Ethical dilemmas are not easy situations.
After completing this chapter, you should be able to:
• Define terminology commonly used in discussions about ethical issues.
• Analyze personal values that influence approaches to ethical issues and decision making.
• Discuss the moral implications of the American Nurses Association and International Council of Nurses codes of ethics.
• Discuss the role of the nurse in ethical health care issues.
• Recognize the role of genetics and genomics in nursing practice.
• Recognize resources to assist in resolving an ethical dilemma.
In developing the content for this chapter, a deliberate effort has been made to “simplify” the presentation of ethical issues and avoid complex philosophical debate. Many nurses shy away from formal ethical discussions, because the terminology seems better suited to graduate school and a peer-reviewed journal. In reality, nurses deal with ethical issues every day in practice and need to have the tools to advocate effectively for patients, as well as for themselves. The first step in equipping oneself for ethical debate is becoming comfortable with the language and issues. Ethics refers to principles of right and wrong behaviors, beliefs, and values. Thompson et al. (2007) add, “ethics is essentially concerned with our life as members of a community, and how we behave and function in society” (p. 36).
Concern about ethical issues in health care has increased dramatically in the past three decades. This interest has soared for a variety of reasons, including advances in medical technology; social and legal changes involving abortion, euthanasia, patient rights, end-of-life care, reproductive technology; and growing concern about the allocation of scarce resources, including a shortage of nurses. Nurses have begun to speak out on these issues and have focused attention on the responsibilities and the possible conflicts that they experience as a result of their unique relationship with patients and their families and their role within the health care team.
Understanding Ethics
Let us begin by defining commonly used terms (Box 19.1).
What Are Your Values?
Your values represent ideas and beliefs that you hold with high regard. Clarification of your values is suggested as a strategy to develop greater insight into yourself and what you believe to be important. Value clarification involves a three-step process: choosing, prizing, and acting on your value choices in real-life situations (Steele, 1983). Moreover, our values may impact how we practice as nurses and the decisions that we make each day in our professional practice (Wang, Chou, & Huang, 2010). Opportunities to make choices and improve your decision making are included in the following pages. As you consider your values, you will, I hope, gain more understanding about the underlying motives that influence them. It is not intended as a “right” or “wrong” activity; rather, it is a discovery about the “what” and “why” of your actions. Do not be surprised if your peers or family hold different views on some topics. And remember, the values that are “correct” or “right” for you may not always be the “right” values for others, including patients and their families. Your values may also change through time as you face different life experiences.
Evaluate the critical thinking questions, write down your responses to them, and consider the possible reason or reasons for your choices. The critical thinking exercise in Critical Thinking Box 19.1 is suggested as a means of clarifying your values. Discuss your answers with peers and decide how comfortable you are in discussing and defending your values, especially if they differ from the values of your peers. Critical Thinking Box 19.2 involves reproductive issues and has been included here because of the proliferation of reproductive technology, including genetics, and the ongoing moral and political debate regarding abortion and the use of stem cells.
Moral/Ethical Principles
What Is the Best Decision, and How Will I Know?
