Chapter 15. Endocrine system III. Hormones and metabolism
Insulin, diabetes mellitus and obesity
At the end of this chapter, the reader should be able to:
• explain the basics of the actions, release and mechanisms of action of insulin
• state the two types of diabetes mellitus
• list the types of insulin available for treating IDDM
• describe how insulin is given by injection and be able to give the standard strength of insulin injections
• explain the basics of monitoring treatment with insulin
• recognize the signs of hypoglycaemia
• describe the use of insulin in special circumstances such as pregnancy and diabetic coma
• list the different types of oral hypoglycaemic agents
• describe the actions of glucagon
• outline the management of patients with obesity, including aspects of diet and lifestyle
The pancreas
The pancreas is a relatively large gland lying across the upper part of the posterior abdominal wall (Fig. 15.1). It produces a number of digestive enzymes that drain into the duodenum and help digestion. Scattered throughout the gland are small collections of tissue known as the islets of Langerhans. These islets contain two important types of cell, called alpha and beta cells. The alpha cells secrete glucagon and the beta cells secrete insulin. Insulin and glucagon are important components of the body’s mechanism for controlling glucose metabolism. D cells produce somatostatin.
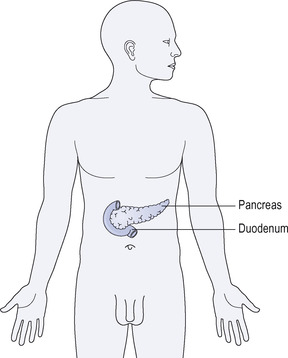 |
| Figure 15.1 Anatomical location of pancreas. |
The normal control of glucose metabolism
Circulating concentrations of glucose are monitored and controlled by the endocrine system. When circulating glucose concentrations rise – for example after a meal – insulin is released from the beta cells of the pancreas into the bloodstream and causes glucose to be taken up into the tissues, where it is converted into energy stores such as liver glycogen and fat or used to generate metabolic energy.
When circulating concentrations of glucose fall, then insulin release is suppressed and other hormones – namely, glucagon, adrenaline, the adrenal glucocorticoids and thyroxine – stimulate the breakdown of fats and glycogen to glucose, which enters the circulation.
Insulin is therefore the only endocrine hormone that is hypoglycaemic: i.e. lowers plasma glucose. Glucagon, adrenaline, the adrenal glucocorticoids and thyroxine are hyperglycaemic. A hormone such as insulin that promotes the conservation of energy and tissue growth is termed anabolic. Hormones that promote the breakdown of tissues to provide energy are termed catabolic.
Insulin
Insulin is a protein hormone whose release from the pancreatic beta cells is stimulated by glucose. It was the first hormone to be discovered and crystallized, and its discovery meant that many thousands of children who would otherwise have died from diabetes could be treated.
Actions of insulin
Insulin lowers the concentration of glucose in the blood by:
• stimulating the uptake of glucose by the tissues
• converting glucose to glycogen in the liver, where it is stored
• increasing the production of fat and protein.
These actions are summarized in Figure 15.2.
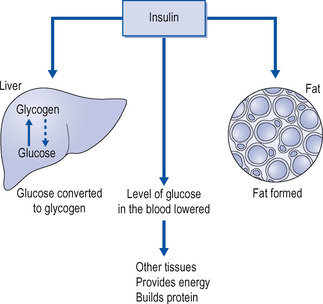 |
| Figure 15.2 The metabolic effects of insulin. |
Release of insulin
Insulin is released from the beta cells when the concentrations of glucose in the blood rise, for example after a meal. A number of other chemical agents – for example, amino acids, carbohydrates and fatty acids – will stimulate insulin release, but the most important insulin releaser for proper maintenance of circulating glucose is glucose itself.
Mechanism of action of insulin
Insulin binds to a specific insulin receptor on cell membranes and this triggers the cell’s response. An important response is the transport of glucose and other sugars away from the blood and into the cell. Glucose is transported into the cell across the cell membrane by so-called glucose transporters, and insulin increases the activity of the glucose transporters.
Diabetes mellitus
The term ‘mellitus’ is derived from the Latin word mel, meaning honey. There is a popular tale that in bygone days doctors diagnosed the disease by tasting the patient’s urine, which tasted sweet because of the glucose in it.
Types of diabetes mellitus
Diabetes mellitus is a disease caused by insulin deficiency. There are two types:
• insulin-dependent diabetes mellitus (IDDM; type I)
• non-insulin-dependent diabetes mellitus (NIDDM; type II).
Insulin-dependent diabetes mellitus
Insulin-dependent diabetes is an autoimmune disease in which the immune system attacks and destroys the beta cells. There is now evidence that a virus, the Coxsackie B4 virus, may cause this form of diabetes in children by infecting the pancreatic islet cells. The disease occurs predominantly in young people. This deficiency leads to a rapid rise in the blood glucose concentration with subsequent loss of large amounts of glucose accompanied by water and salt in the urine. In addition, fats in the body are broken down, releasing ketoacids, which cause acidosis. Protein is also lost and weight loss may be marked. If not treated, the patient will lapse into a coma (hyperglycaemic ketoacidosis). The only treatment is with insulin (see below).
Non-insulin-dependent diabetes mellitus
Non-insulin-dependent diabetes mellitus has traditionally occurred in middle-aged or elderly people who are frequently overweight. An alarming modern development in Western societies, including the UK, is the appearance of obesity and NIDDM in young people, even in some teenagers. This may possibly be due to the large increase in food intake, particularly the eating of fast foods. In some societies, notably among the Native Americans, the situation has become so bad that upwards of 60% of an entire community may suffer from obesity and NIDDM through the ingestion of vast amounts of carbohydrates and fats that are not part of a traditional diet. These people have the added disadvantage of a genetic predisposition to diabetes.
In this type of diabetes there appears to be resistance to the action of insulin coupled with a deficiency of the hormone due to an exhausted pancreas. The blood glucose concentration is raised with glycosuria, but ketoacidosis is less common and the symptoms are often those of the late complications of diabetes, such as infection. The treatment of NIDDM is given below.
Later complications of both type I and type II diabetes mellitus
• Disease of the small arteries leads to damage to the retina of the eye, declining renal function and serious interference with the circulation to the legs, sometimes requiring amputation, and various peripheral nerves may be damaged (peripheral neuropathy).
• Patients with diabetes are particularly prone to infection and these infections may, in turn, exacerbate the diabetes, sometimes leading to ketoacidosis and coma. Good control of the diabetes reduces the severity of the complications but does not entirely prevent them.
Treatment of insulin-dependent diabetes mellitus
Dietary management
Patients with IDDM require insulin replacement to replace the deficiency and a diet suited to their lifestyle and work, to maintain them in good health as judged by their subjective feelings and their weight (which should be kept at the correct level for their age and height) and to keep their blood glucose levels near normal (Fig. 15.3).
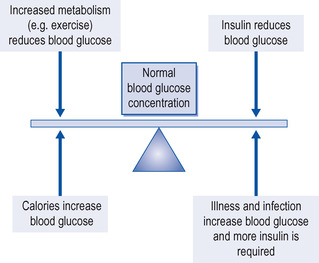 |
| Figure 15.3 Balancing patients with diabetes. |
There are many dietary schemes and, with changing fashions, it is too lengthy a subject to discuss here in detail. Briefly, about 50% of the calories in the normal, healthy diet should be from carbohydrate in forms that are slowly absorbed, such as wholemeal bread, potatoes and other starchy vegetables, but not rapidly digestible sugars such as sweets and cakes. About 35% of the calories may come from fat and the rest from protein.
Because they are at special risk from atheroma, patients with diabetes should avoid foods that have a deleterious effect on plasma lipids. Hypertension, if present, should be treated, exercise encouraged and smoking avoided.
Insulin
Source of insulin
Insulin is available in many preparations that vary in their duration of action. Previously, insulin was extracted from the pancreas of cows (bovine) or pigs (porcine) and needed extensive purification. It is now possible to produce human insulin, either by modifying porcine insulin or, more usually, by a recombinant method involving bacteria. The code for synthesizing human insulin can be inserted into bacteria ( Escherichia coli), which then multiply and produce human insulin. Virtually all insulin now used is human insulin.
Short-acting insulins (soluble insulins)
These are used for the treatment of diabetic coma (ketoacidosis), to cover operations and illnesses in patients with diabetes, and sometimes in the long-term control of diabetes, combined with longer-acting insulin. They are the only insulins suitable for intravenous injection. Following subcutaneous injection their action starts after about 30 minutes and continues for 8 hours. After intravenous injection, their onset is more rapid, but only lasts for about half an hour: they include Humulin and Human Actrapid.
Insulin lispro and insulin aspart are modified forms of human insulin, which are very rapidly mobilized from the subcutaneous injection site. They act even more quickly than soluble insulin (15 minutes against 30 minutes) and their duration of action is only 4 hours. Their place in the management of diabetes is not settled, but they may be useful, if given immediately before a meal, for controlling the rise in blood sugar and thus mimicking more closely the response of the normal pancreas.
Insulin glulisine is a fast-acting synthetic recombinant insulin analogue differing from human insulin in its amino acid sequence. It is marketed under the trade name Apidra by Sanofi Aventis. It is injected subcutaneously immediately before meals and when necessary after food. When injected subcutaneously, it appears in the blood earlier and at higher concentrations than does human insulin. When used as a meal-time insulin, the dose should be given within 15 minutes before a meal or within 20 minutes after starting a meal.
Intermediate-acting insulins
These insulins act for varying periods, depending on the mix of rapid and slow-acting components. The blood glucose starts to fall in 1–2 hours after injection and this effect continues for 16–24 hours. They are usually given once or twice daily and may be combined with soluble insulin.
Insulin zinc suspension (IZS)
It was found that if insulin was buffered with acetate its action was prolonged, and a further two types of insulin could be prepared: amorphous, in which the particles were small, and a crystalline form with larger particles. The action of amorphous insulin is rapid and short-lived, but that of crystalline insulin is more prolonged. By using a mixture of these insulins, a smooth and prolonged effect can be achieved. Among those available are Human Monotard (30% amorphous, 70% crystalline) and Human Ultratard (crystalline).
Biphasic isophane insulins
Biphasic isophane insulins consist of insulin complexed with protamine. This can then be mixed with varying amounts of soluble insulin to produce an immediate and a longer effect. These include Human Mixtard 30/70 and Humulin M1, M2, M3, M4 (varying proportions of soluble and isophane insulin).
Insulin glargine
Insulin glargine ( Lantus) is a new product. It is a preparation of insulin as an acidic solution that is given subcutaneously once daily at bedtime and forms microcrystals under the skin. The microcrystals dissolve slowly and release insulin into the bloodstream. The onset of action is 1 hour after injection, and full activity is reached within 4–5 hours. This activity is maintained at a constant level for 24 hours. In contrast to insulin zinc suspension ( Lente) and isophane insulin (NPH), insulin glargine produces no significant insulin peaks in the bloodstream. Adverse effects of insulin glargine are similar to those of NPH insulin and include hypoglycaemia, reactions at the injection site, rashes, pruritus and allergic reactions. The incidence of hypoglycaemias is similar to that produced by NPH insulin. Insulin glargine has been claimed to produce less nocturnal hypoglycaemia than does once-daily NPH insulin.
Readers are referred to the company’s literature for more information about the use of this insulin preparation.
Long-acting insulins
Protamine zinc insulin (PZI)
This is produced by adding protamine and zinc to insulin. Its action is prolonged, starting after 6 hours and lasting for 24–30 hours. It is bovine insulin and may give rise to skin rashes and painful lumps at the site of injection. If soluble and PZI insulin are mixed in the syringe before injection, some of the soluble insulin becomes PZI insulin. To minimize this, the soluble insulin should be drawn up first and the mixture of insulins injected immediately.
Human Ultratard
Alternatively, the crystalline form of human insulin zinc suspension ( Human Ultratard) also has a prolonged action and is not immunogenic.
Insulin detemir
This is a recombinant form of long-acting insulin, produced and marketed under the trade name Levemir by Novo Nordisk. This is identical to insulin in amino acid sequence and composition, but has been made more fat-soluble through addition of a fatty-acid moiety to the last amino acid on the end of the B chain. This makes the insulin more slowly absorbed from the fat stores after subcutaneous injection, thereby making it more long-lasting. Also, the fatty-acid addition causes it to be bound to circulating albumin, which holds it in the bloodstream longer.
Choice of insulin
If a patient is satisfactorily controlled on a certain type of insulin, that preparation should usually be continued. Human insulin is the least immunogenic and it should be used in the following circumstances:




• for patients starting treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
