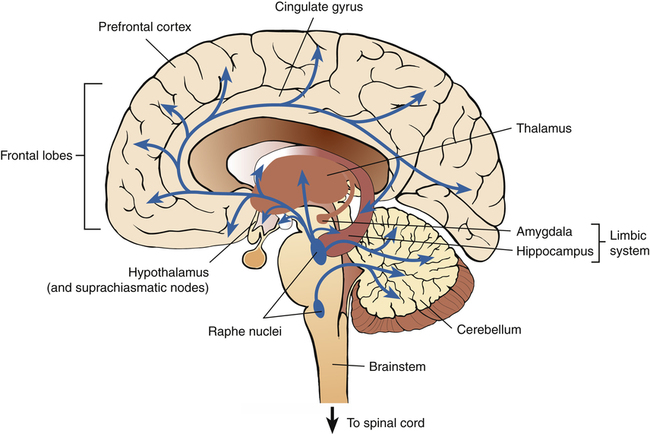
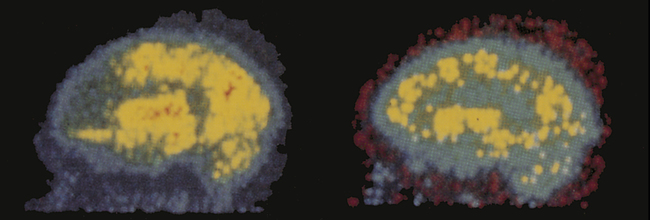
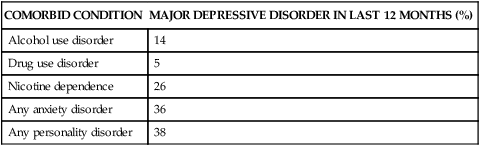
Lying awake, calculating the future, Trying to unweave, unwind, unravel And piece together the past and the future, Between midnight and dawn, when the past is all deception, 1. Describe the continuum of adaptive and maladaptive emotional responses. 2. Identify behaviors associated with emotional responses. 3. Analyze predisposing factors, precipitating stressors, and appraisal of stressors related to emotional responses. 4. Describe coping resources and coping mechanisms related to emotional responses. 5. Formulate nursing diagnoses related to emotional responses. 6. Examine the relationship between nursing diagnoses and medical diagnoses related to emotional responses. 7. Identify expected outcomes and short-term nursing goals related to emotional responses. 8. Develop a patient education plan to enhance social skills. 9. Analyze nursing interventions related to emotional responses. The continuum of emotional responses is shown in Figure 18-1. • At the adaptive end is emotional responsiveness. It implies an openness to and awareness of feelings. In this way, feelings provide us with valuable learning experiences. They are barometers that give us feedback about ourselves and our relationships, and they help us function more effectively. • Also adaptive in the face of stress is an uncomplicated grief reaction. Such a reaction implies that the person is facing the reality of the loss and is immersed in the work of grieving. • A maladaptive response is the suppression of emotions. This may be a denial of one’s feelings or a detachment from them. A temporary suppression of feelings may at times be necessary to cope, as in an initial response to a death or tragedy. • Delayed grief reaction also is maladaptive. It involves a prolonged suppression of emotion that interferes with effective functioning. • The most maladaptive emotional responses are depression and mania seen in bipolar disorder. Severe mood disturbances are recognized by their intensity, pervasiveness, persistence, and interference with social and physiological functioning. • Uncomplicated grief is an adaptive response. It runs a consistent course that is modified by the abruptness of the loss, the person’s preparation for the event, and the significance of the lost object. It is a self-limited process of realization; it makes real the fact of the loss. • Delayed grief reaction is maladaptive. Something is preventing the grief from running its normal course. Persistent absence of any emotion signals a delay in the work of mourning. This delay may occur in the beginning of the mourning process, slow the process once it has begun, or both. The delay and rejection of grief may occasionally last for many years. • Bereavement and loss also can be seen in the maladaptive response of depression. It is an abnormal extension or overelaboration of sadness and grief (Kendler et al, 2008). Depression is the oldest and most common psychiatric illness. The word depression is used in a variety of ways. It can refer to a sign, symptom, syndrome, emotional state, reaction, disease, or clinical entity (Ayuso-Mateos et al, 2010). In this chapter depression is viewed as a clinical disorder that is severe, maladaptive, and incapacitating. Culture affects the symptomatic expression, clinical presentation, and effective treatment of depression (Jang et al, 2010) (Box 18-1). Culture has an effect on the neural systems, psychological states, and interpersonal patterns that exist throughout one’s life, and cultural variations in family and child-rearing practices shape one’s view of the world. Culture provides a release for emotional expression and also can influence one’s source of distress, the form of illness experienced, modes of coping with distress, help-seeking behavior, and social response. There have been changes in attitudes about the causes and treatment of depression among the American public in the past decade. More people now believe in a biological basis for the disorder (Blummer and Marcus, 2009). This may lead to more effective outreach, prevention, and education efforts. Depression often occurs along with other psychiatric illnesses (Table 18-1). Up to 40% of patients with major depressive disorders have histories of one or more nonmood psychiatric disorders that significantly impair their quality of life. These statistics underscore the importance of this health problem and suggest the need for timely diagnosis and treatment. Unfortunately, only one third of all people with depression seek help, are accurately diagnosed, and obtain appropriate treatment (Mojtabai, 2009). TABLE 18-1 COMORBIDITY OF DEPRESSION AND OTHER PSYCHIATRIC ILLNESSES A high incidence of depression is found among all patients hospitalized for medical illnesses. Its intensity and frequency are higher in more severely ill patients (Lin et al, 2010; Fallon, 2011). These depressions are largely unrecognized and untreated by general health care providers. Depressive conditions are highly prevalent in primary care settings. It is one of the most common clinical problems. One of every five patients seeing a primary care practitioner has significant symptoms of depression and one in ten patients meet criteria for major depressive disorder (Halaris, 2011). Yet health care providers fail to diagnose major depression in their patients up to 50% of the time. Given the prevalence and disability associated with depression, the U.S. Preventive Services Task Force (2010) has recommended screening of adults for depression in primary care settings that have systems in place to ensure accurate diagnosis, effective treatment, and responsive follow-up. It is particularly important to screen for depression among women of reproductive age, especially those who have children or plan to become pregnant. This is because major depression during pregnancy can result in negative fetal outcomes, impaired neurocognitive and socioemotional development of the child, and increased risks of mental and medical disorders in the offspring later in life (Bansil et al, 2010). Simply stated, children of depressed mothers suffer. Yet, with appropriate diagnosis, mothers can be successfully treated, with improved functioning in their offspring (Pilowsky et al, 2008). In the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000), the major mood disorders are separated into two groups—bipolar and depressive disorders—based on the involvement of manic and depressive episodes over time. • Major depression may involve a single episode or a recurrent depressive illness but does not include a manic episode. • Bipolar disorder includes one or more manic episodes, with or without a major depressive episode. Bipolar disorders are less common than depressive disorders. It is estimated that 2.6% of the adult population has bipolar disorder (Wieseke et al, 2011). Risk factors are being female and having a family history of bipolar disorder. Most people start showing signs of bipolar disorder in their late teens (average age at onset, 21 years). The data suggest that people younger than 50 years of age are at higher risk of a first attack, whereas those who already have the disorder face increased risk of a recurrent manic or depressive episode as they grow older (Sorrell, 2011). Bipolar disorders are associated with increased premature mortality secondary to general medical illnesses (Roshanaei-Moghaddam and Katon, 2009; Weber et al, 2011). Unhealthy lifestyle, biological factors, adverse medication effects, and disparities in health care are contributing factors. Additional facts about depressive and bipolar disorders are presented in Box 18-2. Behaviors associated with depression include affective, physiological, cognitive, and behavioral responses. Box 18-3 presents the spectrum of possible behaviors. Not all patients experience all of these behaviors. Two subgroups of major depressive disorder deserve special attention. 1. Postpartum blues are brief episodes, lasting 1 to 4 days. They occur in about 50% to 80% of women within 1 to 5 days of delivery. Women have labile mood and tearfulness. Treatment consists of reassurance, social support, adequate sleep, and time to resolve this normal response. 2. Postpartum depression may occur from 2 weeks to 12 months after delivery but usually occurs within 6 months. The risk of postpartum depression is 10% to 15%, but the rate is higher for women with a history of psychiatric disorders. Treatment with medication and psychotherapy is indicated for postpartum depression, because treatment has positive effects on both mother and baby (Meltzer-Brody et al, 2008; Pilowsky et al, 2008). 3. Postpartum psychosis typically begins 2 to 3 days after delivery, with highest risk during the first month. It can be divided into depressed and manic types. The incidence of postpartum psychosis is low, and the prognosis is good for acute postpartum psychosis if it is treated at its onset. Psychiatric hospitalization is usually required to protect the mother and her baby (Friedman et al, 2009). Many patients go on to develop bipolar disorder (Spinelli, 2009). The recurrence rate is 33% to 51%, underscoring the importance of early intervention. The potential for suicide should always be assessed in those with severe mood disturbances. Suicide and other self-destructive behaviors are discussed in detail in Chapter 19. Previous suicide attempts and poor social support indicate risk, however the time spent depressed is a major factor in determining long-term risk of suicide (Holma et al, 2010). This example highlights three important points: 1. Medical illness often involves a loss of function, body part, or appearance; therefore all medically ill patients should be assessed for depression. 2. All people experiencing depression and despair have the potential for suicide; therefore all depressed patients should be assessed for suicide. 3. Nurses should intervene with nursing actions that can be preventive, curative, or rehabilitative, based on the nursing assessment and diagnosis. Manic behavior, the essential feature of bipolar disorder, is a distinct period of intense psychophysiological activation. Some of these behaviors are listed in Box 18-4. The predominant mood is elevated or irritable. It is accompanied by one or more of the following symptoms: hyperactivity, the undertaking of too many activities, lack of judgment in anticipating consequences, pressured speech, flight of ideas, distractibility, inflated self-esteem, and hypersexuality. The person with bipolar illness may exhibit disturbed speech patterns. As mania intensifies, formal and logical speech is replaced by loud, rapid, and confusing language. This is often referred to as pressured speech. As the activated state increases, speech includes numerous plays on words and irrelevancies that can escalate to loose associations and flight of ideas (see Chapter 6). Some of these behaviors are seen in the following clinical example. Both heredity and environment play an important role in severe mood disturbances (Zimmermann et al, 2011). Major depression and bipolar disorder are familial disorders, and their familiarity primarily results from genetic influences. The lifetime risk is 20% for relatives of people with depression and 24% for relatives of people with bipolar disorder. The lifetime risk for mood disorders in the general population is 6%. A person who has an identical (monozygotic) twin with an affective disorder has a two to four times greater risk for the disorder than if the sibling were a fraternal (dizygotic) twin or nontwin. Therefore good evidence exists for the role of genetic factors in mood disorders (Breen et al, 2011; Hamilton, 2011). Poorer maternal and fetal outcomes are associated with maternal depression (Pilowsky et al, 2008; Bansil et al, 2010). This underscores the need for early interventions by nurses for parents experiencing depression and for their children (Horowitz et al, 2009; Connelly et al, 2010). There are three forms of personality organization that could lead to depression (Arieti and Bemporad, 1980). They emphasize the critical importance of self-concept and the patients’ appraisal of their life situation. • One type occurs because the patient has relied on another for self-esteem and personal satisfaction. Clinging, passivity, manipulativeness, and avoidance of conflict are seen, along with a lack of personal goals and a predominant focus on problems. • A second type results when a person realizes that a desired but unrealistic goal may never be accomplished. This person sets unrealistic goals and evaluates them with an all-or-nothing standard. Much time is spent in wishful thinking and introverted searches for meaning. • The third type is seen in people who experience emptiness, hypochondriasis, pettiness in interpersonal relationships, and a harsh, critical attitude toward themselves and others. Their illness appears to be preceded by a severe blow to their self-esteem. Helplessness is a “belief that no one will do anything to aid you.” Hopelessness is a “belief that neither you nor anyone else can do anything.” This theory proposes that it is not trauma that produces depression but the belief that one has no control over important outcomes in life (Seligman, 1975; Abramson et al, 1989). • People who are resistant to depression have high self-efficacy and have experienced mastery in life. Their childhood experiences proved to them that their actions were effective in producing gratification and removing annoyances. • People who are susceptible to depression have low self-efficacy and have had lives without mastery. Their experiences caused them to believe that they were helpless and incapable of influencing their sources of suffering, and they developed no coping responses against failure. The behavioral model views people as being capable of exercising control over their own behavior (Lewinsohn et al, 1979). They do not merely react to external influences; they select, organize, and transform incoming stimuli. Thus people are not viewed as powerless objects controlled by their environments; nor are they absolutely free to do whatever they choose. Rather, people and their environments affect each other. Depression is likely to occur if the following positively reinforcing events are absent: Depression also can occur if the following punishing events are present: Abnormalities are seen in many body systems during a depressive illness, including electrolyte disturbances (especially of sodium and potassium); neurophysiological alterations; dysfunction and faulty regulation of autonomic nervous system activity; adrenocortical, thyroid, and gonadal changes; and neurochemical alterations in the neurotransmitters, especially in the biogenic amines, which act as central nervous system and peripheral neurotransmitters. The biogenic amines include three catecholamines—dopamine, norepinephrine, and epinephrine—as well as serotonin and acetylcholine (Krishnan and Nestler, 2010). Some symptoms of depression that suggest endocrine changes are decreased appetite, weight loss, insomnia, diminished sex drive, gastrointestinal disorders, and variations of mood. Mood changes also have been observed with a variety of endocrine disorders, including Cushing disease, hyperthyroidism, and estrogen therapy (Howland, 2010). Further support for this theory is evident in the high incidence of depression during the postpartum period, when hormonal levels change. • The first is the corticotropin-releasing factor stimulation test, which evaluates the pituitary’s ability to respond to corticotropin-releasing hormone (CRH) and secrete sufficient amounts of adrenocorticotropic hormone (ACTH) to induce normal adrenal activity. • The second is the thyroid-releasing hormone (TRH) infusion test, which assesses the pituitary’s ability to secrete sufficient amounts of thyroid-stimulating hormones (TSHs) to produce normal thyroid activity. Substantial evidence exists for abnormal regulation of the serotonin (5-HT) neurotransmitter system (Figure 18-2). This dysregulation is in the amount or availability of 5-HT, the sensitivity of its receptors in relevant regions of the brain, and its balance with other neurotransmitters and brain chemicals. • MRI studies of depressed patients show a decrease in the size of the hippocampus. This supports the hypothesis that increased levels of stress hormones are associated with damage to the hippocampus (a limbic structure involved in learning and memory). • MRI studies of bipolar patients show that brain structures responsible for human mood are larger. Specifically, the amygdala (the limbic structure responsible for modulating feelings of aggression, anger, love, and shyness) is especially large, perhaps accounting for some of the heightened emotionality and problematic behaviors seen in manic patients. Positron emission tomography (PET) studies of mood disorders show decreased frontal lobe brain metabolism (hypometabolism), which is more pronounced on the left hemisphere in depression and on the right hemisphere in mania. This means that the frontal lobes, which have an important role in intellectual and emotional activities, are not using as much glucose as they should (Figure 18-3). Prefrontal cortex (PFC) hypometabolism affects the function of many brain structures that are connected with the PFC by way of the 5-HT system. These interconnections contribute to the varied symptoms of depression (Table 18-2). Also, the amygdala shows increased blood flow, which is associated with intrusive ruminations in people with severe recurrent depression and a family history of mood disorders. TABLE 18-2 PREFRONTAL CORTEX AND SEROTONIN INTERCONNECTIONS: IMPLICATIONS IN DEPRESSION
Emotional Responses and Mood Disorders
Continuum of Emotional Responses
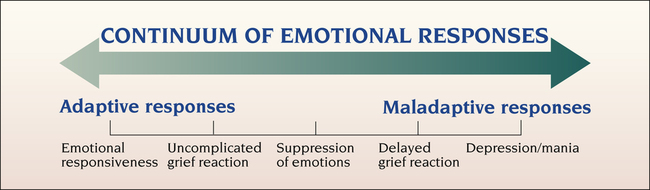
Grief Reactions
Depression
COMORBID CONDITION
MAJOR DEPRESSIVE DISORDER IN LAST 12 MONTHS (%)
Alcohol use disorder
14
Drug use disorder
5
Nicotine dependence
26
Any anxiety disorder
36
Any personality disorder
38
Bipolar Disorder
Assessment
Behaviors
Behaviors Associated With Delayed Grief Reaction
Behaviors Associated With Depression
Postpartum onset
Suicide
Behaviors Associated With Bipolar Disorder
Predisposing Factors
Genetics
Object Loss Theory
Personality Organization Theory
Learned Helplessness-Hopelessness Model
Behavioral Model
Biological Model
Endocrine system
Neurotransmission
Brain imaging
INTERCONNECTED BRAIN STRUCTURES
HYPOTHESIZED ROLE OF THESE INTERCONNECTIONS IN DEPRESSION
Prefrontal Cortex
Covering the frontal lobes, it is unique within the central nervous system (CNS) for its strong interconnections with all other areas of the brain; it receives information that has already been processed by other sensory areas and then merges this information with other emotional, historical, or relevant information, thus attending to both feelings and intellect.
Limbic System Structures
The prefrontal cortex modulates limbic system activities (emotional and instinctive) by way of the following three structures:
Hippocampus
Major importance in cognitive function, including memory
Amygdala
Major importance in modulating feelings such as aggression, anger, love, and shyness
Cingulate gyrus
Involved in motivation and interest
Brainstem
Responsible for regulating the general state of arousal and tone of brain function; also the location of structures that manufacture various neurotransmitters, such as serotonin (5-HT), norepinephrine (NE), and dopamine (DA).
Raphe Nuclei
Located in the brainstem, they manufacture 5-HT; they also modulate excessive stimuli and the organization and coordination of appropriate responses to these stimuli.
Hypothalamus
This interconnection allows for direct prefrontal input into neuroendocrine function by way of the hypothalamic-pituitary axis (HPA).
Suprachiasmatic Nucleus
Located in the hypothalamus, it regulates circadian (24-hour) rhythms and circannual rhythms; thus it is also implicated in seasonal affective disorder (SAD). ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Emotional Responses and Mood Disorders
Get Clinical Tree app for offline access