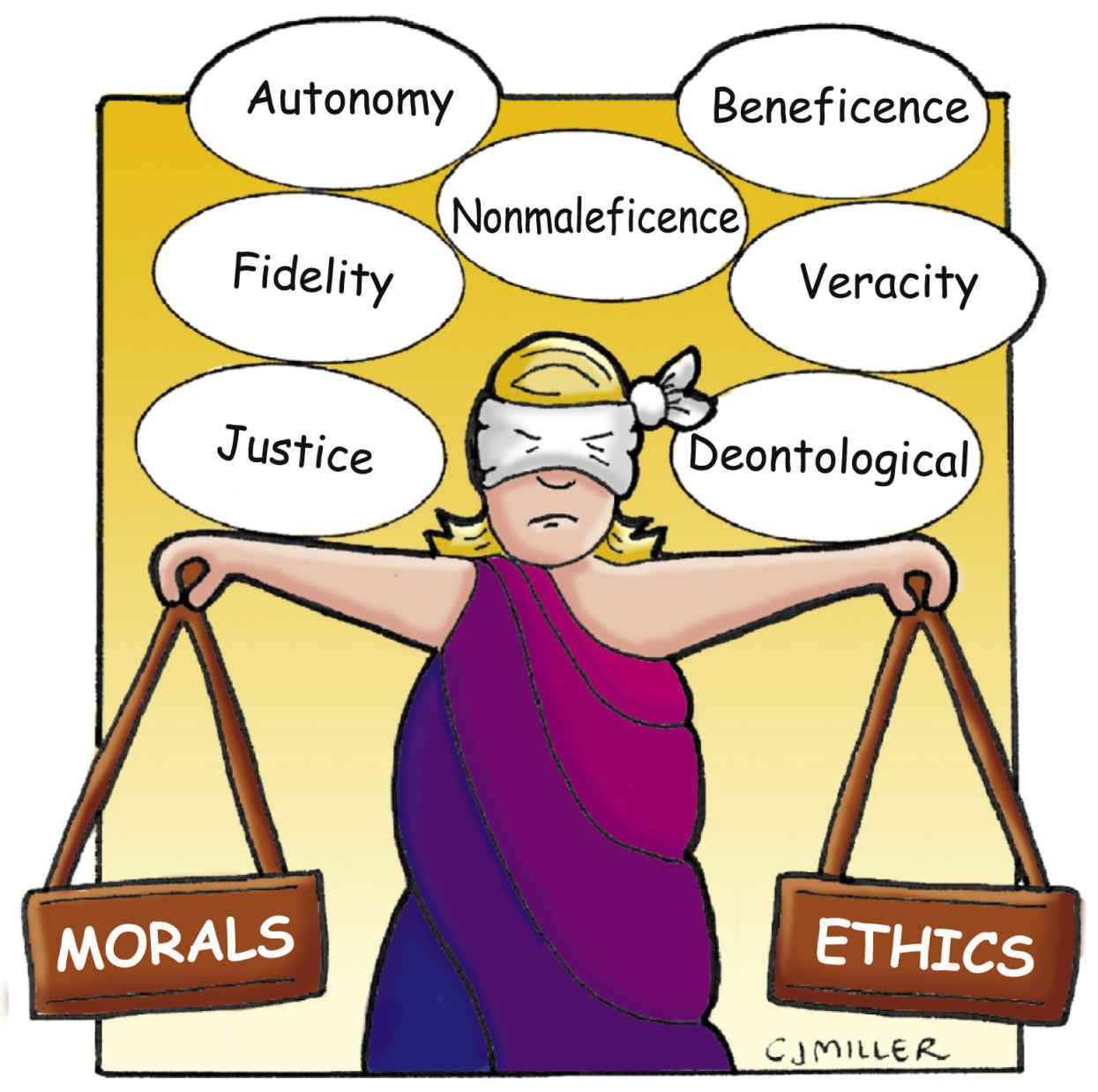
Despite different ideas regarding which moral or ethical principle is most important, ethicists agree that there are common principles or rules that should be taken into consideration when an ethical situation is being examined. As you read through each principle, consider instances in which you have acted on the principles or perhaps felt some conflict in trying to determine what was the best action to take (Fig. 19.1).
Autonomy: a patient’s right to self-determination without outside control
Autonomy implies the freedom to make choices and decisions about one’s own care without interference, even if those decisions are not in agreement with those of the health care team. This principle assumes rational thinking on the part of the individual and may be challenged when the individual infringes on the rights of others.
Consider this: What if a patient wants to do something that will cause harm to himself or herself? Under what circumstances can the health care team intervene?
Beneficence: duty to actively do good for patients
For example, you use this principle when deciding what nursing interventions should be provided for patients who are dying when some of those interventions may cause pain. In the course of prolonging life, harm sometimes occurs.
Consider this: Who decides what is good? Patient, family, nurse, or physician? How do you define good?
Nonmaleficence: duty to prevent or avoid doing harm, whether intentional or unintentional
Is it harmful to accept an assignment to “float” to an unfamiliar area that requires the administration of unfamiliar medications?
Consider this: Is it acceptable to refuse an assignment? When does an assignment become unsafe?
Fidelity: the duty to be faithful to commitments
Fidelity involves keeping information confidential and maintaining privacy and trust (e.g., maintaining patient confidentiality regarding a positive HIV test or “blowing the whistle” about unscrupulous billing practices).
Consider this: To whom do we owe our fidelity? Patient, family, physician, institution, or profession? Who has the right to access patient medical records? When should we “blow the whistle” about unsafe staffing patterns?
Justice: the duty to treat all patients fairly, without regard to age, socioeconomic status, or other variables
This principle involves the allocation of scarce and expensive health care resources. Should uninsured patients be allowed to use the emergency department (ED) for nonemergency care—the most expensive route for delivering this type of care? Who should be paying for their care?
Consider this: What is fair, and who decides? Why are some patients labeled very important persons (VIPs)? Should they receive a different level of care? Why or why not? What kind of access to health care should illegal immigrants receive: preventive or more costly ED care?
Veracity: the duty to tell the truth
The principle of veracity may become an issue when a patient who suspects that her diagnosis is cancer asks you, “Nurse, do I have cancer?” Her family has requested that she not be told the truth, because their culture believes bad news takes away all hope for the patient.
Consider this: Is lying to a patient ever justified? If a patient finds out that you have lied, will that patient have any reason to trust you again?
Each of the aforementioned principles sounds so right; yet the “consider this” questions indicate that putting principles into practice is sometimes much easier said than done. Reality does not always offer textbook situations that allow flawless application of ethical principles. As Oscar Wilde, an Irish playwright, once said, “The truth is rarely pure, and never simple.” You will encounter clinical situations that challenge the way you apply an ethical principle or that cause two or more principles to be in conflict, creating moral distress, which is often referred to as an ethical dilemma.
Which Principle or Rule Is Most Important?
Current thinking on the part of ethicists favors autonomy and nonmaleficence as preeminent principles, because they emphasize respect for the person and the avoidance of harm. However, there is no universal agreement, and many individuals rely on their spiritual beliefs as the cornerstone to ethical decision making.
Another possible approach to decision making is to consider the relative benefits and burdens of an ethical decision for the patient. If patients are capable of rational decision making, they may choose a different treatment approach than the care team. This fact is sometimes difficult for health care team members to accept, especially if it involves a decision to stop treatment. If patients are not capable of autonomous decision making, substituted judgment (decision making) by their designated family is then used. Problems frequently arise when family members disagree on a treatment choice or quality-of-life issues, as evidenced by the Terry Schiavo case in Florida (2003), when the husband’s wishes to discontinue life support for his wife were granted after a prolonged court case that included attempted government intervention.
Traditional and contemporary models of ethical reasoning offer worldviews from which ethical principles, spiritual values, and the concepts of benefits and burdens can be derived, interpreted, and comparatively emphasized. Nevertheless, models of ethical reasoning are not without their critics, including nurses, who feel that abstract ideas about right and wrong are not helpful or “practical” at the bedside.
In recent years, nursing ethicists have advanced a new approach to ethical issues, emphasizing an ethic of caring as the moral foundation for nursing. Nurses have been encouraged to consider all ethical issues from the central issue of caring. Because caring implies concern for preserving humanity and dignity and promoting well-being, the awareness of rules and principles alone does not adequately address the ethical issues that nurses confront, such as in cases of suffering or powerlessness. Research regarding the application of caring to ethical issues is under way, but a practical model for applying this ethic of caring to clinical situations does not yet exist. Currently, the most care-centered approach to ethical dilemmas is to consider the relative “benefits versus burdens” that any proposed solution offers to the patient. Health team members need to try to consider benefits and burdens from the patient’s perspective versus their own values on life, death, and the vast degrees of illness between the two. It is a difficult task to undertake.
So How Do I Make an Ethical Decision?
A number of approaches to ethical decision making are possible. The following is a brief overview of the three most commonly applied models of ethical reasoning. The first two types are considered normative because they have clearly defined parameters, or norms, to influence decision making. The third type is a combination of the other two models.
Deontological
Derived from Judeo-Christian origins, the deontological normative approach is duty-focused and centered on rules from which all action is derived. The rules represent beliefs about intrinsic good that are moral absolutes revealed by God. This approach reasons that all persons are worthy of respect and thus should be treated the same.
As a result of the rules and duties that the deontological approach outlines, the individual may feel that he or she has clear direction about how to act in all situations. Right or wrong is determined based on one’s duty or obligation to act, not on the consequences of one’s actions. Therefore abortion and euthanasia are never acceptable actions, because they violate the duty to respect the sanctity of all life, and lying is never acceptable because it violates the duty to tell the truth. The emphasis on absolute rules with this approach is sometimes seen as rigid and inflexible, but its strength is in its unbending approach to many issues, emphasizing the intent of actions.
Teleological
Derived from humanistic origins, the teleological approach is outcome-focused and places emphasis on results. Good is defined in utilitarian terms: That which is useful is good. Human reason is the basis for authority in all situations, not absolutes from God. Morality is established by majority rule, and the results of actions determine the rules. Because results become the intrinsic good, the individual’s actions are always based on the probable outcome.
Simplistically, this view is sometimes interpreted as “the end justifies the means.” Abortion may be acceptable, because it results in fewer unwanted babies. Euthanasia is an acceptable choice by some patients, because it results in decreased suffering. Giving preference for a heart transplant to a foreign national who can pay cash and donate money for a transplant program is acceptable, because this will create a greater good for others. Using this approach, the rights of some individuals may be sacrificed for the majority.
Situational
Derived from humanistic and Judeo-Christian influences and most commonly credited to Joseph Fletcher (1966), an Episcopalian theologian, the situational view holds that there are no prescribed rules, norms, or majority-focused results that must be followed. Each situation creates its own set of rules and principles that should be considered in that particular set of circumstances. Emphasizing the uniqueness of the situation and respect for the person in that situation, Fletcher appeals to love as the only norm. Critics of this approach argue that this can lead to a “slippery slope” of moral decline.
Chemically restraining a disruptive patient who has Alzheimer’s disease provides a calmer atmosphere for other patients in a long-term care facility. This approach is used after all other efforts to calm the patient have failed. “Pulling the plug” on a terminally ill patient who does not want any more extraordinary care can be considered an act of compassion. Withholding or withdrawing treatment is ethically correct from the individual patient’s perspective if the burden of treatment outweighs the benefit of merely extending life. Defining burden has to be approached from the patient’s perspective, not from others who may feel burdened by the patient’s need for care. Viewing a situation from the perspective of benefit versus burden can assist patients and families to make difficult decisions on the basis of the patient’s clear or intended wishes discussed over a period of time. Nurses and other health care providers need to be patient advocates, speaking out for those who are disadvantaged and cannot speak for themselves.
Table 19.1 compares the relative advantages and disadvantages of each approach. Remember that there is no perfect worldview. If there were, debate would stop, and the need for continued ethical deliberation would cease. The ethical models presented here are not intended to be all-inclusive or exhaustive in depth. Rather, they should whet your appetite for further content. Many journals and texts are devoted to clinical ethics, and you are encouraged to see how ethicists apply these and other models to issues that affect your area of practice. Surveys of nurses indicate an ongoing interest and an expressed need for ethical discussion and support in practice. Nurses experience ethical distress along with other health care team members, but the 24/7 experience of nursing is unique from the perspective of patient continuity and opportunities for advocacy. Nurses increasingly serve on hospital ethics committees and are encouraged to contribute their perspectives to ethical debates.
TABLE 19.1
Three Approaches to Ethical Decision Making: Comparison of Advantages and Disadvantages
| Ethical Approach | Advantages | Disadvantages |
| Deontological | Clear direction for action. | Perceived as rigid. |
| All individuals are treated the same. Does not consider possible negative consequences of action. | Does not consider possible negative consequences of actions. | |
| Teleological | Interest of the majority is protected. | Rights of individual may be overlooked or denied. |
| Results are evaluated for their good, and actions may be modified. | What is a good result? Who determines good? Morality may be arbitrary. | |
| Situational | This approach mirrors the way most individuals actually approach day-to-day decision making. | What is good? Who decides? Morality is possibly arbitrary. |
| Merits of each situation are considered. Individual has more control/autonomy to make decisions in his or her own best interest. | Lack of rules of generalizability limits criticism of possible abuse. |
How Do I Determine Who Owns the Problem?
The decision to choose a particular model of ethical reasoning is personal (see Table 19.1) and is based on your own values. Familiarize yourself with various models to decrease your own moral uncertainty and gain some understanding of the values of others. The following guidelines are suggested as a means of analyzing ethical issues that will confront you in nursing practice. You will not be a pivotal decision maker in all situations, but these guidelines can assist you in making up your own mind and helping patients to voice their wishes and ask questions.
First, determine the facts of the situation
Make sure you collect enough data to give yourself an accurate picture of the issue at hand. When the facts of a situation become known, you may or may not be dealing with an ethical issue.
For example, as an ICU nurse, you believe that the wishes of patients regarding extraordinary care are being disregarded. In other words, resuscitation is performed despite expressed patient wishes to the contrary. You need to
▪ Determine whether discussion about extraordinary care is taking place among patients, their families, and health care providers.
▪ Clarify the institution’s policy regarding cardiopulmonary resuscitation (CPR) and do-not-resuscitate (DNR) orders.
▪ Determine what input the families have had in the decisions—that is, whether the families are aware of the patient’s wishes.
▪ Explore the use of advance directive documentation at your institution, and determine whether patients are familiar with the use and possible limitations of living wills.
▪ Share your concerns with health care providers to obtain their views of the situation. Discuss the situation with your clinical manager to clarify any misconceptions regarding policy and actual practice.
Second, identify the ethical issues of the situation
In the ICU scenario, if competent patients have expressed their wishes about resuscitation, this should be reflected in the chart. If a living will has been executed and is recognized as valid within your state, its presence in the chart lends considerable weight to the decision. The patient should be encouraged to discuss his or her decision with family to decrease the chances for disagreement if and when the patient can no longer “speak” for himself or herself. If immediate family members disagree with the living will, the physician may be reluctant to honor it, at least in part because of concern regarding possible liability. If a living will is executed without prior or subsequent discussion with the attending physician, there may be reluctance to honor the will, because the physician was not informed of the patient’s decision. The physician may feel that the patient did not make an informed decision. However, a durable power of attorney for health care (DPAHC), combined with a living will completed before the patient’s present state of incapacitation, would stand as clear and convincing evidence of the patient’s wishes, preventing such a problem. The example of extraordinary care in the ICU illustrates the existence of values and principles in conflict. When the care team, family, and patient have different views of the situation, the patient is likely to be burdened with less than the best outcome, unless differences are resolved. The nurse can facilitate communication between the family and patient in resolving differences among all those involved. In this situation, the ethical components of this second step involve autonomy and fidelity versus beneficence.
Third, consider possible courses of action and their related outcomes
Having collected data and after having attempted to discuss the issue with all involved parties, you are faced with the following three options:
1. Advocate for the patient with physicians and the family by facilitating communication.
2. Encourage the patient and family to share feelings with each other regarding desires for care.
3. Encourage the family, patient, and attending physicians to discuss the situation more openly.
If the advocacy role does not bring about some change in behavior, consider the possible input and assistance of an interdisciplinary ethics committee (IEC). In the past two decades, such committees have evolved in response to the growing number of ethical issues faced in clinical practice. Most hospitals now have an IEC, which is typically composed of physicians, clergy, social workers, lawyers, and, increasingly, nurses. Any health team member can access the committee with the assurance at least of receiving a helpful, listening ear. If necessary, the committee will convene to review a clinical case and will offer an unbiased opinion of the situation. Committee members may be helpful in clarifying issues or offering moral support; they may also be persuasive in suggesting that involved parties (i.e., family, physician, patient, and nurse) consider a suggested course of action. The authority of an IEC is usually limited, because the majority of IECs are developed with the understanding that the advice and opinions offered are not binding to the individual. However, an IEC can serve as a potent form of moral authority and influence if used.
Taking the initiative to express your values and principles is not necessarily easy. As a recent graduate, it may seem safer to “swallow hard,” remain quiet, and invest your energies in other aspects of your role. You may risk ridicule, criticism, and disagreement when you speak out or have questions on an ethical issue, especially if your view is different or unpopular. However, you risk something far more important if you do not speak out and ask questions for clarification. Silence diminishes your own autonomy as a person and as a professional. Depending on the situation, you may raise eyebrows, but it is important to make your concerns known, because some values may be imposed on the patient or on you in the clinical setting, and those values may not be morally correct. You may not agree with the values or believe that they are in the best interest of the patient. Unresolved moral distress is also cited as a cause for job resignation (Pendy, 2007). Find your voice, ask questions, and speak up so you can control your practice more effectively.
Fourth, after a course of action has been taken, evaluate the outcome
In the ICU scenario, did improved communication occur among patients, families, and physicians? Were your efforts to advocate met with resistance or a rebuff? What could you try differently the next time? What values or principles were considered most important by the decision makers? What kind of assistance did you receive from the IEC? What role did nursing play in this situation, and was it appropriate?
What Other Resources Are Available to Help Resolve Ethical Dilemmas?
Nurses have several resources to assist them in resolving ethical issues that may occur in professional settings. Nurses must first consider their personal views on the issue and consider having an open and honest discussion with their peers and supervisors. After reflection and discussion, nurses may consider consulting the institution’s ethics committee if the issue remains unresolved. Many professional resources are also available to provide direction about ethical issues and behavior. The first of these is the American Nurses Association (ANA) Code of Ethics for Nurses (2015, p. 196). The code is a statement to society that outlines the values, concerns, and goals of the profession. It should be compatible with the individual nurse’s personal values and goals. The code provides direction for ethical decisions and behavior by repeatedly emphasizing the obligations and responsibilities that the nurse–patient relationship entails.
The provisions of the Code of Ethics for Nurses allude to the ethical principles mentioned earlier in this chapter and certainly imply that fidelity to the patient is foremost. A copy of the code with interpretive statements is available from the ANA. If you did not purchase a copy as a reference for school, consider buying it for your own use in practice. A copy of the code should be accessible within your place of employment.
Critics of the Code of Ethics for Nurses cite its lack of legal enforceability. This is a valid criticism, because the code is not a legal document as licensure laws are. However, the code is a moral statement of accountability that can add weight to decisions involving legal censure. Many practicing nurses claim ignorance of the Code of Ethics for Nurses or believe that it is a document for students only. However, the Code of Ethics is for all nurses and was developed by nurses. In 2001, the American Nurses Association published a Bill of Rights for Registered Nurses, a first ever document of “rights” in contrast to the traditional focus on responsibilities. Awareness of these rights may provide nurses with a sense of comfort in voicing their advocacy for patients as well as for themselves. Take the opportunity to become familiar with its contents (ANA, 2001). Box 19.2 presents the International Council of Nurses Code for Nurses. The international code is valuable because it points out issues of universal importance to all nurses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree