Epidemiology
Unraveling the Mysteries of Disease and Health
Gina C. Rowe
Focus Questions
What statistical measures are used in epidemiology?
How are data used in determining the health status of a community?
How is epidemiological information used to frame or focus health-related research?
Key Terms
Analytic studies
Case-control
Cohort
Correlation
Descriptive studies
Epidemics
Epidemiology
Experimental trial
Health information systems
Incidence
Morbidity
Mortality
Pandemics
Prevalence
Primary prevention
Rate
Ratio
Records
Secondary prevention
Surveillance
Surveys
Tertiary prevention
Vital statistics
“Too Much Heart Surgery?” “Where Do We Stand in the Fight against Cancer?” “What Doctors Don’t Know about Women: NIH Tries to Close the Gender Gap in Research.” “Baby Boomers Enter Their Fifties.” “Decline of Birth Rate in United States.” “Evaluation of Health: Haves and Have Nots.” “Increasing Global Burden of AIDS.”
What is the source of the information that produces these headlines? Who collects it? How is the information used in nursing and health care? Understanding health problems, conditions related to health, and ways to improve the well-being of a population requires a systematic approach to gathering factual information. This chapter does the following:
• Presents an overview of basic formulas and methods of epidemiological investigation
• Identifies the most important health issues for all age groups in the United States
The last objective is a critical first step in assessing the health needs of populations, aggregates, and target groups.
Epidemiology is the discipline that provides the structure for systematically studying the distribution and determinants of health, disease, and conditions related to health status. Epidemiological concepts are used to understand and explain how and why health and illness occur as they do in human populations. Nursing and medical science employ these concepts to help guide clinical practice and influence health outcomes. For example, the Healthy Babies Program, which includes home visiting by a nurse during an infant’s first year, was established to decrease infant mortality and promote health.
Florence Nightingale, the first nurse epidemiologist, pioneered the use of statistics to improve public health. During the Crimean War, Nightingale collected data and systemized record-keeping practices to improve hospital conditions. She invented pie charts and other graphical illustrations to depict mortality rates and show how improvements in sanitary conditions would lead to a decrease in deaths. By focusing on health and disease trends among populations, Nightingale saved or improved the lives of countless individuals, the ultimate goal of epidemiology.
Interests of population-based data
In community health nursing, the community or the total population under investigation replaces the individual as the focus of concern and study. Nursing at the community level extends the boundaries of practice beyond those that are traditionally associated with caregiving activities. The thinking and decision making that a community health nurse uses to define the health status of a community are markedly different from those used in assessing individual clients or families. Applying the nursing process to the entire community is complex and generally requires educational preparation at the graduate level.
The concepts and methods employed in assessing health status that affect program planning in health care, as well as analysis and applications of epidemiological data, form the basis of this chapter. An in-depth understanding of statistics is not required to understand epidemiology. Computation of the simple formulas used in this chapter requires only basic mathematical skills: addition, subtraction, multiplication, and division.
A Few Statistics
Rate, ratio, incidence, and prevalence are common terms used to help describe illness and disease among population groups.
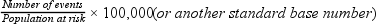
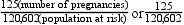
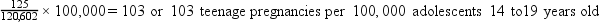
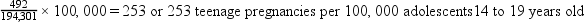
Rates and Ratios
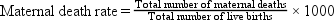
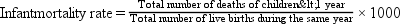
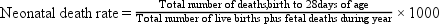
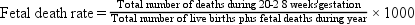
A rate is a statistic used to describe an event or characteristic. In epidemiology a rate is used to make comparisons among populations or to compare a subgroup of the population (specific rate) with the total population. The numerator of a rate is the actual number of events, and the denominator is the total population at risk. In epidemiology the rate is usually converted to a standard base denominator—such as 1000, 10,000, or 100,000—to permit comparisons between various population groups (Box 7-1). A rate description includes time, person or population, and place specifications (e.g., the number per year [time] in uninsured children [population] in a specific city [place]).
Using standard base rates makes comparing the magnitude of an event (e.g., illness, death) in different population groups easier. For example, if city A had 125 teenage pregnancies in an at-risk population group of 120,602 female teenagers (14 to 19 years old), the rate of teenage pregnancies in city A could be expressed as 125 per 120,602. If city B had 492 teenage pregnancies in an at-risk population of 194,301 female teenagers, the rate of teenage pregnancies in city B would be 492 per 194,301 (see Box 7-1). Comparison of these two rates is difficult because no common reference point exists. However, if the denominators of these two rates were converted to a common at-risk population of 100,000, city A’s rate would be 103 per 100,000, and city B’s rate would be 253 per 100,000. Common base rates permit accurate comparisons and are much easier to understand.
Health statistics are sometimes reported as a ratio, which is simply the comparison of one number with another. A ratio is often used to compare one at-risk population with another. Ratios are usually simplified by reducing the numbers so that the smallest number becomes 1. To use the example of cities A and B, the ratio of teenage pregnancies in city A to those in city B would be 103 (city A) to 253 (city B), or 103:253, which can be reduced to approximately 1:2.5; in other words, city B has approximately 2.5 times as many teenage pregnancies per 100,000 female teenagers aged 14 to 19 years as does city A.
Suppose you were told that more homicides occurred in Los Angeles than in Washington, DC. How would you compare the rates, rather than just the numbers? Would you need to know the total population at risk for each city? In 2010 there were 293 homicides in Los Angeles, a city of 3,841,707 people, and 132 in Washington, DC, a city of 601,723 people. The murder rate for Los Angeles was 7.63 per 100,000 people compared with 21.94 per 100,000 people in Washington, DC (Federal Bureau of Investigation, 2011a, 2011b). The murder rate for Washington, DC was almost three times higher than that for Los Angeles.
Measures of Morbidity and Mortality
Statistics on mortality (death rates) and morbidity (illness rates) are collected routinely and used to describe the frequency of death or disease for a given time, place, and group of persons. Morbidity statistics also include measures related to specific symptoms of a disease, days lost from work, and number of clinic visits. In the United States, the law requires that death records be kept; they are tabulated by the National Center for Health Statistics and help determine trends in the United States.
Incidence and Prevalence Rates
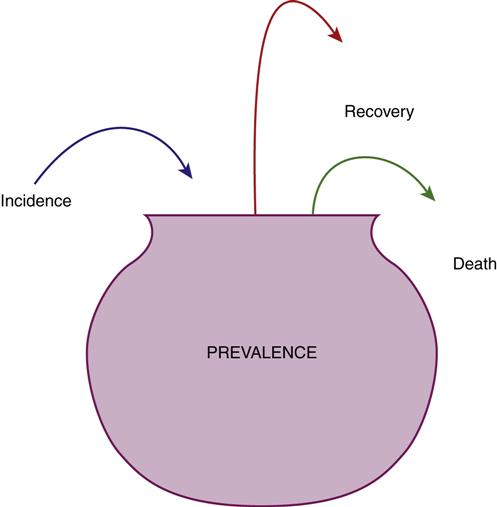
Incidence refers to the rate at which a specific disease develops in a population. The incidence rate is the number of new cases of an illness or injury that occurs within a specified time. In contrast, prevalence measures all of the existing cases at a given point in time. Prevalence includes the new cases (incidence) plus all of the existing cases. The prevalence rate is influenced by how many people become ill and how many people recover or die (Figure 7-1).
Prevalence is important in determining measures of chronic illness in a population and is affected by factors that influence the duration of the disease. Thus prevalence rates have relevance for planning for health care services, resources, and facilities; for determining health care personnel needs; and for evaluating treatments that prolong life.
Conversely, incidence rates are used as tools for studying patterns of both acute and chronic illness. Incidence rates are important because they are a direct measure of the magnitude of new illness in a population and provide assessments about the risk associated with particular illnesses. For example, the incidence of certain childhood illnesses, such as measles, polio, and whooping cough, was drastically reduced in the United States during the twentieth century with the introduction of vaccines effective in preventing these diseases. Because they reflect only the development of a disease, incidence rates may be influenced by preventive health measures but typically remain unchanged by new medical treatment patterns. New drugs to treat type 2 diabetes mellitus can help to control blood glucose levels and prevent serious disease complications, such as heart attack, blindness, and limb amputation, but they will not affect diabetes incidence; only health promotion and disease prevention efforts targeting behavioral change in diet and exercise patterns have the potential to decrease incidence of this chronic disease.
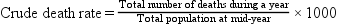
Crude, Adjusted, and Specific Rates
A rate can be expressed for the total population (crude or adjusted rate) or for a subgroup of the population (specific rate). Box 7-2 presents the formulas for frequently used mortality rates. Age-specific and age-adjusted rates are often quite helpful in making comparisons among populations.
Types of epidemiological investigation
People who are engaged in epidemiological research frequently observe rather than manipulate variables believed to influence the health of the human population. An observational methodology means that the researcher has far less control of the factors under study and that extraneous factors may not be well controlled for in the study design. Epidemiological studies, however, do identify nonrandom patterns of health and disease and serve as the basis for determining the circumstances in which experimental studies would be beneficial. They also are of value in planning and evaluating health care services. Epidemiological studies can be divided into three major types: descriptive, analytic, and experimental.
Descriptive Studies
Descriptive studies, including prevalence and correlation studies, customarily describe the amount and distribution of disease within a population. This approach relies primarily on collection of existing data and answers the following questions:
• Where is the disease distributed in the human population (place)?
• When is the disease present (time)?
The National Health Interview Survey, sponsored by the U.S. Department of Health and Human Services (USDHHS), is administered to a random sample of individuals in the United States. Descriptive information from this survey provides demographic and health information for the nation. The results of this survey are available to the public, and researchers who are seeking to test their own hypotheses can conduct secondary analyses of this descriptive data set.
An example of a prevalence study is “Vitamin D Deficiency and Seasonal Variation in an Adult South Florida Population” (Levis et al., 2005). At winter’s end, the researchers found deficient levels of vitamin D in 38% of men and 40% of women in the study. These prevalence rates were higher than expected in a southern region, which indicated that health care providers in Florida should still consider vitamin D deficiency as a possible factor when assessing patients for osteoporosis.
An example of a correlational design is a study conducted by Burnett-Zeigler and associates (2011) exploring prevalence and correlates of alcohol misuse among Army National Guard service members recently returned to Michigan from Afghanistan and Iraq. Results indicated that the rate of alcohol misuse was high (36%) and associated with male gender, younger age, and reported symptoms of depression or posttraumatic stress disorder. Major barriers to accessing mental health services cited by those who met misuse criteria were related to perceived stigma. In contrast, concern by a spouse, physician, peer, friend, or family member was most commonly cited as positively influencing pursuit of mental health care. Thus, the study identified associations, or correlations, between alcohol misuse and possible contributing factors, and proposed early outreach and social support as potential interventions to improve mental health care linkages. Descriptive studies may employ cross-sectional timing in their design, in which information on risk factors or exposures and information on outcomes or diseases is all gathered at the same time. Because data are gathered at only one point in time, it can be difficult to determine which actually occurred first, suspected risk factors or disease. Does alcohol misuse contribute to developing depression, or do depressed people tend to misuse alcohol more often? Associations between variables may be noted in descriptive studies, but these are not necessarily due to cause-and-effect relationships.
Analytic Studies
Like descriptive studies, analytic studies use observational methodology, but in contrast to simple descriptive designs, analytic studies begin to answer questions about cause-and-effect relationships between a potential risk factor and a specific health phenomenon or disease condition. Hypotheses, which are statements of possible relationships, are used to predict the causal association among the variables. Being able to predict risk thus points to factors that, if changed, may prevent the disease from occurring or reduce its risk. The hypotheses are tested through studies using cohort or case-control designs, and these studies may be retrospective or prospective.
Cohort studies are useful in identifying factors associated with increased risk of developing certain diseases. The Framingham Heart Study is a classic example of a prospective cohort study, which follows originally healthy people over time to observe risk factors and the development of disease. The study was begun in 1948 with funds from the National Heart Institute in Framingham, Massachusetts, to identify factors contributing to cardiovascular disease. It is still going on today in collaboration with Boston University and now includes data on three generations—the original study subjects, the offspring of the original cohort, and the generation III cohort (National Heart, Lung, and Blood Institute, 2011). Landmark findings from the Framingham Heart Study have provided information about obesity and elevated lipid levels as risk factors for atherosclerotic disease and about tobacco use, sedentary lifestyles, hypertension, and diabetes as risk factors for cardiovascular disease.
Other examples of cohort studies are the Nurses’ Health Studies (NHS) I and II, initiated by Dr. Frank Speizer in 1976 and expanded by Dr. Walter Willett and colleagues in 1989 with funds from the National Institutes of Health. The primary goal of NHS II was to gather long-term information about oral contraceptive use, diet, and lifestyle risk factors in women younger than the original NHS cohort. Over 81,000 nurses between 25 and 42 years of age were recruited and answered surveys about health and lifestyle every 2 to 4 years over 26 years (Chiuve et al., 2011). Chiuve and colleagues found that adherence to a low-risk lifestyle (i.e., regular exercise, not smoking, following a Mediterranean-style diet, and maintaining a normal body mass index) was associated with a 92% lower risk of sudden cardiac death in this population. A new, more diverse cohort of nurses has now been recruited for NHS III, which will be conducted online and examine effects of hormones, diet, and occupation on women’s health and fertility; the principal investigator is Susan E. Hankinson, RN, ScD.
Case-control studies are retrospective because the study begins after the health outcome has already occurred. Researchers select a group of case subjects with a known disease or health outcome and compare them to a group of control subjects who do not have the disease or health outcome. King and associates (2005) used a case-control design to investigate potential relationships between stillbirths in Nova Scotia and Eastern Ontario, Canada, and chlorine disinfection by-products found in public drinking water sources. They found that stillbirth cases were more likely than live birth controls to have been exposed to some types of these drinking water disinfection by-products (trihalomethanes) but not to others (haloacetic acids). Case-control studies are advantageous in assessing multiple exposures or risk factors for diseases or health outcomes that occur infrequently, because they can be done with smaller sample sizes than those needed to study rare or infrequent health outcomes in cohort studies.
Experimental Trials
If the evidence suggests that some relationships are appropriate for further study to confirm cause and effect, an experimental study, usually known as a clinical or experimental trial, may be conducted. Experimental trials always begin with carefully designed questions, hypotheses, and research protocols that specify the criteria for selection of the people (subjects) to be studied, the methods for random assignment of subjects to the experimental and control groups, the treatment procedure, the follow-up of subjects, and the details of the data analyses. In experimental studies, the researcher always manipulates variables, such as a nursing intervention or a health-teaching approach, in the experimental and control groups. An example of an experimental epidemiological study is the Physicians’ Health Study. In this randomized, placebo-controlled study, 22,071 male physicians aged 40 to 84 years were randomly assigned to one of four treatment groups to study the effects of aspirin and beta-carotene use on cardiovascular disease (Physicians’ Health Study, 2011). The study found that low-dose aspirin use (325 mg every other day) reduced the risk of cardiovascular mortality by 44% (Steering Committee of the Physicians’ Health Study Research Group, 1989), but long-term beta-carotene supplementation had no effect on the incidence of cancer or cardiovascular disease (Hennekens et al., 1996). Because of ethical concerns about not causing suffering or exacerbation of illness, experimental studies usually involve the testing of hypotheses related to disease prevention, health promotion, or, in some situations, the treatment of a specific disease.
Because community health nurses are asked to plan, implement, and evaluate health care services for specific populations, understanding epidemiological concepts and principles is important. For example, epidemiological investigations can evaluate the extent to which a program that is provided by nurses and designed to increase access to early prenatal care is successful in reducing prematurity and low birth weight. Epidemiological methods may also be used to evaluate the effectiveness of primary intervention strategies and thus improve nursing practices. The trend toward outcomes research and evidence-based practice is reflected in studies using these types of methods.
Understanding aggregate-level data
A primary focus of community health nursing is the definition of health-related problems (assessment) and the posing of solutions (interventions) for populations or aggregates of people. Population-level decision making requires a different understanding from that used in direct caregiving to individuals. The questions for analysis are different. At the population level, pertinent questions might be the following:
• Which subgroups have the highest incidences of diabetes?
• Who is at high risk for developing diabetes?
• What programs are available for diabetes prevention and early detection?
Given the focus of community health on the well-being of the community, emphasis is necessarily placed on what makes a healthy community. This includes the interrelationship between the health status of the population and the potential for healthy actions within the population, factors that influence health status, and the ability of the health care system to allocate appropriate resources and respond effectively to the needs of the population. The projected trend for health care reform and the increased prevalence of managed care delivery systems call for nurses to assume more responsibility for clients in the community. Therefore, the need for nurses to understand and practice nursing at the population level is more urgent.
In an attempt to respond effectively to these health care challenges, the USDHHS published a report establishing national health objectives for each decade. Healthy People 2020 is the current report outlining national objectives for health promotion and disease prevention (see the Healthy People 2020 box below and the discussion in Chapter 2). This report identifies the goals and priorities toward which health care planners and providers should work to improve the health of the U.S. population. Although the goals are directed toward healthier lives for all Americans, particular emphasis is given to special cohorts. A cohort is a group of people who share similar characteristics. For example, people born in the same decade represent an age cohort. Healthy People 2020 targets certain cohort groups: newborn babies, boys and girls, adolescents and young people, women and children, and people in their later years (USDHHS, 2010).
Concepts related to prevention, health promotion, and disease
Three major concepts are crucial to understanding epidemiology: the natural history of disease, the levels of prevention, and the multiple causation of disease. These concepts are an important foundation to help in planning appropriate nursing interventions for cohorts, aggregates, and populations.
Natural History of Disease
Diseases evolve over time. Leavell and Clark (1965), in their classic description of the disease process, delineate two distinct periods: prepathogenesis and pathogenesis. The prepathogenesis period encompasses the stages of susceptibility and adaptation. During the stage of susceptibility, interactions occur among the person, the environment, and the causative agent that increase the potential for disease. This period leads to the stage of adaptation, in which changes in the body occur in response to some agent or stimulus, but these physiological or immune system reactions are still part of a normal adaptive response. Although factors are present that increase risk during the period of prepathogenesis, no disease exists. For example, obesity in combination with a sedentary lifestyle and smoking increases a person’s chances for developing coronary heart disease. Because some risk factors can be altered, understanding the natural history of a disease is important. Awareness of the presence of risk allows the nurse to initiate preventive measures against the disease or limit its development.
For diseases in which detection through symptoms occurs late in the disease trajectory, early detection may be possible by technological screening procedures. In the case of breast cancer, for example, mammography can detect the disease before symptoms emerge. Many diseases, such as acute or infectious diseases, run their course, and a person experiences complete recovery. Changes resulting from chronic diseases or conditions, however, may have long-term effects. Symptoms generally become more fixed and are less reversible as the disease continues. With advancing disease, functional changes may produce marked disability and lead to death.
Analyzing the natural history of a disease involves the use of the epidemiological triangle (Figure 7-2). A change in any of the factors represented in this triangle (the person, the causative agent, or the environment) has the potential to change the balance of health. For the person or host, demographic characteristics, the level of health and history of prior disease, genetic predisposition, states of immunity, body defenses, and human behavior should be examined (Box 7-3). Causative agents may include biological, physical, chemical, nutritional, genetic, or psychological factors that have the ability to affect health and disease in the person. The environment includes anything external to the person or agent, including the presence of other persons or animals that potentially affect health and disease.

Investigation by public health officials did not identify a single event, food handler, or contaminated water supply as a source for this outbreak. However, most case clients ate lunch in schools, and further analysis revealed a strong association between illness and consumption of food items containing frozen strawberries.
The strawberries linked to this outbreak were grown in Mexico and shipped to a southern California company, where they were processed, packed, and frozen in 30-lb containers to be distributed to U.S. Department of Agriculture–sponsored school lunch programs. Whether the strawberries were contaminated in Mexico or in the processing company in California was uncertain. Further investigations continued to track the source of the contamination. Meanwhile, the Centers for Disease Control and Prevention (CDC) notified the health departments in six other states to which strawberries from the same lots as those sent to Calhoun County had been shipped. Immunoglobulin postexposure prophylaxis was offered to persons who consumed frozen strawberries from the suspected lots through school lunch programs, but only when it could be initiated within 14 days of their exposure.
Can you think of some ways that the epidemiological concepts of host, agent, and environment relate to this clinical example?
Multiple Causation of Disease
The theory of multiple causation of disease is critical to understanding epidemiological problems. Causality is generally considered in terms of a stimulus or catalyst that produces a single effect, result, or outcome. In epidemiology the interactions of the agent, person (host), and environment are analyzed by statistical methods to determine whether a causal relationship exists between various factors and health status. Understanding these interactions and relationships is even more important and complex as one considers the natural history of noninfectious diseases, chronic conditions, and the health and well-being of a population. In these instances, multiple causes or factors are usually interacting to affect health status.
A significant number of multiple causation models in epidemiology can be found. The model of Dever (1991) recognizes input from human biology, lifestyle, environment, and the health care system in the development of a particular health condition. The Web of Causation model is a metaphoric model that has been used in epidemiology texts since the early 1960s to describe the multifactorial causes of disease (Krieger, 1994).
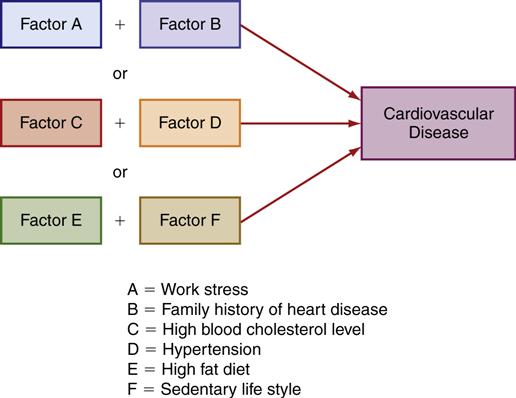
All the models point to the interplay of numerous factors in the presentation of a specific disease. Figure 7-3 illustrates factors associated with heart disease. Some of these factors are easily amenable to change, whereas others are not. One way to remember the categories of causes for disease is the acronym used in the BEINGS model of disease causes. These categories include the following:
Obviously, the factors in some of these categories are harder to change than others. For example, genetic factors remain the most difficult to manipulate, whereas nutritional factors are more easily changed.
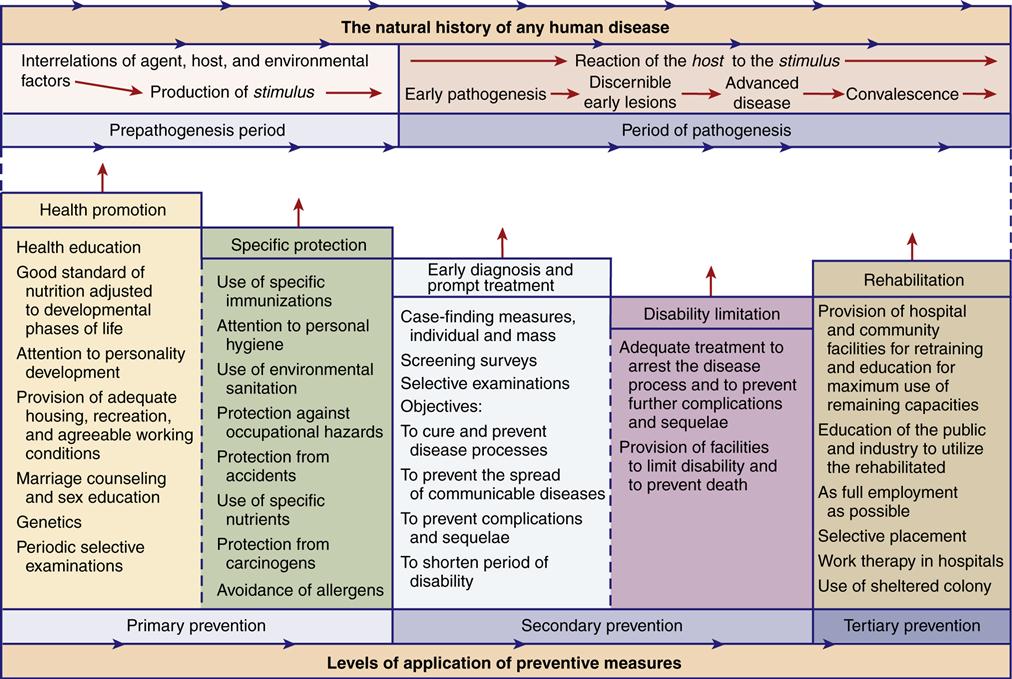
Levels of Prevention
Because disease occurs over time, there are many potential points at which intervention may prevent, halt, or reverse the pathological change. A three-level model developed by Leavell and Clark (1965) based on the idea that disease evolves over time continues to be used in the conceptualization and structure of health programs (Figure 7-4).
Primary Prevention
Primary prevention is aimed at altering the susceptibility or reducing the exposure of persons who are at risk for developing a specific disease. Primary prevention includes general health promotion and specific protective measures in the prepathogenesis stage, which are designed to improve the health and well-being of the population. Nursing activities include health teaching and counseling to promote healthy living and lifestyles. Specific protective measures aimed at preventing certain risk conditions or diseases—such as immunizations, the removal of harmful environmental substances, protection from ultraviolet rays, or the proper use of car safety seats for infants and children—are also primary prevention activities. Recent advances in genetic screening have initiated a debate over its role in disease or disability prevention. Although genetic scientists hail research advances as one step on the road to ridding the world of disease and disability, others view that step more as a slippery slope. Is a child with less potential for disease or disability a more perfect child? If we have the technology to produce such a child (by selective abortion or gene manipulation), does the public have the right of access to this technology? What message does this send to the disabled community? From a community perspective, what other dilemmas can you imagine surfacing in relation to genetic screening?
Secondary Prevention
Secondary prevention is aimed at early detection and prompt treatment either to cure a disease as early as possible or to slow its progression, thereby preventing disability or complications. Screening programs in which asymptomatic persons are tested to detect early stages of a disease are the most frequent form of secondary prevention. Early case finding and prompt treatment activities are directed toward preventing the transmission of communicable diseases, such as the spread of impetigo in a school. Preventing or slowing the development of a particular disease or condition and preventing complications from a disease, such as scoliosis in teenage girls, are also examples of secondary prevention.
Tertiary Prevention
Tertiary prevention is aimed at limiting existing disability in persons in the early stages of disease and at providing rehabilitation for persons who have experienced a loss of function resulting from a disease process or injury. Nursing activities include education to prevent deterioration of a person’s condition, direct nursing care, and referrals to resources that can help clients minimize the loss of function.
Health information systems
Health information is the data collected about the significant health-related events that occur over a period within a population. Health information systems are data collection systems for gathering health statistics and other health-related information at the population level and may include collection of vital statistics, surveillance, surveys, and records.
Data used in epidemiology are systematically collected by government agencies and private groups to measure the size and scope of health problems and factors contributing to them; to study trends and predict the future course of health problems; to identify subgroups to target for interventions; and to evaluate the outcomes of intervention programs and their costs.
Types of health information collected include vital statistics and health statistics on morbidity and disability, health behaviors, nutrition, and health care access, utilization, and costs. Data on personal, behavioral, environmental, and occupational risk factors associated with illness are collected and analyzed, and sometimes information on related political and economic issues that affect health is also collected.
Much epidemiological information is now available on the Internet, for example, the home pages of the U.S. Census Bureau and the CDC. These two websites also contain many helpful links to other websites. (See the resource list at the end of the chapter for additional information.)
Vital Statistics
A major source of information about a population comes from the vital statistics that are recorded about them. Vital statistics is the term used for the data collected from the ongoing registration of vital events, such as death certificates, birth certificates, and marriage certificates. These data are systematically collected by agencies such as the National Center for Health Statistics and the World Health Organization (WHO). Many other governmental agencies within the CDC and the USDHHS, as well as private groups such as the Children’s Defense Fund, also make use of these statistics and issue reports related to particular health concerns. One example of such a publication is the Morbidity and Mortality Weekly Report (MMWR) published by the CDC.
Surveillance
Surveillance is the ongoing systematic collection, analysis, and dissemination of health information for the purpose of monitoring and containing specific, primarily contagious, diseases. An example of a surveillance and response system is the WHO’s Global Outbreak Alert and Response Network, a group of collaborating institutions formed to rapidly identify, confirm, and respond to internationally important disease outbreaks, such as avian influenza (WHO, 2011). The National Notifiable Diseases Surveillance System in the United States is operated by the CDC and the Council of State and Territorial Epidemiologists to provide weekly reports (MMWR) and annual reports (Summary of Notifiable Diseases, United States) on the occurrence of notifiable diseases, a list of which is provided in Chapter 8. Notifiable disease reports are received from all U.S. states and territories, but morbidity data from surveillance efforts are not as accurate as mortality data collected by vital statistics registration, for several reasons: (1) state laws mandate disease reporting, but reporting to the CDC is voluntary; (2) not all cases receive care and not all treated cases are reported; and (3) the completeness of reporting varies. Noninfectious chronic diseases, such as diabetes, arthritis, and asthma, are not notifiable. The CDC does coordinate other surveillance systems, such as the Pregnancy Risk Assessment Monitoring System and the Behavioral Risk Factor Surveillance System. These surveillance systems are also ongoing, but data are collected only periodically, and only from samples. In 1973, the National Cancer Institute (NCI) established the Surveillance, Epidemiology, and End Results (SEER) program to provide data on cancer incidence and track patients diagnosed with cancer. SEER contracts with 18 population-based local and state registries that submit cancer data covering approximately 26% of the U.S. population twice a year (NCI, 2011).
Surveys
Because ongoing national surveillance systems result in incomplete data on morbidity and disability, the CDC’s National Center for Health Statistics, the National Institutes of Health, and other agencies periodically conduct a number of large-scale, representative surveys on samples of the total population. Examples include the National Health and Nutrition Examination Survey (NHANES) and the National Survey on Drug Use & Health. Surveys use random samples drawn from multiple geographical areas. NHANES, first conducted in the early 1960s, focuses on chronic disease prevalence and related biophysical measures. A segment on nutrition was added in 1971.
Records
Hospital records, such as patient charts, are no longer often used except when local data are being gathered, because national and state organizations such as the American Hospital Association and the Institute of Medicine now survey hospitals, analyze the data, and provide much information in organized, easily available formats. The CDC’s National Center for Health Statistics also conducts regular surveys to collect data on diseases treated and health care provided, such as the National Ambulatory Medical Care Survey, the National Hospital Discharge Survey, and the National Nursing Home Survey.
Other organizations that routinely use health statistics, such as local health departments, regional planning agencies, and other local and state governmental agencies, are additional data sources.
Table 7-1 shows the breakdown of visits to hospital emergency departments by leading diagnoses for gender and age groups in 2008. Which diagnosis is seen more commonly in girls under 15 years of age than in boys of this age? (You are correct if you identified acute pharyngitis as a leading cause of hospital visits for girls but not boys under 15 years of age.) Are there any diagnoses listed for boys that are not listed for girls? What other interpretations are possible from the data in Table 7-1?
Table 7-1
Visits to Hospital Emergency Departments by Diagnosis: 2008
| Leading Diagnosis | Number (1000) | Rate/1000 Persons1 | Leading Diagnosis | Number (1000) | Rate/1000 Persons1 |
| Men | Women | ||||
| All ages | 56,742 | 388 | All ages | 67,020 | 440 |
| Under 15 years2 | 12,762 | 409 | Under 15 years2 | 10,395 | 348 |
| Acute upper respiratory infections3 | 1,129 | 36 | Acute upper respiratory infections3 | 916 | 31 |
| Otitis media | 826 | 26 | Otitis media | 696 | 23 |
| Open wound of the head | 742 | 24 | Pyrexia of unknown origin | 650 | 22 |
| Pyrexia of unknown origin | 718 | 23 | Contusion with intact skin surfaces | 363 | 12 |
| Contusion with intact skin surfaces | 577 | 18 | Acute pharyngitis | 308 | 10 |
| 15-44 years2 | 23,246 | 379 | 15-44 years2 | 31,763 | 516 |
| Open wound, excluding head | 1,264 | 21 | Abdominal pain | 2,103 | 34 |
| Contusion with intact skin surfaces | 1,186 | 19 | Complications of pregnancy, childbirth, & the puerperium | 1,394 | 23 |
| Cellulitis and abscess | 921 | 15 | Contusion with intact skin surfaces | 1,121 | 18 |
| Chest pain | 869 | 14 | Chest pain | 1,121 | 18 |
| Sprains and strains, excluding ankle & back | 765 | 12 | Spinal disorders | 1,048 | 17 |
| 45-64 years2 | 12,542 | 333 | 45-64 years2 | 13,793 | 346 |
| Chest pain | 786 | 21 | Chest pain | 850 | 21 |
| Open wound, excluding head | 565 | 15 | Abdominal pain | 701 | 18 |
| Spinal disorders | 512 | 14 | Spinal disorders | 512 | 13 |
| Abdominal pain | 452 | 12 | Contusion with intact skin surfaces | 433 | 11 |
| Cellulitis and abscess | 373 | 10 | Cellulitis and abscess | 389 | 10 |
| 65 years & older2 | 8,192 | 511 | 65 years & older2 | 11,069 | 522 |
| Chest pain | 456 | 28 | Chest pain | 628 | 30 |
| Heart disease, excluding ischemic | 442 | 28 | Contusion with intact skin surfaces | 541 | 25 |
| Pneumonia | 356 | 22 | Heart disease, excluding ischemic | 537 | 25 |
| Contusion with intact skin surface | 254 | 16 | Abdominal pain | 459 | 22 |
| Chronic and unspecified bronchitis | 241 | 15 | Urinary tract infection, site not specified | 316 | 15 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree