles and postoperative wound healing to interpret whether learning has occurred and whether further instruction is needed. Tonya knows that repetition is important in learning and thus plans another instruction session with the family during a dressing change the next day. Evaluative findings determine Tonya’s next course of action. In the Jacobs’ case Tonya knows that this is the first time Mr. Jacobs has had major surgery. Mrs. Jacobs voiced concern about recognizing the signs of infection. To meet the outcomes of care, Tonya plans to discuss the appearance of the wound during normal healing and specifically how signs of infection present. She reinforces this explanation during the dressing change so Mr. and Mrs. Jacobs can look at the wound closely again under Tonya’s instruction.
Positive evaluations occur when the patient meets desired outcomes, which leads you to conclude that the nursing intervention(s) were effective. For example, in the case study Tonya notes that Mrs. Jacobs identified three signs and symptoms of infection and Mr. Jacobs identified two. Therefore Tonya determines the expected outcome of “describing signs and symptoms of wound infection” was partially met by the patient. However, further instruction is necessary. Unmet or undesirable outcomes such as incorrect or incomplete knowledge indicate that interventions are not effective in minimizing or resolving the actual problem or avoiding an at-risk problem. An unmet outcome reveals that the patient has not responded to interventions as planned. As a result, the nurse changes the plan of care by trying different therapies or changing the frequency or approach of existing therapies.
This sequence of critically evaluating and revising therapies continues until you and the patient successfully and appropriately resolve the problems defined by nursing diagnoses. Remember that evaluation is dynamic and ever changing, depending on the patient’s nursing diagnoses and conditions. As problems change, so do expected outcomes. A patient whose health status continuously changes requires more frequent evaluation. In addition, you evaluate priority diagnoses first. For example, Tonya continues to evaluate Mr. Jacobs’ acute pain before evaluating the status of his deficient knowledge.
Standards for Evaluation
Nursing care helps patients resolve actual health problems, prevent the occurrence of potential problems, and maintain a healthy state. The evaluation process is an integral step to that end. The American Nurses Association (ANA) defines standards of professional nursing practice, which include standards for the evaluation step of the nursing process (see Chapter 1). The standards are authoritative statements of the duties that all registered nurses, regardless of role, patient population they serve, or specialty, are expected to perform competently (ANA, 2010). The competencies for evaluation include being systematic and using criterion-based evaluation, collaborating with patients and other professionals, using ongoing assessment data to revise the plan, and communicating results to patients and families. It is also important to ensure the responsible and appropriate use of interventions to minimize unwarranted or unwanted treatment (ANA, 2010).
Criterion-Based Evaluation
You evaluate nursing care by knowing what to look for as described in the criterion-based standards included in a patient’s goals and expected outcomes. The goals and outcomes are objective criteria needed to judge a patient’s response to care.
Goals
A goal is the expected behavior or response that indicates resolution of a nursing diagnosis or maintenance of a healthy state. It is a summary statement of what will be accomplished when the patient has met all expected outcomes. For Mr. Jacobs Tonya selected the goal of, “Patient expresses acceptance of health status by day of discharge” for the nursing diagnosis of anxiety (see Chapter 18). Successful achievement of this goal depends on Tonya delivering interventions selected from the Nursing Interventions Classification (NIC), including acceptance of health status and anxiety level (see Nursing Care Plan, Chapter 18).
Goals often are also based on standards of care or guidelines established for minimal safe practice. For example, the Infusion Nurses Society (INS) has standards of care for prevention of the intravenous (IV) complication phlebitis (INS, 2006). When a nurse cares for a patient with a peripheral IV line, the goal, “The IV site will remain free of phlebitis,” is established on the basis of sound practice standards. The INS phlebitis scale contains physical criteria for determining phlebitis (see Chapter 41).
Expected Outcomes
An expected outcome is an end result that is measurable, desirable, and observable and translates into observable patient behaviors (ANA, 2010). It is a measure that tells you if the interventions applied in patient care led to successful goal achievement. When nurses apply the nursing process, a nursing-sensitive outcome is a measurable patient or family state, behavior, or perception largely influenced by and sensitive to nursing interventions (Moorhead et al., 2008). The interventions must be within the scope of nursing practice and integral to the processes of nursing care. Examples of nursing-sensitive outcomes include reduction in pain frequency, incidence of pressure ulcers, and incidence of falls (Box 20-1). In comparison, medical outcomes are largely influenced by medical interventions. Examples include patient mortality, surgical wound infection, and hospital readmissions. Outcomes are statements of progressive, step-by-step physical, emotional, or behavioral responses that the patient needs to accomplish to achieve the goals of care. When you achieve outcomes, the related factors for a nursing diagnosis usually no longer exist. Two of the expected outcomes for Mr. Jacobs’ goal of, “Patient expresses acceptance of health status by day of discharge,” are “Patient describes surgical outcomes in discussion with surgeon in 24 hours,” and “Patient shares concerns with wife before day of discharge.” Tonya evaluates Mr. Jacobs by observing for behaviors that reflect anxiety and discussing what the patient has learned from the surgeon and discussed with his wife. The related factor of “uncertainty over recovery” no longer exists if Mr. Jacobs is able to relate surgical outcomes discussed with the surgeon and reports having had a discussion about those outcomes with his wife.
Evaluation is not a description of the achievement of an intervention. Evaluation of Mr. Jacobs does not involve observing his ability to perform relaxation exercises for his anxiety. Evaluation does involve observation of the patient’s behavior (facial expression) during discussions about his recovery.
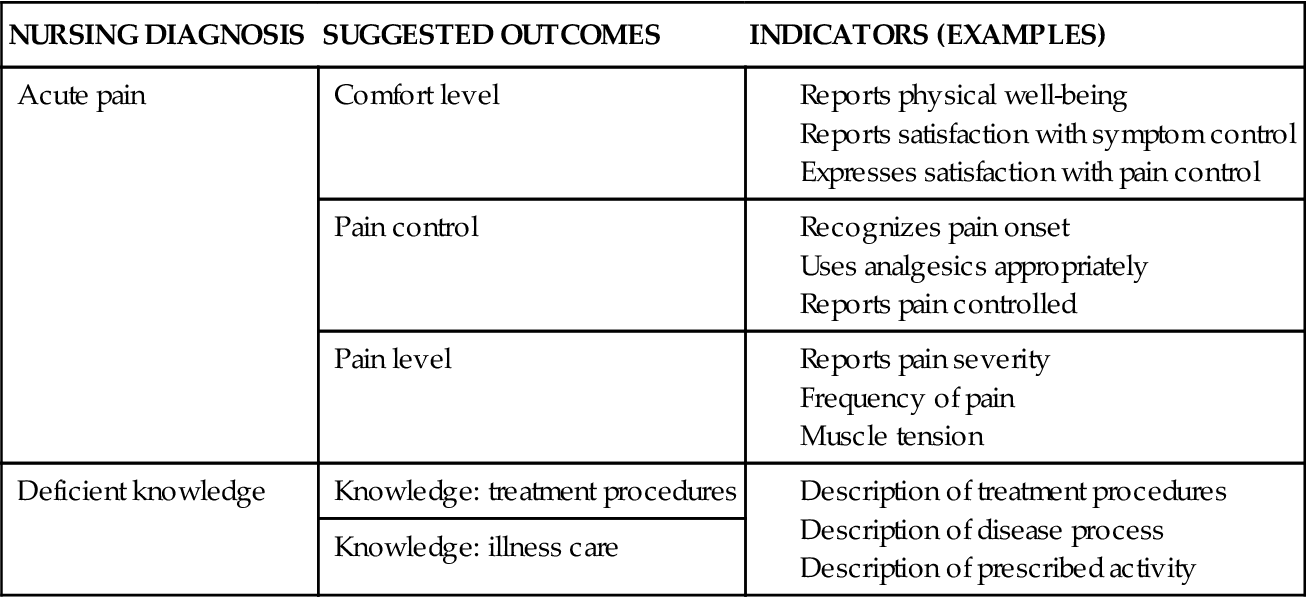
A valuable resource for selecting outcomes is the Nursing Outcomes Classification (NOC) (see Chapter 18). It offers a language for the evaluation step of the nursing process. The purposes of NOC are (1) to identify, label, validate, and classify nurse-sensitive patient outcomes; (2) to field test and validate the classification; and (3) to define and test measurement procedures for the outcomes and indicators using clinical data (Moorhead et al., 2008). Within the NOC taxonomy you can select outcomes specific for nursing interventions that relate to nursing diagnoses. The NOC project complements the work of NANDA International (NANDA-I) and the NIC project. The NOC classification offers nursing-sensitive outcomes for NANDA-I nursing diagnoses (Table 20-1). For each outcome there are specific recommended evaluation indicators (i.e., the patient behaviors or responses that are measures of outcome achievement).
TABLE 20-1
Linkages between Nursing Outcomes Classification and Nursing Diagnoses
| NURSING DIAGNOSIS | SUGGESTED OUTCOMES | INDICATORS (EXAMPLES) |
| Acute pain | Comfort level | |
| Pain control | ||
| Pain level | ||
| Deficient knowledge | Knowledge: treatment procedures | |
| Knowledge: illness care |
Collaborate and Evaluate Effectiveness of Interventions
An important aspect of patient-centered care and evaluation is collaboration. A nurse must respect the patient and family as a core member of the health care team, meaning that the patient and family must be actively involved in the evaluation process. When you develop patient care goals and expected outcomes with a patient, he or she becomes an important resource for being able to tell you if outcomes are being met. For example, a patient knows best if pain has lessened or if breathing is easier. The same holds true for the family, who often can recognize changes in patient behavior sooner than you can because of their familiarity with the patient. Members of the health care team who contribute to the patient’s care also gather evaluative findings.
Proper evaluation determines the effectiveness of nursing interventions, allowing you to answer the following questions: What is the patient’s response to nursing care? Was the therapy effective in improving the patient’s physical or emotional health? It is important to evaluate whether each patient reaches a level of wellness or recovery that the health care team and patient established in the goals of care. In addition, have you met the patient’s expectations of care? Ask patients about their perceptions of care such as, “Did you receive the type of pain relief you expected?” “Did you receive enough information to change your dressing when you return?” This level of evaluation determines the patient’s satisfaction with care and strengthens partnering between you and the patient.
Evaluative Measures
Evaluating a patient’s response to nursing care requires the use of evaluative measures, which are assessment skills and techniques (e.g., observations, physiological measurements, patient interview) (Fig. 20-3). In fact, evaluative measures are the same as assessment measures, but you perform them at the point of care when you make decisions about the patient’s status and progress. The intent of assessment is to identify which, if any, problems exist. The intent of evaluation is to determine if the known problems have remained the same, improved, worsened, or otherwise changed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree