CHAPTER 19 End-of-life decision making for older people
FRAMEWORK
This chapter deals with the increasing issues surrounding end-of-life decision making. As the life trajectory for older people changes, the need for open discussion about their health problems and treatment becomes more critical. Acceptance of the ageing process itself is often not easy so the matter of a good death is even more distressing for some people to consider. The vignette provides an excellent discussion on the need for open dialogue with the older person and their families, whether they are acutely ill or have chronic health problems. How a person wishes to be treated when quality of life is not going to improve, no matter what interventions are put in place, seems essential for person-centred care. The issue of competency is one that must be determined before any decision is made by any person involved in care. [RN, SG]
Introduction
It was not long ago that most people died suddenly, at any age, whereas now most of us in the developed world will die of serious chronic disease after a substantial period of disability, but after having lived a great number of years (Lynn et al 2000). Being able to have input into the process of our dying, whether that be through limiting or refusing interventions or determining how we are to be cared for, raises many ethical, legal and clinical issues. This chapter will examine end-of-life decision making with specific reference to older people who are no longer able to make an autonomous choice about their future care. We will introduce you to Charlie and explore the concerns his story raises to highlight some of the issues involved in end-of-life decision making. A discussion of the challenges of competency/capacity to make decisions will be provided. The final component of this chapter will examine advance care planning as a means by which the autonomous wishes of the older person (or people of any age) can be maintained even when they are no longer competent to actively make their own decisions about future health care. Finally, two advance care planning programs will also be discussed.
End-of-life trajectories for older people
The increase of lifespan has meant that we live longer, but we also live longer with chronic diseases. Australians enjoy one of the highest life expectancies in the world — the combined male and female life expectancy at birth is currently 82 years (World Health Organization [WHO] 2008). This is second only to Japan where the combined male and female life expectancy at birth is 83 years (WHO 2008). However in 2004–05, 77% of Australians had a disease or other health problem that had lasted, or was expected to last, 6 months or more and could be classified as a long-term condition (Australian Institute of Health and Welfare [AIHW] 2008). The two most common causes of death in people aged over 65 years in Australia in 2005 were cancer and cardiovascular disease with respiratory system disease, endocrine diseases and genitourinary diseases making up the other leading causes of mortality (AIHW 2008). According to predictions from the WHO (2008), the three leading causes of death in the world in 2030 will be ischaemic heart disease, cerebrovascular disease (stroke) and chronic obstructive pulmonary disease (COPD), all of which are chronic disease conditions.
An uncomplicated death is becoming rarer as we often live with not one but several chronic diseases (Department of Health and Ageing 2001) for which there can be many treatment or maintenance options that can potentially make health decision making difficult. One in three, or nearly seven million Australians, have one or more chronic diseases (Scott 2008). According to Lynn and Adamson (2003: 6) ‘chronically ill people coming to the end of life ordinarily have multiple diagnoses, none of which may be particularly revealing about aggregate severity of illness’. It has been proposed that the group of people who have a serious, progressive, eventually fatal illness, may follow one of three illness trajectories (Lorenz et al 2008; Lynn & Adamson 2003).
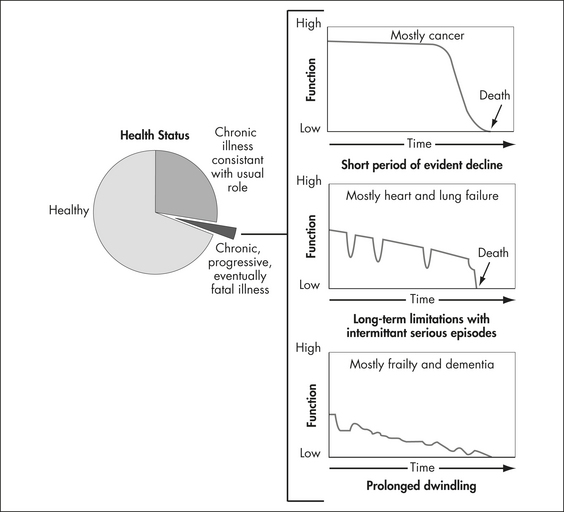
Figure 19.1 Chronic, progressive, eventually fatal illness in the elderly typically follows three trajectories
(Lynn & Adamson 2003: 8)
While it has been argued that a useful way of envisioning care for older people is through classifying them into one of these three categories (Lynn & Adamson 2003), the uncertainty of the trajectories creates a major difficulty in considering end-of-life care and decision making. Unless people have an understanding of their disease and its underlying prognosis, it could be argued that they cannot make informed choices. Prognostic information, according to some commentators (Feldman-Stewart et al 1996; Weissman 2004), is often the most important piece of information that people need when making informed decisions.
People react to a diagnosis of illness and/or simply the changes in old age in different ways. It is the population in the ‘prolonged dwindling’ category that is growing the fastest. For example, it is estimated that by 2031 there will be an increase of 150% from 2006 in the number of older Australians with dementia (AIHW 2008). Less is known about the prognosis of dementia than of other life-threatening diseases (Covinsky & Yaffe 2004; Wolfson et al 2001) but it has been shown to generally have a long lingering decline towards death.
However, despite the uncertainty of illness trajectories and the inaccuracy of prognostication there is recognition that an appropriate end-of-life pathway should encompass the following elements: discussion as the end of life approaches; assessment, care planning and review; coordination of care for individuals; delivery of high quality services in different settings; care in the last days of life; and care after death (Department of Health (NHS) 2008).
VIGNETTE
The nursing staff found it difficult to care for Charlie, especially as he had become totally uncommunicative and just sat with a vacant expression on his face. Many of the staff had known Charlie from when he started dialysis, when he was an avid reader, loved watching documentaries, and was quick to rise to a political debate at any time. The dialysis nurses thought that Charlie could probably feel pain as he pulled away and had to be held down whilst the dialysis needles were being inserted. The nursing staff were compromised in their care for Charlie and felt that dialysis was not in his ‘best interests’. The medical staff, however, did not feel comfortable about withdrawing dialysis and Charlie’s son (Michael), when finally contacted, would not discuss this option. Michael said that his father had made the decision to commence dialysis and that he ‘could’ not authorise the withdrawal of this treatment from Charlie. No advance care planning had ever taken place with Charlie.1 It was decided however, by both Michael and the medical staff, that if Charlie fell over again he would not go to the operating theatre, and that if he got a chest infection intravenous antibiotics would not be given.
Charlie’s experience highlights several issues. Several years previously he had made a decision to undertake a life-sustaining treatment. He had not discussed with anyone whether or not he wanted the therapy to be maintained if he experienced a serious decline in his health status. Charlie had lived independently but then developed dementia, which impaired his decision-making capacity and necessitated his move into supported living accommodation. Increasingly it became apparent to those who provided his dialysis treatment that the continuation of this therapy, especially the way in which it seemed necessary to undertake it,2 was burdensome for Charlie and even painful.
Decision making
Determining who should make decisions about care at the end of life is difficult. There is an expectation, especially from a North American perspective (Wolpe 1998), that autonomy, and therefore support for the right of individuals to make autonomous choices, should trump other ethical considerations when it comes to decision making. During the 20th century there has been increasing demand for control over one’s body and medical destiny, especially in areas such as dying and reproduction (Parker & Cartwright 2005). Enhancing individual choice and supporting one’s involvement in health care decisions has become a central theme of health ethics. This is reliant however on the competent person who is able to make, or has the capacity to participate in, these decisions. Alternatively, it is reliant on processes by which people can protect their autonomous decision making for a time when they themselves are no longer able to explicitly express their wishes. Older people who have a disease such as dementia where there is deteriorating and permanent cognitive impairment, or who have experienced some catastrophic ill health event which renders them temporarily cognitively impaired, may find themselves in a situation where they are no longer able to decide or determine what is in their best interests and what will happen to them. They lack decision-making capacity. According to Sullivan (2005: 96) the issue of competency arises more with older people because:
Competence
Competence is sometimes called ‘mental capacity’. According to Parker and Cartwright (2005: 61) capacity, thought of as the capability to consent, is:
Competency is generally acknowledged as a legal determination while its clinical counterpart is known as ‘decision-making capacity’ (Singer 1992: 1236). In the literature, however, the two terms are often used interchangeably (Biegler & Stewart 2001; Miller & Martin 2000). For the purposes of this discussion both these terms will be taken to have a similar meaning; that is, whether a person is cognitively able to make an informed decision about their health care, and specifically in the context of this chapter, about the care/interventions to be provided (or alternatively not to be provided) towards the end of life. Competency or capacity to make health care decisions go to the heart of the concept of informed consent (Miller & Martin 2000) and decision making.
A decision should not be labelled as irrational just because it is not judged as the right decision by others (Brock & Wartman 1990). Using compliance or non-compliance with the opinion and conclusions of health professionals as the barometer to question competency is an outcome approach. The outcome of the decision has been deemed more important than the process by which the person reached the decision (Caplan 1992). In real life clinical situations, however, when someone reaches a decision that is not commensurate with what the health professionals or family would have decided, then the competency of that person to make that decision has been known to be questioned. However, another approach is to use the person’s status as criteria to determine decision-making capacity; that is, the competent are separated from the incompetent along conventional social lines such as majority age or the existence of an illness (Parker & Cartwright 2005). This approach, like that of only reviewing the outcome, does not look at the content of the decision.
A person is generally presumed to be competent to make decisions and the burden of proof lies with others to prove that they are not. Generally competence means the ability to perform a task (Biegler & Stewart 2001). Therefore the ‘criteria of particular competencies [can] vary from context to context because the criteria are relative to specific tasks’ (Beauchamp & Childress 2001: 70). Whether someone is competent or not depends on the person’s ability to meet the demands of a particular task or situation. Competence or incompetence should be the conclusion about the match or mismatch between the person’s ability and the decision-making demands of the situation that they face; a functional approach (Parker & Cartwright 2005). In the context of health care decisions, competence means being able to consent to, or refuse, medical treatment and make decisions about that treatment. In Charlie’s case, the health care professionals perceived his increasing lack of understanding and insight about the fact he needed to have dialysis if he wanted to continue to live as evidence of cognitive decline and, therefore, an increasing lack of decision-making capacity. The staff determined that this lack of insight was initially demonstrated by his turning away of the ambulance and then later by his removal of the dialysis needles and his inability to sit still while the needles were being inserted. It must be said however that Charlie’s behaviour could also have been an indication of his desire not to continue with dialysis. This was not explicitly explored as a reason for his behaviour.
Health professionals’ judgments of a person’s incompetence may lead to: overriding that person’s decisions; turning to surrogates;3 applying for the appointment of a guardian;4 or seeking involuntary institutionalisation for the person whose competency is questioned. Given these implications, it is therefore important that all factors are considered when a determination of cognitive incompetence is made.
Grisso and Appelbaum (1998) define competence as the ability to reason with relevant information so as to engage in a logical process of weighing treatment/care options whereby the information can be rationally manipulated. Rationality may be defined as ‘the ability to reach conclusions that are logically consistent with the starting premise(s)’ (Biegler & Stewart 2001: 524). Therefore potential irrationality is about the processing of information, not in the content or propositions that are processed. A determination of competency also involves being able express a choice about the treatment options (Grisso & Appelbaum 1998). It could be argued that Charlie was unable to verbally and coherently indicate what cause of treatment/care he desired. However given that his story is true, it must be noted that there was no effort made to try other methods of communication besides the active asking of questions with the expectation that he would, or should, appropriately respond. A lack of ability to express a preference can become apparent in the course of routine attempts to talk with a person (Grisso & Appelbaum 1998).
Medical conditions that can affect a person’s cognitive capacity include mental illness, dementia, and delirium, and an assessment is needed to determine whether any of these are present. Health professionals sometimes perform clinical assessments such as the Mini-Mental State Examination (MMSE)5 dementia ratings or neuro-psychological testing to help determine general competency. These tests, however, are not definitive in their ability to determine whether or not someone is competent to make a specific health care decision. They may, however, be useful screening tools if incompetence is suspected. There is no acceptable ‘gold standard’ test for determining competency to make decisions. While the health professionals suspected that Charlie had dementia, no formal screening was undertaken.
Health care professionals generally have to informally assess a person’s competence during several interactions with them (Parker & Cartwright 2005). According to Biegler and Stewart (2001), the treating doctor is the person best placed to assess a person’s competence as they are likely to know the facts of the case. In particular, they are likely to know whether any of the factors that may impair competency are present (Biegler & Stewart 2001). Moye et al (2006) also recognise that clinical judgment is still the best way to make a capacity determination but admit, however, that it can be unreliable. Parker and Cartwright (2005) advocate a simple, practical method for assessing capacity to make decisions, which could consist of the following steps:
 The increase of lifespan has meant that we live longer with chronic diseases.
The increase of lifespan has meant that we live longer with chronic diseases. It is the population in the ‘prolonged dwindling’ category that is growing the fastest.
It is the population in the ‘prolonged dwindling’ category that is growing the fastest. Enhancing individual choice and supporting one’s involvement in health care decisions has become a central theme of health ethics.
Enhancing individual choice and supporting one’s involvement in health care decisions has become a central theme of health ethics. Competency or capacity to make health care decisions go to the heart of the concept of informed consent.
Competency or capacity to make health care decisions go to the heart of the concept of informed consent.


